Figures & data
Figure 1 Clinical and anterior segment optical coherence tomography (OCT) images of an 80-year-old male with a history of recurrent Salzmann nodular degeneration in both eyes. The individual underwent superficial keratectomy on 3 different occasions – 12, 10, and 4 years prior to presentation – with nodules recurring in both eyes each time. He was subsequently fitted with a prosthetic replacement of the ocular surface ecosystem (PROSE) in both eyes, which improved his visual acuity by 4 lines. He presented with complaints of blurred vision, photophobia, and foreign-body sensation. Given his history of multiple recurrences after superficial keratectomy, he was managed conservatively and refitted for PROSE lenses for both eyes. (A) Slit-lamp photograph of the right eye demonstrating a grayish, subepithelial opacity at eleven o’clock with anterior stromal haze underlying the nodule. (B) Slit-lamp photograph of the right eye demonstrating the hyper-reflective, subepithelial lesion with an arcuate split beam. (C) Cirrus OCT image of the right eye demonstrates a subepithelial lesion (*) with thin overlying epithelium. In this image, there is not a clear separation between the nodule and Bowman’s.
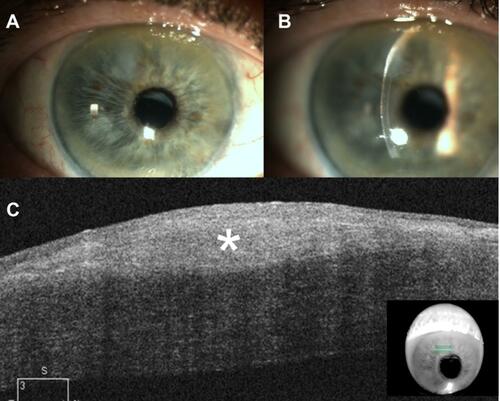
Figure 2 Clinical and anterior segment optical coherence tomography (OCT) images of a 65-year-old male with a history of wet age-related macular degeneration in the right eye who was referred for evaluation of corneal scars. Clinical examination revealed two superior Salzmann lesions in the right eye, which were treated conservatively with ocular surface lubrication. The nodules remained stable for 6 years since initial presentation. (A) Slit-lamp photograph of the right eye demonstrating a white, round-shaped, paracentral corneal opacity between eleven and twelve-o’clock. (B) Heidelberg Spectralis high-resolution OCT demonstrates two distinct hyper-reflective, subepithelial nodules (arrows) with thinned overlying epithelium. In this case, a clear distinction is noted between the nodules and underlying Bowman’s layer.
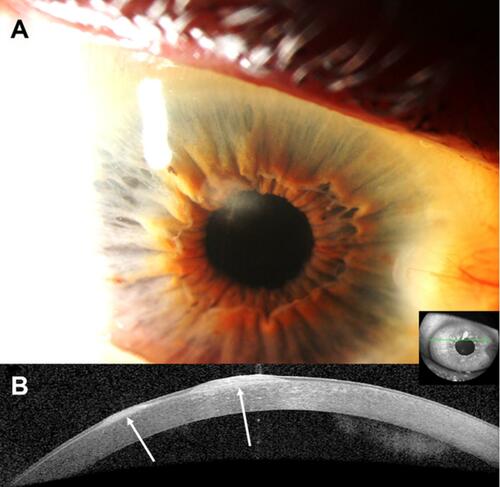
Figure 3 Clinical images of a 58-year-old white male with history of diabetes, cataracts, and trauma to the right eye 40 years prior who presented with Salzmann nodular degeneration in both eyes. Best-corrected visual acuity (BCVA) in the right eye was 20/30 with a correction of −1.25+3.00 x 93. (A) Slit-lamp photograph depicts multifocal, large white-gray corneal opacities in the superior periphery extending centrally. (B) Tomography reveals mildly irregular astigmatism (simK astigmatism 2.0 diopters). (C) 7 weeks after undergoing superficial keratectomy, nodule removal, photokeratectomy, and intra-operative mitomycin-C application, BCVA remained 20/30 but manifest refraction improved to −1.00+0.50 x 95. Tomography reveals improvement in irregular astigmatism (simK astigmatism 0.8 diopters). The patient is now scheduled to undergo cataract extraction.
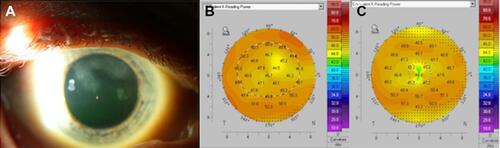
Figure 4 Slit-lamp photographs, anterior segment optical coherence tomography (OCT), and histological images of a 60-year-old white female with a long-standing history of a corneal opacity that was difficult to further subtype by clinical examination alone. (A) Slit-lamp photograph of the right eye demonstrating a whitish-gray, paracentral corneal opacity at eight-o’clock. (B) Heidelberg Spectralis high-resolution OCT image of the right eye depicts a hyper-reflective subepithelial lesion (arrow) with irregularly thinned overlying epithelium. Centrally, Bowman’s layer is intact but is absent peripherally. The classic appearance of the lesion led to a final diagnosis of Salzmann nodular degeneration. (C) Subepithelial fibrocellular tissue with irregular collagen lamellae is present. The overlying epithelium is of variable thickness (Periodic acid Schiff original magnification x400). (D) The subepithelial fibrocellular tissue stains positively for collagen (Gomori’s one step trichrome original magnification x400).
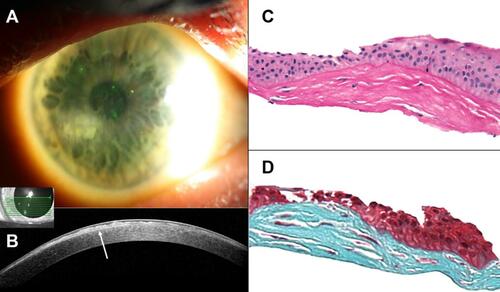
Table 1 Percentage of eyes with recurrent disease following surgical intervention
