Figures & data
Figure 2 (A and B) The front surface of the instrument with 2 markings on the long and short arm respectively for positioning the instrument on the cornea (A). The back surface of the instrument: two tiny prominences at both ends of the long arm of the instrument for marking the insertion and removal site of the suture needle after blue staining (B).Citation8
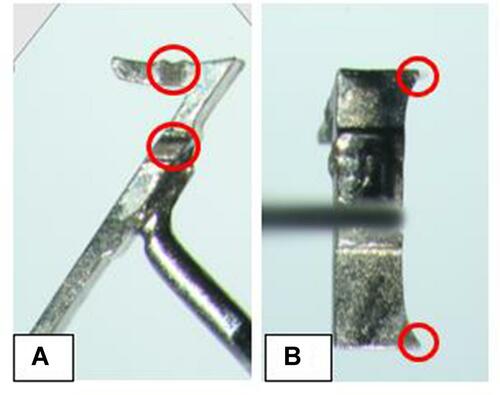
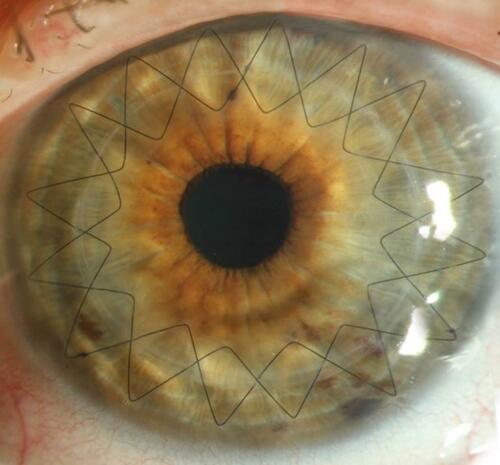
Figure 3 A young surgeon’s first independent continuous cross-stitch keratoplasty in a patient using the Homburg cross-stitch marker. The two sutures are crossing almost everywhere over the interface.Citation8
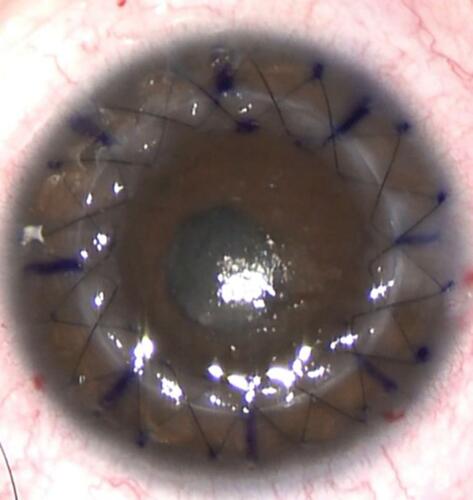
Table 1 Distribution of Indications (n) Between the Two Groups. The Differences Between the Indications Were Not Statistically Significant Between the 2 Groups (P = 0.24)
Table 2 Corrected Distance Visual Acuity (CDVA) (Mean ± Standard Deviation) (Min–Max) in the Two Groups at the Different Follow-Up Time Points After PKP. In Group 2 (with Device), The CDVA Was Significantly Better (P = 0.04, with Bonferroni Correction) Compared to Group 1 (without Device) at 6 Weeks, 10 Months Post Operative and 6 Weeks After the Second Suture Removal
Figure 4 Corrected distance visual acuity (CDVA) (logMAR). There was a statistically significant better visual acuity at 6 weeks, 10 months post operative and 6 weeks after the second suture removal in group 2 (with device) compared to group 1 (without device).
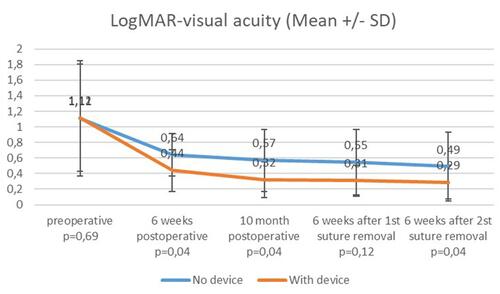
Table 3 Topographic Astigmatism (Mean ± Standard Deviation) (Min–Max) in the Two Groups at Different Time Points After PKP. In Group 2 (with Device), Topographic Astigmatism Was Significantly Lower (P < 0.03 with Bonferroni Correction) at 6 Weeks, 10 Months Post Operative and 6 Weeks After the First Suture Removal Compared to Group 1 (without Device)
Figure 5 Topographic astigmatism. There was a statistically significant lower topographic astigmatism at 6 weeks, 10 months post operative and 6 weeks after the first suture removal in group 2 (with device) compared to group 1 (without device).
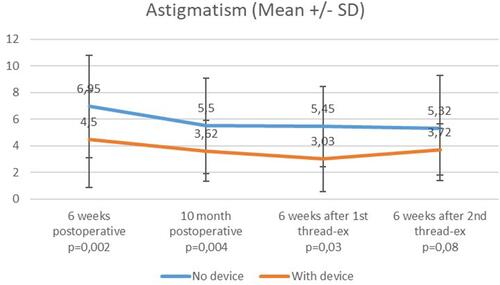
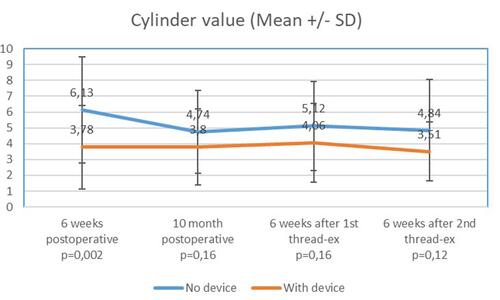
Table 4 Refractive Cylinder (Mean ± Standard Deviation) (Min–Max) in the Two Groups at Different Time Points After PKP. In Group 2 (with Device), The Refractive Cylinder Was Significantly Lower (P = 0.002 with Bonferroni Correction) at 6 Weeks Postoperative Time Point Compared with Group 1 (without Device)
Figure 6 Refractive cylinder. There was a statistically significant lower cylinder value at 6 weeks post operative time point in group 2 (with device) compared to group 1 (without device).