Figures & data
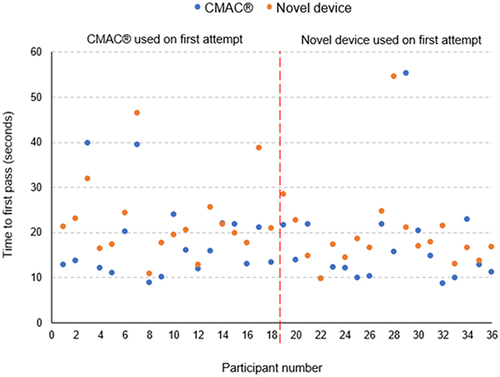
Figure 1 Computer-assisted design model of video laryngoscope blade. (A) Oblique view of the handle. (B) Frontal view of the blade tip. (C) Endotracheal tube cut-away in early design.
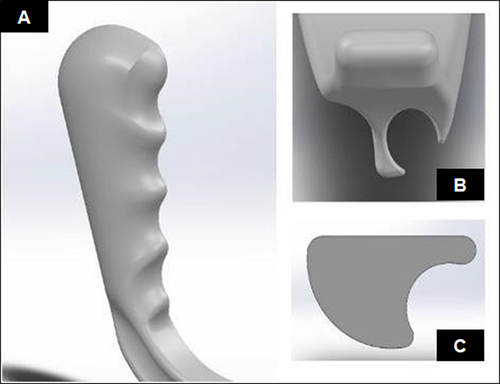
Figure 2 The novel device used in this study. The 3D printed VL blade and handle are attached to a commercially available 6.5 mm borescope camera inserted into a Samsung® Galaxy A11 smartphone.

Figure 3 Diagrammatic presentation of the study process showing sample randomisation. Participants were randomised to either of the two devices for their first attempt at intubation. A videorecording of this attempt was made. Thereafter, the alternative device was used in the same manner.
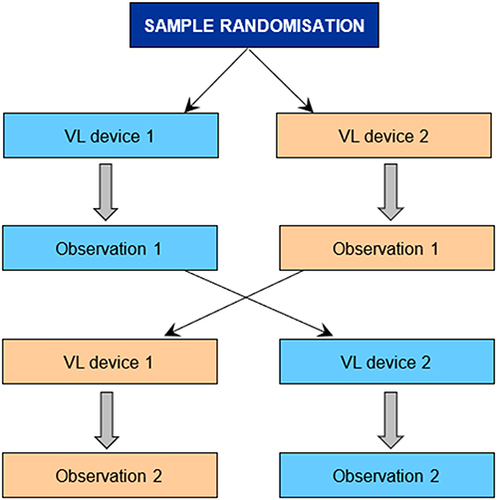
Table 1 Comparative Summary of the Main Outcomes (Time to Seeing Vocal Cords and Time to First Pass) Achieved with the CMAC® Video Laryngoscope and the Novel Device (N=36)
Table 2 Comparative Summary of the Main Outcomes (Time to Seeing Vocal Cords and Time to First Pass) According to Device Use First
Figure 4 Time to first pass of CMAC® and novel device of all participants. The dot chart depicts participants time to first pass using the two different modalities. The vertical axis represents the time to first pass of the endotracheal tube. The blue and orange dots, respectively, represent the time to first pass with the CMAC® and the novel device. The horizontal axis corresponds with each of the participants and their matching attempts. The first 18 participants on the graph used the CMAC® for their first attempt and the second 18 participants used the novel device on their first attempt. Outlying measurements occurred with both modalities. Participant 22 had approximately the same numerical value for both devices, with participants 12 and 35 showing closely similar results.