Figures & data
Table 1 Inclusion and exclusion criteria for patients
Table 2 Demographics and surgical characteristics of PDR patients
Figure 1 Vitreous concentrations of MCP-1 (A), IL-6 (B), IL-8 (C), and VEGF (D) in the vitreous samples at the first vitrectomy in PDR patients, and the same vitrectomized PDR patients at the time of the reoperation.
Abbreviations: PDR, proliferative diabetic retinopathy; NS, not significant.
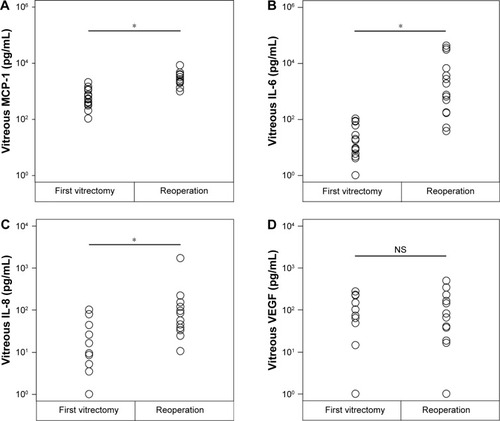
Figure 2 Intravitreous levels of MCP-1, IL-6, IL-8, and VEGF at the time of reoperation vitrectomy and their correlations with the presence or absence of tractional retinal detachment (TRD) due to fibrous proliferation.
Abbreviation: NS, not significant.
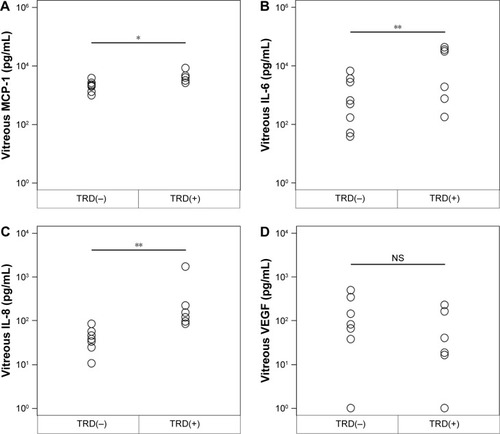
Figure 3 Intravitreous levels of MCP-1, IL-6, IL-8, and VEGF at the time of reoperation vitrectomy and their correlations with the presence or absence of neovascular glaucoma (NVG) and/or anterior hyaloidal fibrovascular proliferation (AHFVP).
Abbreviation: NS, not significant.
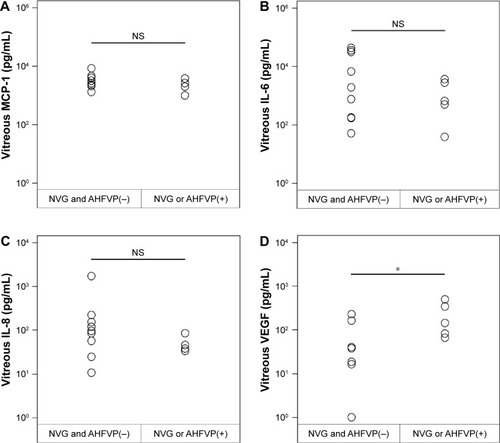
Figure 4 Vitreous concentrations of MCP-1 (A), IL-6 (B), IL-8 (C), and VEGF (D) in patients with an idiopathic epiretinal membrane or a macular hole (nondiabetic controls; n=110), and also eyes with proliferative diabetic retinopathy (PDR; n=129), and proliferative vitreoretinopathy (PVR; n=24).
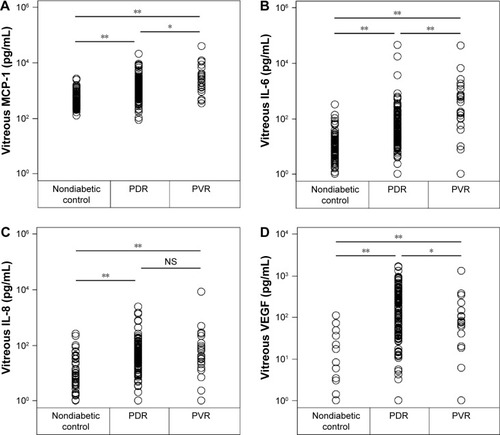
Table 3 Correlations among vitreous concentration of MCP-1, IL-6, IL-8 and VEGF in eyes with proliferative diabetic retinopathy (PDR) and proliferative vitreoretinopathy (PVR)
