Figures & data
Figure 1 Jaw N-stretch with vapocoolant spray.
Notes: The patient is instructed to place the tip of the tongue on the roof of the mouth just behind the frontal teeth (like saying the letter “N”) and to open – stretching the mandible while the spray is directed towards the face (masseter muscle region) in an upward motion.

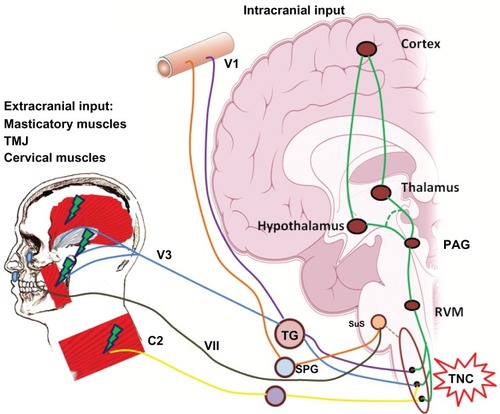
Figure 4 Relationship between temporomandibular disorders and headache.
Notes: Extracranial nociceptive inputs arising from craniofacial structures as a result of a temporomandibular disorder, as well as cervical input from the cervical muscles, may influence the activation of the trigeminovascular system. The commonality is that these nociceptive inputs converge on the TNC in the same way as do intracranial nociceptive inputs arising from the dural blood vessels and higher centers.
Abbreviations: C2, C2 region of the cervical spinal cord; PAG, ventrolateral periaqueductal gray; RVM, rostral ventromedial medulla; SPG, sphenopalatine ganglion; SuS, superior salivatory nucleus; TG, trigeminal ganglion; TMJ, temporomandibular joint; TNC, trigeminal nucleus caudalis; VII, facial nerve; VI, ophthalmic branch of the trigeminal nerve; V3, mandibular branch of the trigeminal nerve.
Abbreviations: C2, C2 region of the cervical spinal cord; PAG, ventrolateral periaqueductal gray; RVM, rostral ventromedial medulla; SPG, sphenopalatine ganglion; SuS, superior salivatory nucleus; TG, trigeminal ganglion; TMJ, temporomandibular joint; TNC, trigeminal nucleus caudalis; VII, facial nerve; VI, ophthalmic branch of the trigeminal nerve; V3, mandibular branch of the trigeminal nerve.