Figures & data
Table 1 Demographic Features of Patients
Figure 1 Illustrative case of a 49-year-old woman with lumbar spinal stenosis (LSS), who underwent initial surgery on the left side and reoperation on the right side. Initial preoperative sagittal computed tomography (CT) (A1), sagittal magnetic resonance imaging (MRI) (A2), axial CT (A3) and axial MRI (A4). Initial postoperative sagittal CT (B1), sagittal MRI (B2), axial CT (B3) and axial MRI (B4). The second postoperative sagittal CT (C1), sagittal MRI (C2), axial CT (C3) and axial MRI (C4). The second postoperative sagittal CT (D1), sagittal MRI (D2), axial CT (D3) and axial MRI (D4). Endoscopy showed that the nerve roots and dura were relatively smooth during the reoperation, without obvious scarring (E1) and decompression completion (E2).
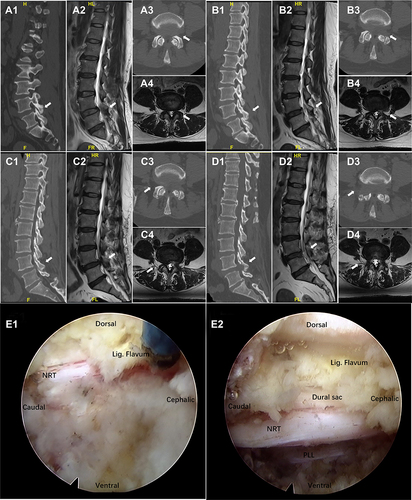
Figure 2 An illustrative case of an 85-year-old woman with lumbar spinal stenosis (LSS) who underwent ipsilateral (right-sided) reoperation. The first preoperative sagittal computed tomography (CT) (A1), sagittal magnetic resonance imaging (MRI) (A2), axial CT (A3) and axial MRI (A4). The second postoperative sagittal CT (B1), sagittal MRI (B2), axial CT (B3) and axial MRI (B4). The second postoperative sagittal CT (C1), sagittal MRI (C2), axial CT (C3) and axial MRI (C4). Endoscopy showed significant scar formation and adhesion of nerve roots and peridural area during resurgery (D1), and completion of decompression (D2).
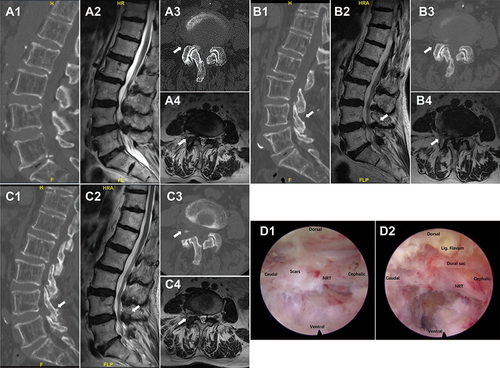
Table 2 Postoperative Modified MacNab Criteria and Outcomes
Table 3 Clinical Outcomes of Percutaneous Endoscopic Lumbar Decompression (PELD) Reoperation
Table 4 Comparation Between Ipsilateral and Contralateral
Table 5 Complications of Percutaneous Endoscopic Lumbar Decompression (PELD) Reoperation
