Figures & data
Figure 1 PRP was prepared using a 2-step centrifugation method.Citation18,Citation22 Step 1: 22 mL of blood was drawn into tubes containing 2mL of acid-citrate-dextrose solution A. Step 2: The citrated blood was centrifuged at 1500g for 10 minutes. Step 3: The plasma layer (top) and buffy coat layer (middle) containing platelets were extracted. Step 4: Both layers were centrifuged again at 1500g for 10 minutes. Step 5: The entire platelet-rich pellet (bottom layer) was extracted and resuspended with some platelet-poor plasma (top layer) to create an 11mL PRP suspension. Step 6: PRP suspension was aliquoted into vials for storage.
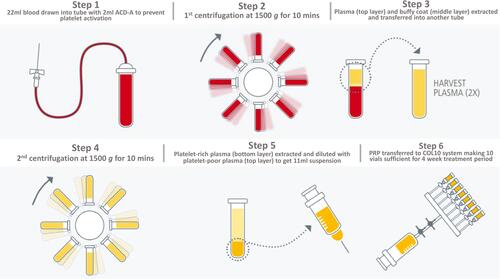
Figure 2 Tear meniscus height (TMH) measurements as generated by the Keratograph 5M. The final TMH is calculated from the average of the TMH measurements at the left, right and center of each eyelid. The final TMH in this eye is 0.36 mm.
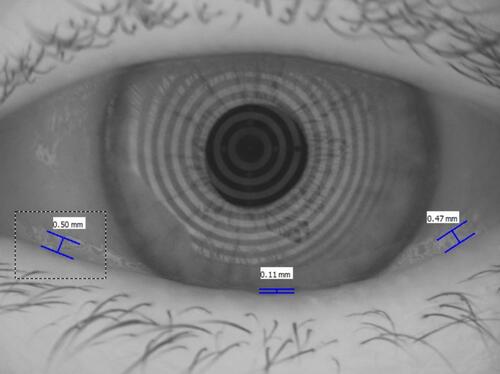
Table 1 Patient Demographics and Baseline Clinical Features
Table 2 Clinical Outcomes with 4 Weeks of Autologous Platelet-Rich Plasma Drops
Figure 3 PRP treatment resulted in significant improvements in patient-reported outcomes as measured by the Canadian dry eye assessment (CDEA, (A)) and patient subjective assessment (PSA, (B)). ***p<0.001.
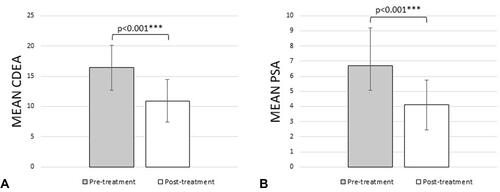
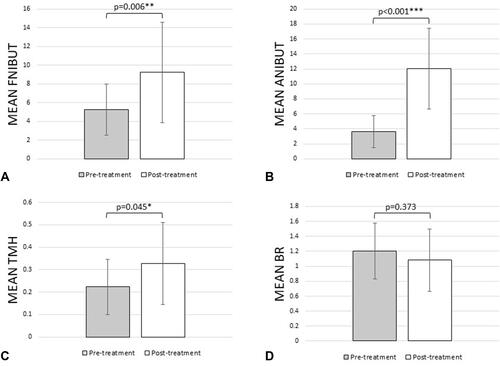
Figure 4 PRP treatment resulted in significant improvements in functional dry eye outcomes as measured by the change in mean first non-invasive break-up time (fNIBUT, (A)), mean average non-invasive break-up time (aNIBUT, (B)), mean tear meniscus height (TMH, (C)), and mean bulbar redness (BR, (D)). *p<0.05, **p<0.005, ***p<0.001.