Figures & data
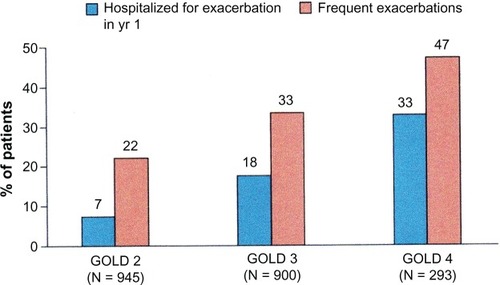
Figure 1 The EPR 3 recommended approach to asthma severity categorization for asthma patients 12 years of age and older is complex.
Abbreviation: EPR 3, Expert Panel Report III.
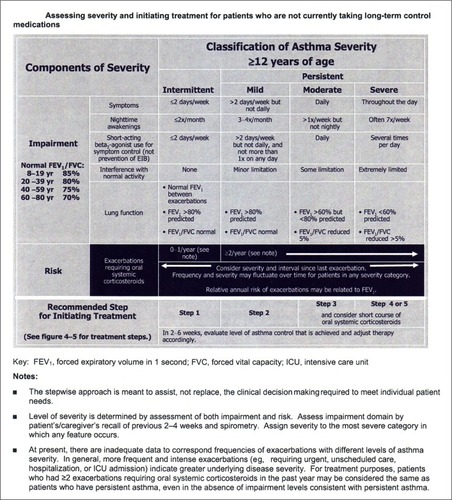
Figure 2 (A) A normal bronchial biopsy from a patient without asthma compared with (B) a bronchial biopsy specimen from a patient with a history of asthma but in complete remission demonstrates epithelial shedding and extensive presence of α-major basic protein.
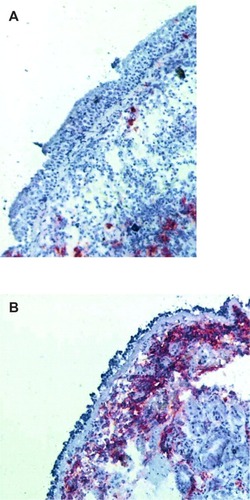
Figure 3 (A) Cumulative severe exacerbations were significantly reduced when asthma treatment was determined by induced sputum eosinophilia used in conjunction with guideline methods (sputum management group) than guideline methods alone (BTS management group).Citation33 (B) The cumulative incidence of mild first exacerbations was significantly lower when asthma therapy was adjusted based on methacholine testing used along with guideline methods (AHR-strategy) than guideline methods alone (Reference-strategy).Citation34
Abbreviations: AHR, airway hyperresponsiveness; BTS, British Thoracic Society.
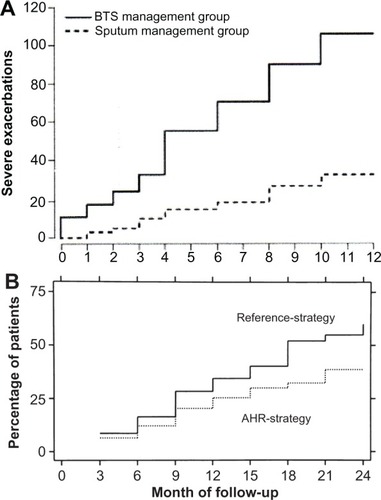
Figure 4 The horizontal red line indicates the fixed FEV1/FVC ratio of 0.70. The black circles above this line represent patients without COPD. The predicted normal post-bronchodilator FEV1/FVC ratio decreases with age. The black diagonal line represents the age-adjusted lower limit of normal for the FEV1/FVC for men. The green circles below this line represent patients with COPD. The red circles between the two lines indicate the 558 (16% of the entire cohort of 3473 men studied) symptomatic male current and ex-smokers referred for spirometry testing who would have been incorrectly diagnosed with COPD based on using the fixed threshold rather than the predicted lower limit of normal.Citation88
Abbreviations: COPD, chronic obstructive pulmonary disease; FEV1, forced expiratory volume in one second; FVC, forced vital capacity.
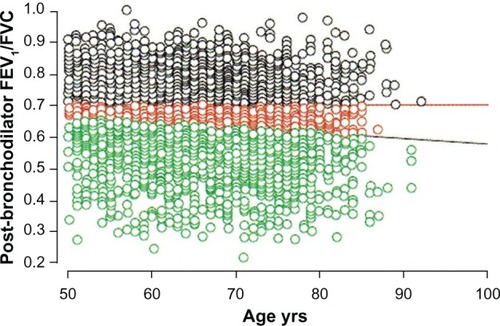
Figure 5 As COPD severity stage increases, the frequency of exacerbations requiring hospitalization increases. The percent of patients with frequent exacerbations (ie, two or more exacerbations per year) also increased with COPD severity stage. In GOLD Stage 2 COPD the exacerbation rates were 0.85 per year. The high exacerbation rate suggests that an algorithm based on claims for COPD exacerbations could be a useful approach to identifying COPD patients in GOLD Stage 2 and above.Citation96
Abbreviations: COPD, chronic obstructive pulmonary disease; GOLD, Global Initiative for Obstructive Lung Disease.