Figures & data
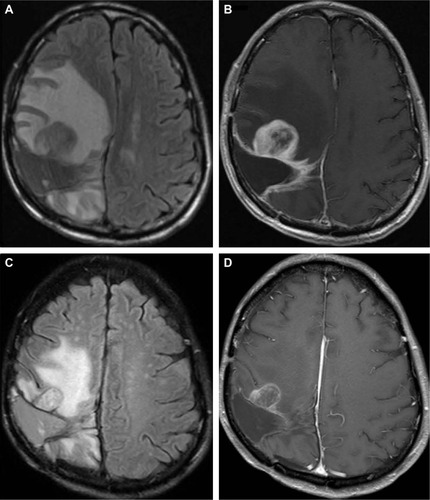
Figure 1 Pre- and postoperative MRI and histopathological diagnosis for patient 1.
Abbreviations: MRI, magnetic resonance imaging; HE, hematoxylin–eosin; WHO, World Health Organization.
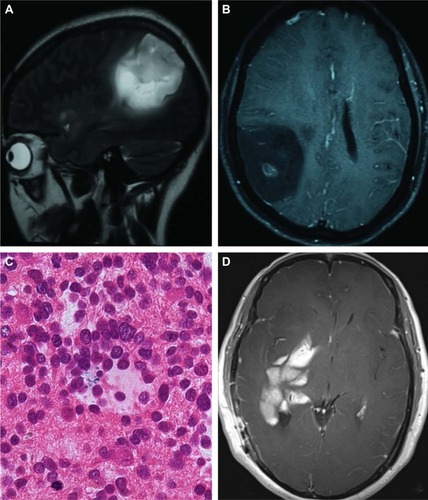
Figure 2 MRI during the second relapse for patient 1.
Abbreviation: MRI, magnetic resonance imaging.
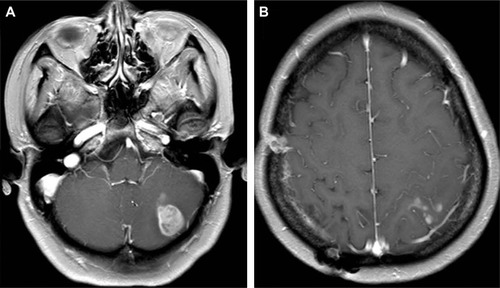
Figure 3 MRI comparison between pre- and post-apatinib for patient 1.
Abbreviations: FLAIR, fluid attenuation inversion recovery; MRI, magnetic resonance imaging.
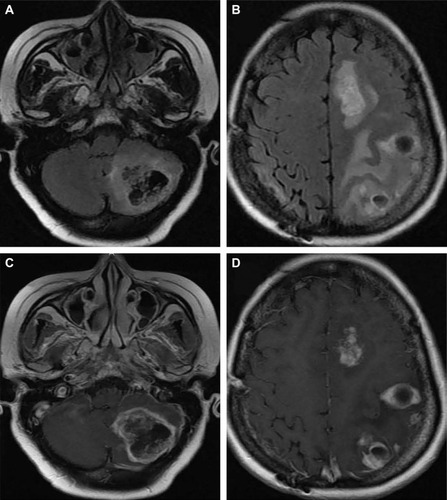
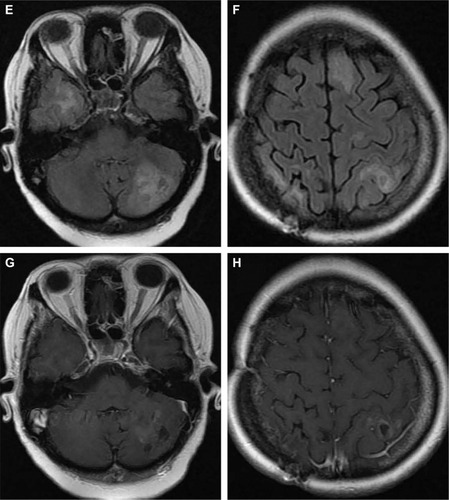
Figure 4 Pre- and postoperative MRI between the first and second operation and histopathological diagnosis for patient 2.
Abbreviations: MRI, magnetic resonance imaging; HE, hematoxylin–eosin; WHO, World Health Organization.
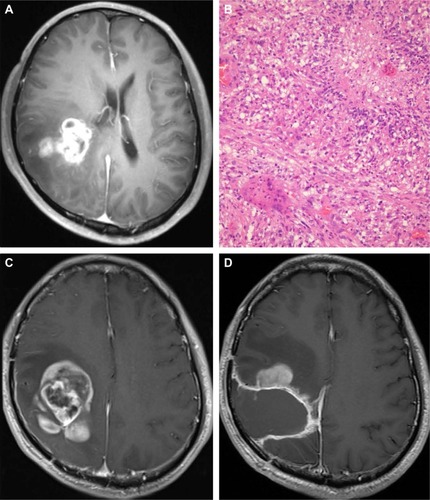
Figure 5 MRI comparison between pre- and post-apatinib for patient 2.
Abbreviations: MRI, magnetic resonance imaging; FLAIR, fluid attenuated inversion recovery.