Figures & data
Figure 1 Testicular mass in cryptorchid testis: homogeneous diffuse intratesticular mass lesion with surrounding internal vascularity.
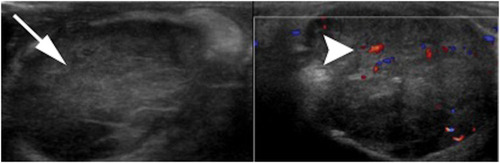
Table 1 WHO Histological Classification of Testis Tumors
Figure 2 Testicular mass in the background of microlithiasis: homogeneous large oval hypoechoic intratesticular mass lesion with surrounding microlithiasis.
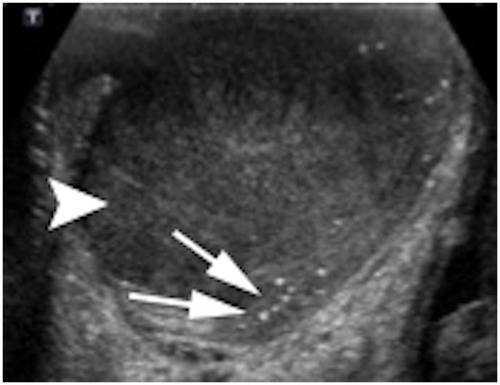
Table 2 Recommended Initial Serological and Radiological Examinations for Staging of Testicular Cancer
Table 3 TNM classification (AJCC eighth edition, 2017)
Table 4 TNM Classification for Testicular Cancer Per Serum Testicular Tumor–Marker Level
Table 5 Stage Groupings of Testicular Germ-Cell Tumors
Table 6 AJCC Staging classification
Table 7 Prognostic-Based Staging System for Metastatic Germ-Cell Cancer
Figure 3 Seminoma: homogeneous large oval intratesticular mass lesion with internal hypervascularity.
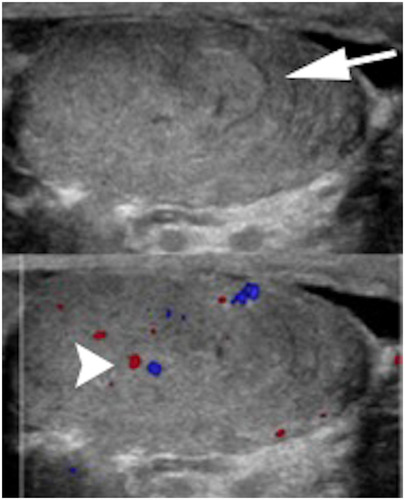
Figure 4 Nonseminomatous GCT: heterogeneous large oval intratesticular mass lesion with internal cystic and calcific changes. The mass also show internal hypervascularity.
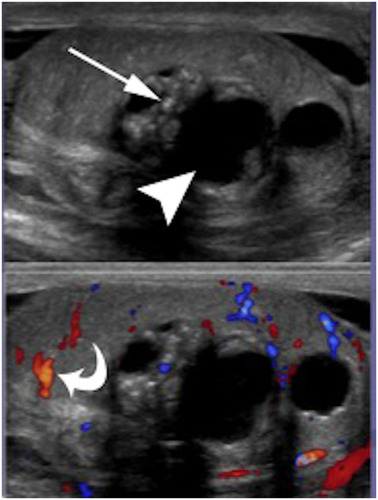
Figure 5 Retroperitoneal metastasis. (A) Left para-aortic lymph node on a patient with left-sided testicular mass. (B) Bilateral large heterogeneous retroperitoneal lymph nodes.
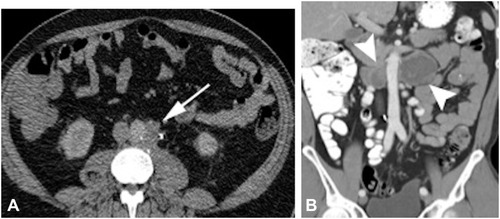
Figure 6 Distant lymph-node metastases. (A) Chest CT soft-tissue window showing subcarinal mediastinal lymphadenopathy with corresponding PET-CT. (B) Increased FDG avidity. (C) Left supraclavicular lymphadenopathy in axial CT with soft-tissue window settings.
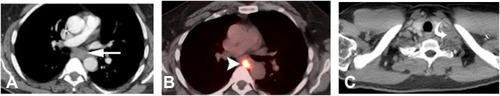
Figure 7 Use of MRI for retroperitoneal spread. Retrocrural heterogeneous T2 intermediate signal intensity LN on right side.

