Figures & data
Figure 1 (A) Optical coherence tomography images of the patient’s right and left maculae at the first visit to the King Khaled Eye Specialist Hospital, Riyadh, Saudi Arabia, showing cystic changes and subretinal fluid in both eyes. (B) Optical coherence tomography images of the maculae after multiple treatments consisting of Avastin® and/or triamcinolone acetonide injections, focal and grid laser. Persistent cystic changes and subretinal fluid are present in both maculae.
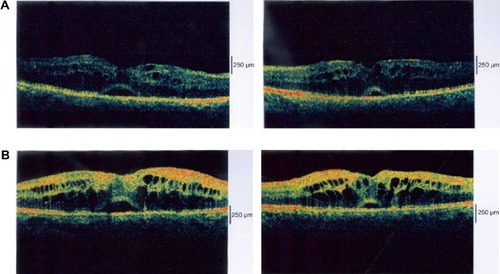
Figure 2 (A) Fluorescein angiographs (left) and photographs (right) of the fundus before and after pars plana vitrectomy and internal membrane peeling, showing improvement in retinal micro- and macro-circulation. (B) Optical coherence tomography image of the macula in bilateral pars plana vitrectomy and internal membrane peeling, showing refractory macular edema.
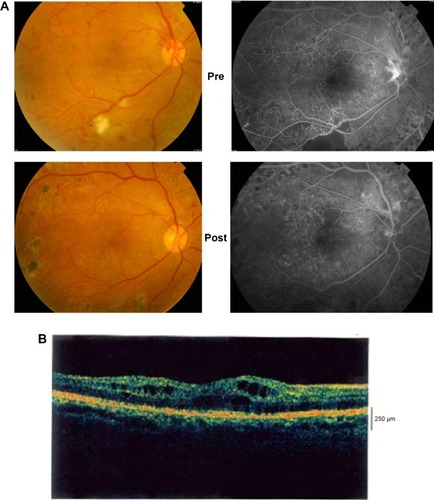
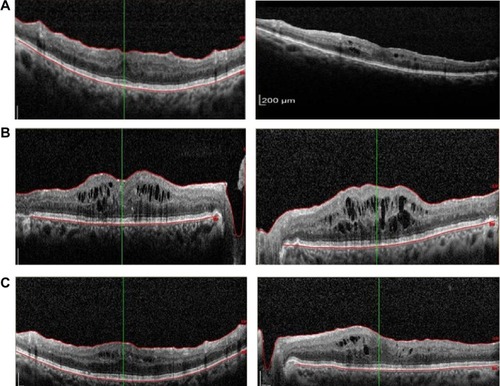
Figure 3 (A) Optical coherence tomography images of both maculae showing marked reduction in the intracellular and subretinal fluid 8 weeks after systemic treatment for diabetic nephropathy. (B) Optical coherence tomography images of both maculae showing recurrent macular edema with the discontinuation of the diuretic and angiotensin-converting enzyme inhibitor medication. (C) Optical coherence tomography images of both maculae 1 month after resuming the diuretic and angiotensin-converting enzyme inhibitor, showing improvement only in the macular edema.