Figures & data
Figure 1 The tachogram (A and F), traditional HRV spectrum (B and G), log–log plots of traditional HRV spectra (C and H), power-law function inside the traditional HRV spectra (D and I), and the residual HRV spectra (E and J) of a representative patient with PCA and a representative patient with AMI.
Abbreviations: AMI, acute myocardial infarction; Frq, frequency; HF, high frequency; HRV, heart rate variability; PCA, patent coronary artery; PSD, power spectral density; RRI, RR interval; VLF, very low frequency.
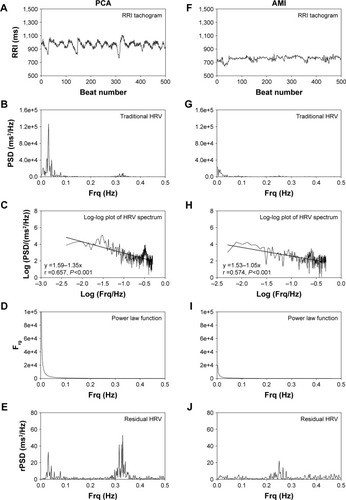
Table 1 Comparison of HRV and rHRV measures between patients with PCA and patients with AMI
Figure 2 The ROC curves with optimal cutpoints for those HRV and rHRV measures the AUC of which is >0.5 in predicting AMI.
Abbreviations: AMI, acute myocardial infarction; AUC, area under the curve; HRV, heart rate variability; nHFP, normalized high-frequency power; nVLFP, normalized very low-frequency power; nrHFP, normalized residual high-frequency power; nrVFLP, normalized very low-frequency power; ROC, receiver operating characteristic; rTP, residual total power; TP, total power.
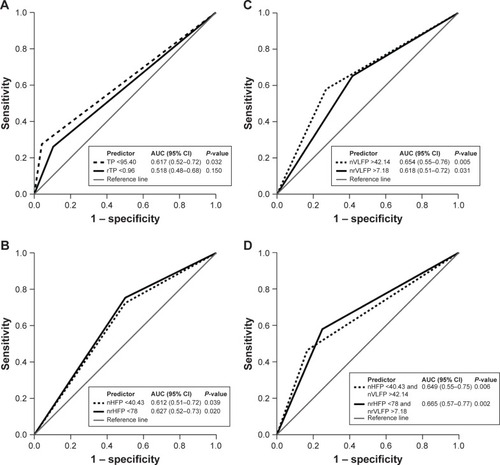
Table 2 The HRV and rHRV measures that have Youden’s cutpoints with an AUC >0.5 in predicting AMI
