Figures & data
Table 1 Patient population.
Figure 1 (A) Setup for high-resolution ocular magnetic resonance (MR) imaging, consisting of a dedicated receive eye-coil, with an integrated mirror. A fixation target is projected onto the screen at the end of the magnet bore. A cued-blinking paradigm is used to minimize blink-induced artefacts. (B) This image demonstrates how the patient's head is positioned within the MRI (magnetic resonance imaging) with the eye coil secured around the head.
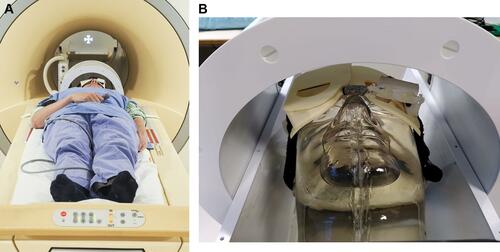
Figure 2 Conventional ultrasound imaging (A) only provides a 2-dimensional cross-section of the tumour, whereas MR (magnetic resonance) imaging (B, C, D) enables a complete 3-dimensional evaluation of the tumour and surrounding structures. Although the original MRI scan (B) is acquired in a transverse direction, the isotropic spatial resolution allows for reformatting in every direction (C, D). To accurately determine the tumour thickness, a reformatting is made which goes through the thickest location of the tumour and is angulated perpendicular to the tumour (blue line in C). On the resulting reformatted scan (D) the tumour thickness can be accurately measured (red arrow).
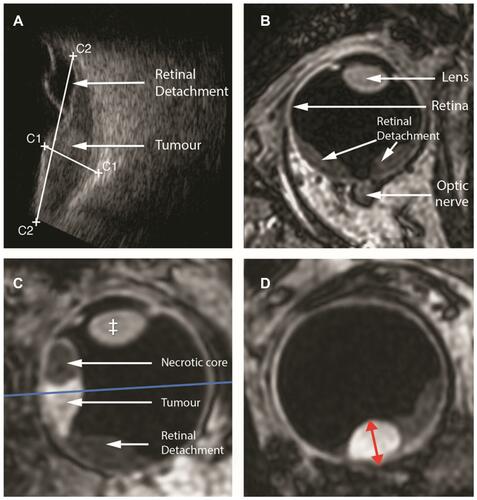
Figure 3 Magnetic resonance (MR) images and ultrasound of a uveal melanoma (UM) with retinal detachment. Sagittal T1 (A), enhanced T1 with fat signal suppression (B) and T2 (C). Ultrasound (US) (D). Notice that the UM enhances (yellow arrow), while the retinal detachment does not enhance (red arrow) and that the outer limit of the sclera is well identified (orange arrow). In comparison with US, the possibility of acquiring multiple sequences and the high soft tissue contrast and high spatial resolution of MRI allow for a better differentiation between tumour and retinal detachment, for a better tumour characterization and better identification of the sclera.
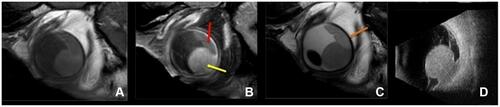
Table 2 Tumours Placed in Different Categories Based on Size, Clinical or Study Groups and a Separate Group for Silicone Oil to Visualise if Treatment Had a Change or Not.
