Figures & data
Table 1 Definitions Used in This Study
Figure 1 Ultra-widefield mapping on angiographic black retinal ischemia. Ultra-widefield fluorescein angiogram (UWF-FA) shows an identifiable “black retinal ischemia” (black-RI) as the nonperfused retina delineated by a water-shed-border. The digital mappings (demarcated borders) of black-RI and optic disc were generated from an Optos-California model of in-built software function, giving a calculation of Angiographic Retinal Ischemic Index (ARI) as the ratio of the black-RI area against the area of the optic disc. UWF-FA also illustrates retinal neovascularization (short arrow) and retinal microvascular anomalies (long arrows) as numerous tiny hyperfluorescent dots sharing the same water-shed border of black-RI.
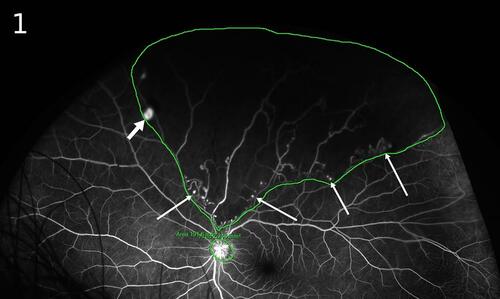
Table 2 Duration of NVE Development and Angiographic Retinal Ischemic Index
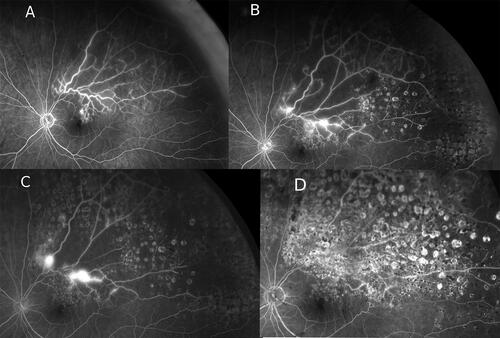
Figure 2 Retinal neovascularizations and angiographic pattern. All the figures (A–D) here are ultra-widefield fluorescein angiograms (UWF-FA) of different patients who had sustained branch retinal vein occlusions. The UWF-FAs depict a recurring theme of angiographic pattern (3Bs pattern); presence of black retinal ischemia (black-RI), budding of retinal microvascular anomalies (RMAs) originating from the same watershed border of black-RI as retinal neovascularizations (NVEs). (A) (a–b) are UWF-FA phases of a patient showing the sectorial black-RI located in the inferotemporal retina involving inferior macula. Active NVEs are seen as hyperfluorescent spots (short arrows) at early phase of angiogram (2Aa) and classically leak fluorescence profusely at the late phase of angiogram (2Ab). The NVEs arise from the water-shed border of black-RI and in this case, are within the macula region. UWF-FA also depicts numerous tiny hyperfluorescent dots of RMAs (long arrows) in early phase of angiogram (2Aa) at the water-shed border but unlike NVEs, they do not leak profusely at late phase (2Ab). (B) UWF-FA of a different patient with branch retinal vein occlusion, showing residual black-RI from insufficient laser treatment hence leading to the proliferation of NVEs with localized pre-retinal hemorrhage in the inferior macula. Note numerous active NVEs arise from the border of the water-shed border, some arise along the venous border within the black-RI. (C) UWF-FA shows patchy ischemic changes in posterior pole but black-RI is most prominent in the far peripheral retina with numerous sprouting NVEs and RMAs (tiny hyperfluorescent dots, long arrows) at the water-shed border. The largest NVE (short arrow) has already bled with localized pre-retinal hemorrhage. (D) UWF-FA of a patient with superior hemi-retinal vein occlusion. The UWF-FA depicts extensive retina ischemia in the superior hemisphere of retina, the black-RI is most prominent at the far peripheral retina. Numerous active NVEs (short arrows) arise from the watershed border and along venous border within the black-RI. RMAs are seen as fainter tiny fluorescein dots (long arrows) scattered along the water-shed border and within the black-RI.
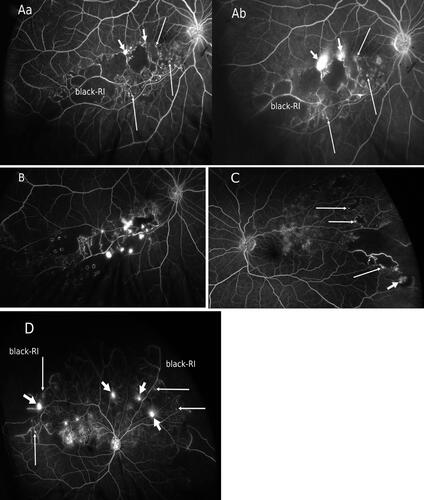
Table 3 Clinical and Ultra-Widefield Angiographic Findings
Figure 3 Retinal ghost vessels and retinal microvascular anomalies. (A) An Optos color image showing a visible network of ghost vessels in the inferotemporal retina and a nearby small retinal microvascular anomaly (RMAs, long arrow) indicating an “old” branch retinal vein occlusion (BRVO). Although the patient’s vision was not affected, a pre-retinal hemorrhage with a visible retinal neovascularization (NVE, short arrow) suggested progression to late complication from a previous untreated BRVO episode. (B) The Optos ultra-widefield fluorescein angiogram (UWF-FA) of the same eye depicting the presence of black retinal ischemia (black-RI) corresponding to the location of the ghost vessels. In addition to outlining the extent of black-RI, UWF-FA is also distinguishing more NVEs (short arrows) and numerous RMAs (long arrows) along the water-shed border of black-RI in comparison to clinical or photographic detection.
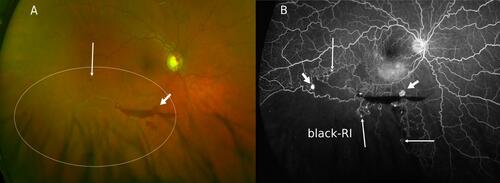
Figure 4 Retinal neovascularizations progression from under-treated retinal ischemia. The patient presented with left eye recurrent vitreous hemorrhage following the diagnosis of a supero-temporal branch retinal vein occlusion (BRVO). Ultra-widefield fluorescein angiograms (UWF-FA) were performed at 5 to 9 months interval showing the course of retinal neovascularizations (NVE) progression over the follow-up period whilst receiving laser treatments. (A) Angiographic “3Bs pattern” was observed with a small NVE developed within the ischemic macula to account for the initial mild vitreous hemorrhage. Target laser photocoagulation was requested on black retinal ischemia (black-RI). (B) Seven months post-laser treatment, multiple new NVEs were seen at different locations, developed from residual inadequately treated black-RI territory. One NVE was at the water-shed border, one was along a major vessel within the black-RI. Further laser treatment was requested. (C) Five months later, the patient presented with further vitreous hemorrhage due to progression of NVE when residual black-RI remained under-treated. (D) Total resolution of all NVEs confirmed from repeated UWF-FA 9 months after the last laser treatment, showing sufficient laser coverage of the entire black-RI area. The patient had no further vitreous hemorrhage and retained excellent vision despite the disease and treatment proximity to fovea.