Figures & data
Figure 1 The injured ulnar nerve is repaired at the injured site (primary or graft repair), and then the branch of the pronator quadratus muscle is transposed to the deep branch of the ulnar nerve at the wrist level (via end-to-end or end-to-side anastomosis). Red arrows indicate where nerve repair is being performed.
Abbreviations: MN, median nerve; UN, ulnar nerve; AIN, anterior interosseous nerve; PQ, pronator quadratus; PQB, pronator quadratus branch.
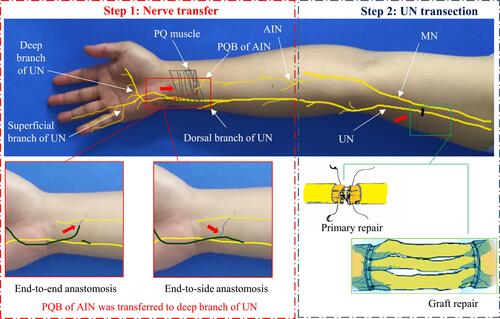
Table 1 Characteristics of Patients with Complete High Ulnar Nerve Injury and Repair
Figure 2 Typical case 1 in group I an 11-year-old male presented with a laceration in the right upper arm. (A) An open wound was observed in the distal upper arm; (B) Complete division of the ulnar nerve in the distal upper arm; (C) Direct fascicular suture of the ulnar nerve injury site; (D) The deep and superficial branches of the ulnar nerve and the anterior interosseous nerve branch of the pronator quadratus muscle were exposed in the wrist incision; (E) The anterior interosseous nerve branch of the pronator quadratus muscle was divided at the farthest distal end; (F) Transfer of the pronator quadratus muscle nerve branch to the ulnar nerve deep branch was performed using end-to-side anastomosis.
Abbreviations: UN, ulnar nerve; AIN, anterior interosseous nerve; PQB, pronator quadratus branch.
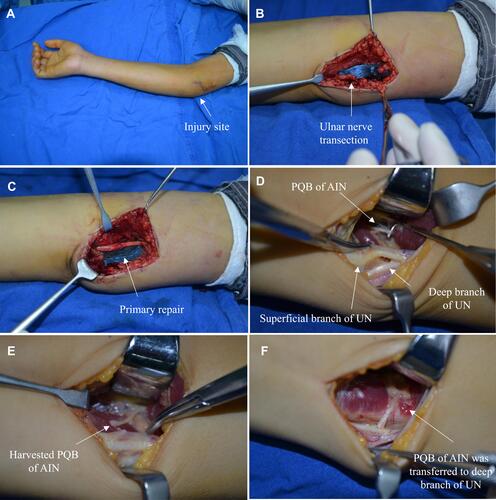
Figure 3 Typical case 2 in group I Direct fascicular suture was performed together with transfer of the nerve branch of the pronator quadratus muscle to the deep branch of the ulnar nerve. (A) An open wound was observed in the distal upper arm; (B) Complete division of the ulnar nerve in the distal upper arm; (C) Direct fascicular suture and repair were performed at the injured site of the ulnar nerve; (D) The deep and superficial branches of the ulnar nerve and the anterior interosseous nerve branch of the pronator quadratus muscle were exposed in the wrist incision; (E) The deep branch of the ulnar nerve was separated non-invasively; (F) The anterior interosseous nerve branch of the pronator quadratus muscle was exposed in the wrist incision; (G) The anterior interosseous nerve branch of the pronator quadratus muscle was divided at the farthest end; (H) Transfer of the pronator quadratus muscle nerve branch to the ulnar nerve deep branch was performed using end-to-end anastomosis; (I–L) Follow-up results after surgery: (I, J) Finger flexion, and extension were normal; (K, L) The function of the intrinsic muscles of the hand was tested by abduction and adduction motions.
Abbreviations: UN, ulnar nerve; AIN, anterior interosseous nerve; PQB, pronator quadratus branch.

