Figures & data
Figure 1 NLRP3 activation induces the cleavage of pro-Caspase-1, activates the effector protein Caspase-1, shears and activates interleukin (IL)-1β and IL-18, and activates the downstream signaling pathways to produce inflammatory mediators; NLRP3 activation induces microglia to synthesize and release inflammatory mediators, which induce inflammatory responses and ultimately lead to neurotransmitter changes in the brain and depressive-like behaviors. (Blue line) TLR4 is ultimately involved in the neuroinflammatory response by promoting the expression of transcription factors such as nuclear transcription factor-kappa-B (NF-κB) and interferon regulatory factor 3, which, in turn, induce the production and release of inflammatory factors such as IL-1β, IL-6, and tumor necrosis factor (TNF)-α, and also upregulate the expression of proteins such as cyclooxygenase-2. (Orange line) IDO is overactivated and the kynurenine metabolic pathway is enhanced, producing several cytotoxic products that cause neurotoxicity and ultimately lead to neurological disorders such as depression. Inflammatory factors such as interferon-γ, TNF-α, and IL-1 also augment the overexpression of IDO. (Green line).
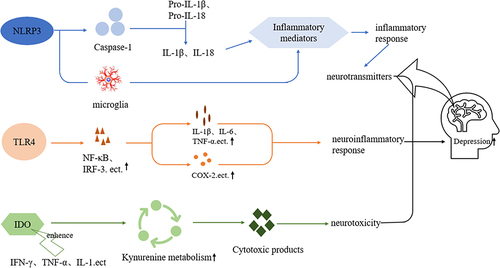
Figure 2 Schematic of the pathogenesis of inflammatory response in depression. Inflammatory response exacerbates abnormal HPA axis function; intestinal flora activates the HPA axis through microbial antigens, prostaglandins, and other mediators, all of which eventually lead to depression (Green line). Inflammatory response decreases the synthesis and thus the levels of monoamine neurotransmitters; some flora in the intestine (anaerobic bacteria, streptococci) can affect the metabolism or synthesis of monoamine neurotransmitters, all of which eventually lead to the onset of depression (Blue line). Inflammatory factors reduce the expression of BDNF and thus its levels, leading to depression (Yellow line). Metabolites of the intestinal flora (short-chain fatty acids, neurotransmitters) enter the brain via blood circulation to aggravate the neuroinflammatory response, and other metabolites activate inflammatory cells to produce inflammatory factors that aggravate the neuroinflammatory response in the brain. The inflammatory factors that are produced in turn lead to an imbalance of the intestinal flora and dysregulation of metabolites (Red line).
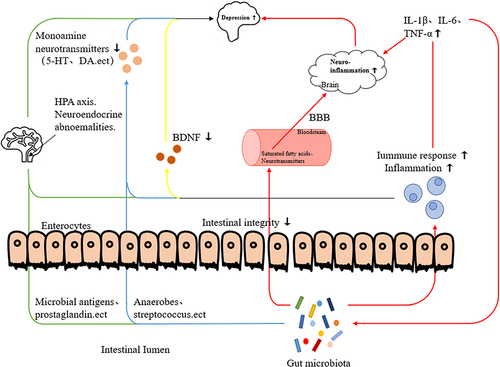
Table 1 Partial List of the Medications Available to Treat Depression