Figure 8 Retroperitoneal metastasis teratoma. (A) Large heterogeneous retroperitoneal mass lesion with internal necrotic and cystic contents. (B) Retroperitoneal spread with vascular invasion involving iliac veins and IVC.
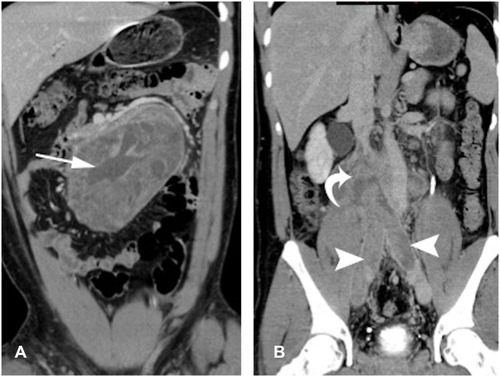
Figure 9 Pulmonary metastases. Same patient as . (A) Chest radiograph showing multiple pulmonary masses and nodules predominantly in bilateral mid-zones. (B) Chest CT lung window settings showing multiple lung nodules in right-middle and left-upper lobes.
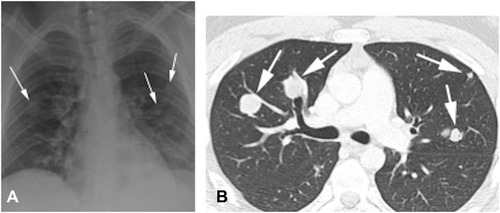
Figure 10 Brain metastases of NSGCT with a patient presenting with headaches. (A) Sagittal T1-weighted postcontrast images showing intra-axial heterogeneous enhancing mass lesion in right occipital region. (B) Axial T2WI Large intra-axial heterogeneous mass lesion with surrounding mass effect and edema, also showing internal darkT2 foci, which could represent hemorrhagic components.
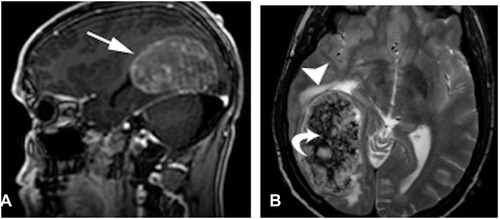
Table 9 Stage I Seminoma Testicular Cancer: Minimum Follow-up Schedule for Postorchiectomy Surveillance, Radiotherapy, or Chemotherapy
Table 8 Stage I Nonseminoma Testicular Cancer: Minimum Follow-up Schedules for Surveillance and Following Retroperitoneal Lymph-Node Dissection or Adjuvant Chemotherapy
Table 10 Advanced (Metastatic) Testicular Cancer: Minimum Follow-up Schedule
Figure 11 Bone metastases of NSGCT in a patient presenting with seminoma and PET-avid osseous metastasis. (A) Pelvic radiography showing geographic lytic lesion involving right superior pubic ramus. (B and C) Axial CT of pelvis showing geographic mass lesion with soft-tissue component involving superior pubic ramus with corresponding increased FDG avidity.
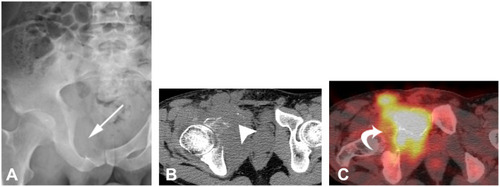
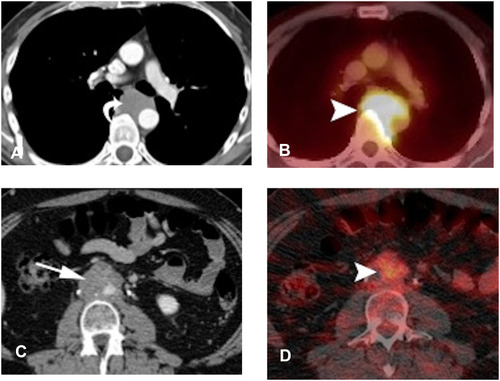
Figure 12 Use of FDG-PETCT in restaging. (A and B) Patient with seminoma showing mediastinal lymphadenopathy with increased FDG avidity. (C and D) Patient with NSGCT showing mildly hypermetabolic retroperitoneal lymph nodes. In both cases, FDG-PET/CT was used for treatment-response monitoring.