Figures & data
Figure 1 Active tubercular retinal vasculitis (TRV). Typical fundus appearance of an exudative, hemorrhagic, segmental posterior retinal vasculitis with predominantly venous involvement. Pre-retinal hemorrhage superior-nasal to the optic disc suggests the occlusive nature of vasculitis. This patient had 20/20 Snellen acuity at this time, but macular edema can follow in some patients.
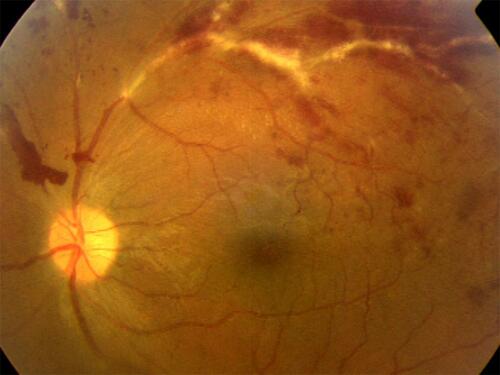
Figure 2 Proliferative stage of TRV. This patient with TRV shows an overlap of inflammatory and proliferative stages of vasculitis: active vasculitis accompanies vitritis, papillitis and vitreous hemorrhage. The key information is that inflammation can directly contribute to neovascularization side-stepping the intervening ischemia.Citation15
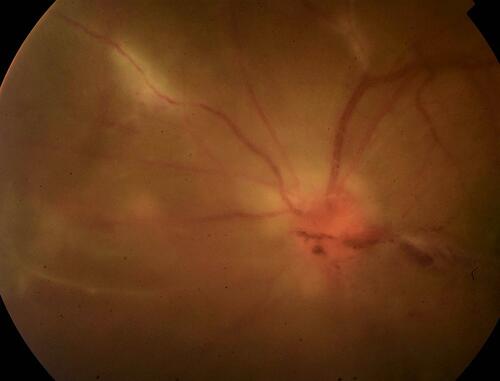
Figure 3 Inactive retinal vasculitis. This patient has 20/20 Snellen acuity with regressed retinal vasculitis with sheathed vessels. Note a chorioretinal atrophic patch with pigment clumps secondary to healed chorioretinitis inferotemporally. There are some collaterals around the temporal vascular arcades indicating compensated retinal ischemia. Such patients need only be observed and counseled for regular follow-ups. Ocular (angiography) or systemic (serologic/radiologic) investigations are not required.
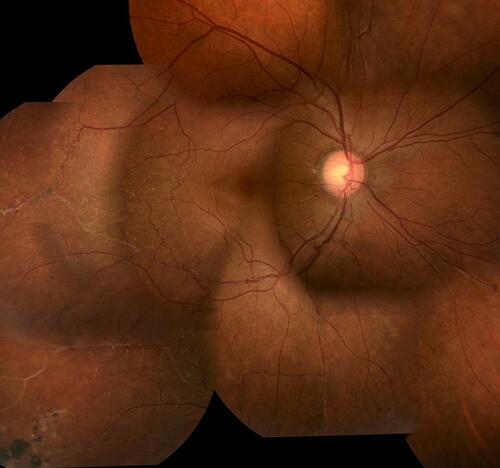
Table 1 Diagnostic Work-up of Tubercular Retinal Vasculitis (TRV)
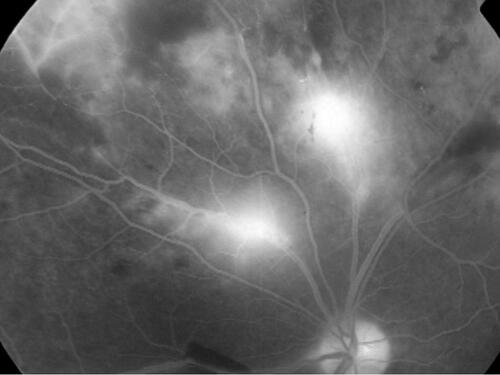
Figure 4 Fluorescein angiography showing inactive TRV. Like (not the same eye), this angiogram shows peripheral capillary non-perfusion in the left upper corner; the blocked fluorescence along the proximal edge of non-perfusion is due to blot hemorrhages and appears darker. Note that the venules draining the capillary dropout are stained, but not leaking: this appearance is suggestive of inactive sheathing, as shown in .
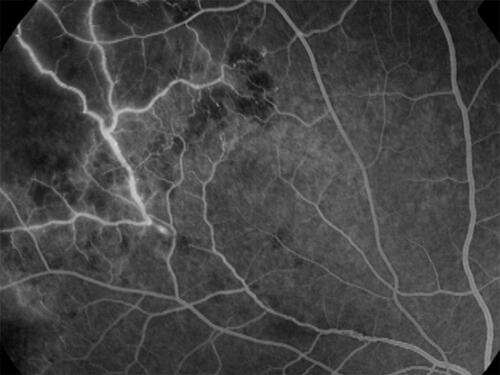
Figure 5 Fluorescein angiography showing active TRV. In contrast to , active vasculitis shows leakage from the vessel wall: more intense from the venules proximal to the optic nerve head, and less intense from the peripheral venule in the left upper corner, but with adjoining capillary nonperfusion. As the active vasculitis regresses, the occlusive phase starts from periphery in the same eye.