Figures & data
Figure 1 Preoperative coronal (A) and sagittal (B) computed tomography of the head with the bone algorithm showing a comminuted blowout fracture involving the right orbital floor that approximately measures 0.86 cm × 1.5 cm × 1 cm in maximum orthogonal dimensions, which was associated with fat herniation, inferior rectus muscle entrapment, soft tissue swelling, and intra-orbital gas locules The optic nerve appears unaffected.
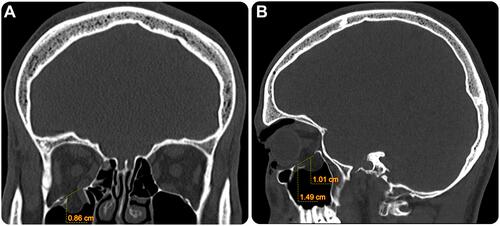
Table 1 Proposed Criteria for Surgical Treatment of Orbital Floor Fractures
Figure 2 Steps for intraoperative custom preparation of polymethyl methacrylate implants. (A) Mixing the PMMA acrylic resin powder with the liquid component (from the set) in a sterile ampoule in a well-ventilated atmosphere. (B) Open the peelable pouch and start emptying the whole contents. (C) Enclose into the sterile foil pouch, ie, plastic sleeves. (D) transfer the plastic sleeves to the sterile surgical area, and when the dough-like material does not adhere to the surgical gloves of the surgeon, the PMMA resin is ready for manipulation. Apply the resin to the osseous defect and remove any excess resin.
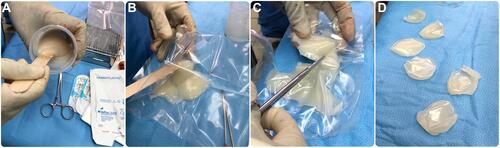
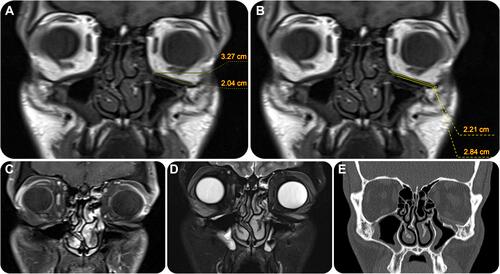
Figure 3 Postoperative follow-up magnetic resonance imaging of the globes. Multi-sequential coronal planar images of the orbit, including plain T1 weighted imaging (A, B); T1-weighted imaging with contrast and fat saturation (C); and T2-weighted imaging (D). These images demonstrate the status after right orbital floor oculoplasty and inferior orbital wall PMMA implant placement (*) with interval complete sealing of the prior fracture. The placed implant measures 1.69 cm × 1.9 cm (A and B) and can be seen covering nearly the entire inferior orbital wall [2.8 cm] (A). The implant is seen subjacent to the inferior rectus muscle with satisfactory attachment to the right inferior orbital wall and adequate fat spacing from extraocular muscles. No significant asymmetry is observed in orbital muscles bilaterally, nor are there signs of an inflammatory process.
![Figure 3 Postoperative follow-up magnetic resonance imaging of the globes. Multi-sequential coronal planar images of the orbit, including plain T1 weighted imaging (A, B); T1-weighted imaging with contrast and fat saturation (C); and T2-weighted imaging (D). These images demonstrate the status after right orbital floor oculoplasty and inferior orbital wall PMMA implant placement (*) with interval complete sealing of the prior fracture. The placed implant measures 1.69 cm × 1.9 cm (A and B) and can be seen covering nearly the entire inferior orbital wall [2.8 cm] (A). The implant is seen subjacent to the inferior rectus muscle with satisfactory attachment to the right inferior orbital wall and adequate fat spacing from extraocular muscles. No significant asymmetry is observed in orbital muscles bilaterally, nor are there signs of an inflammatory process.](/cms/asset/6717df68-be08-414d-ada2-2cbdded91c60/doae_a_12174560_f0003_c.jpg)
Figure 4 Postoperative photographs in the primary gaze (A) and supraduction (B) positions showing significant correction of the inferior sulcus after the BOF and resolving enophthalmos. The patient was followed up for one year and showed no complications.

Figure 5 Preoperative sagittal (A) and coronal (B) computed tomography of the head with the bone algorithm show a displaced fracture of the left lamina papyracea, medial orbit, and displaced BOF of the left inferior orbital wall, which approximately measures 1.4 cm × 2 cm × 1 cm in its maximum orthogonal dimensions. The BOF is associated with a small, displaced bone fragment, abnormal superior orientation of the globe, orbital fat herniation, tethered inferior rectus muscle (*), and proptosis of the eye.
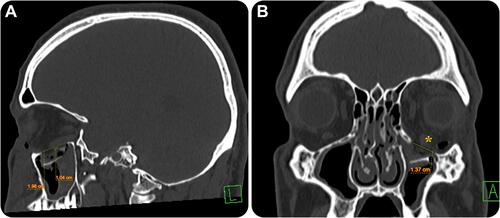
Table 2 A Summary of Commonly Used Synthetic Materials in Oculoplastic Reconstruction2,3
Figure 6 Postoperative follow-up images of the globes, as multi-sequential MR coronal planar images of the orbit including T1 weighted images without (A and B) and T1 weighted images with contrast and fat saturation (C), and T2 weighted images (D) Coronal CT with the bone algorithm (E) showing the status after left orbital floor cranioplasty and inferior orbital wall implant placement for a previous inferior orbital wall displaced fracture, none of which were visualized on follow-up images. The implant measured 2.2 cm × 1.4 cm and covered nearly the entire inferior orbital wall (2.8 cm). The implant is seen subjacent to the inferior rectus muscle with satisfactory attachment to the left inferior orbital wall and adequate fat spacing from extraocular muscles. No significant asymmetry was observed in the orbital muscles bilaterally, nor are there signs of an inflammatory process or implant sliding.