Figures & data
Table 1 Preoperative characteristics of the patient (n=854)
Table 2 Combined procedures (n=854)
Table 3 Procedures by study period
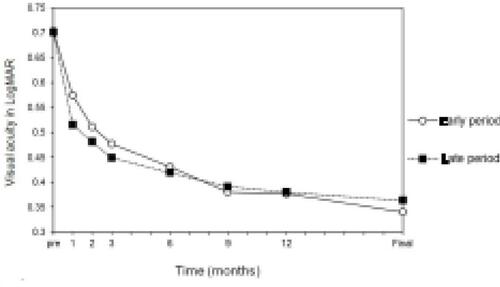
Figure 1 Time course of the changes in the best-corrected visual acuity (BCVA) for the four types of retinal vein occlusions (RVO). The improvement of the BCVA was best in the eyes with branch RVO followed by those with hemi-central RVO (hemi-CRVO), nonischemic central RVO (CRVO), and ischemic CRVO.
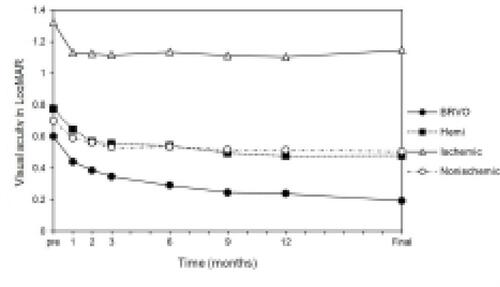
Figure 2 The time course of the changes in the foveal thickness for the four types of RVO. The four types had a similar time course. There was a significant difference between the eyes with a BRVO and ischemic CRVO at preoperatively (P=0.0008).
Abbreviations: RVO, retinal vein occlusion; BRVO, branch RVO; CRVO, central RVO.
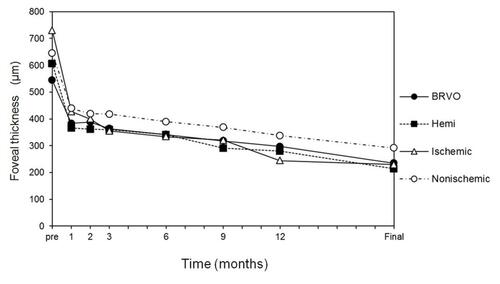
Figure 3 Time course of the changes in the BCVA for the subtypes in BRVO. The improvement is best in the eye with macular RVO followed by second branch RVO, and then by first branch RVO.
Abbreviations: BCVA, best-corrected visual acuity; RVO, retinal vein occlusion; BRVO, branch RVO.
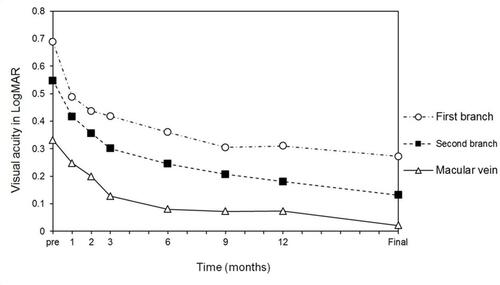
Table 4 Statistical comparison of visual acuity between each time points
Table 5 Visual outcomes at 12 months postoperatively and the final visit
Table 6 Postoperative adverse events (n=854)
Table 7 Postoperative adverse events in acute or chronic eyes (n=854)
Table 8 Additional postoperative surgeries (n=854)
Table 9 Additional postoperative procedures in acute or chronic eyes (n=854)
Table 10 The effects of IVTA on re-occlusion and neovascular glaucoma
Table 11 Multiple regression analyses for re-occlusion
Table 12 Multiple regression analyses for neovascular glaucoma
Table 13 Multiple regression analyses for the final BCVA for the BRVO (n=602)
Table 14 Multiple regression analyses for the final BCVA for the CRVO (n=178)
Figure 4 The time course of the changes in the BCVA for the subgroups of RVO by the acute (duration ≤3 months, n=550) and chronic (duration >3 months, n=304) eyes. The improvement was better in the acute eyes than the chronic eyes. There was a significant difference between two groups at 9 months (P=0.020), at 12 months (P=0.0095), and at the final visit (P=0.012).
Abbreviations: BCVA, best-corrected visual acuity; RVO, retinal vein occlusion; BRVO, branch RVO.
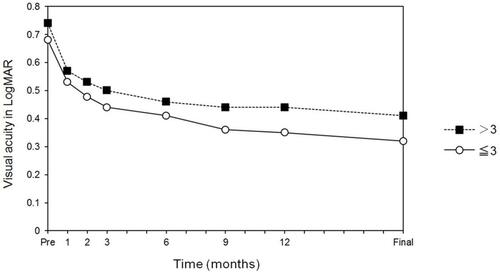
Figure 5 The time course of the changes in the BCVA for the subgroups by the duration of symptoms. There was a significant difference between a duration>6 months and a duration of 2–3 months at 9 months (P=0.0037), at 12 months (P=0.0046), and at the final visit (P=0.0070).
Abbreviation: BCVA, BCVA, best-corrected visual acuity.

Figure 6 The time course of the changes in the BCVA for the subgroups of RVO by the early period (from 9/1994 to 6/2003; n=446) and late period (7/2003 to 11/2011; n=408). There was a significant difference between the two groups at 1 month (P=0.048).
Abbreviations: BCVA, best-corrected visual acuity; RVO, retinal vein occlusion.