Figure 4 Typical case 3 in group I a 19-year-old male presented with a knife cut in the left proximal forearm. Direct fascicular suture was performed in the injured site of the ulnar nerve. Transfer of the pronator quadratus muscle nerve branch to the ulnar nerve deep branch was performed in the wrist. (A) An open wound and complete division of the ulnar nerve were observed in the proximal forearm; (B) Emergency debridement, hemostasis, and closure of the wound were performed; (C) The anterior interosseous nerve branch of the pronator quadratus muscle was exposed in the wrist incision; (D) The deep and superficial branches of the ulnar nerve were exposed in the wrist incision; (E) The anterior interosseous nerve branch of the pronator quadratus muscle was divided at the farthest end, and the deep branch of the ulnar nerve was separated non-invasively and then divided at the proximal end; (F) Transfer of the pronator quadratus muscle nerve branch to the ulnar nerve deep branch was performed using end-to-end anastomosis; (G–K) Follow-up after surgery: (G, H) Finger flexion and extension movements were normal; (I, J) The function of the intrinsic muscles of the hand was tested by abduction and adduction motions; (K) Negative Froment’s sign.
Abbreviations: UN, ulnar nerve; AIN, anterior interosseous nerve; PQB, pronator quadratus branch.
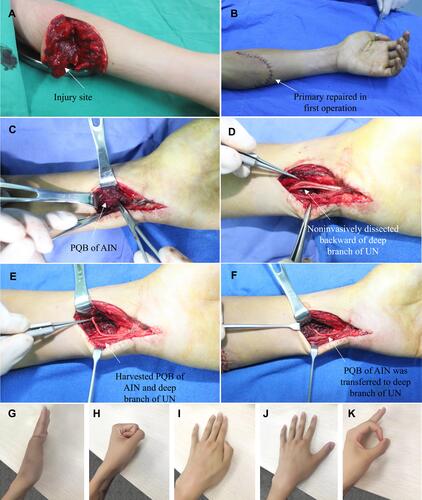
Figure 5 Typical case 4 in group I a 40-year-old male presented with a machinery laceration in the right proximal forearm. (A) An open wound was observed in the distal forearm. Emergency debridement, hemostasis, and closure of the wound were performed; (B) Complete division of the ulnar nerve with an approximate 3-cm defect was noted in the upper third of the forearm; (C) Autologous sural nerve grafting was performed for bridging repair of the ulnar nerve defect; (D) The deep and superficial branches of the ulnar nerve and the anterior interosseous nerve branch of the pronator quadratus muscle were exposed in the wrist incision; (E) The ulnar nerve deep branch was separated retrogradely and non-invasively to the proximal end; (F) Transfer of the pronator quadratus muscle nerve branch to the ulnar nerve deep branch was performed using end-to-end anastomosis; (G–J) Follow-up after surgery: (G, H) The function of the intrinsic muscles of the hand was determined to be normal by abduction and adduction motions of fingers 1–5; (I, J) Finger flexion and extension movements were normal.
Abbreviations: UN, ulnar nerve; AIN, anterior interosseous nerve; PQB, pronator quadratus branch.
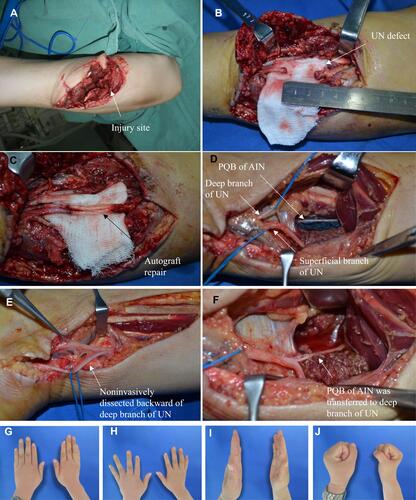
Figure 6 Typical case 5 in group II: Ulnar nerve division was confirmed in the proximal forearm. Only fascicular suture of the injury site of the ulnar nerve was performed; the nerve branch of the pronator quadratus muscle was not transposed to the deep branch of the ulnar nerve at the wrist level. (A) A wound in the proximal forearm; (B) The ulnar nerve was completely divided in the proximal forearm, and the end of the ulnar nerve was retracted. No obvious nerve defect was detected by stretching the nerve; (C) Fascicular suture to repair the ulnar nerve; (D) Primary suture of the wound; (E–H) Follow-up after surgery: (E, G) Obvious atrophy of the first interosseous dorsal muscle and the hypothenar muscles; (F, H) Flexion and extension of fingers were normal.
Abbreviations: UN, ulnar nerve; AIN, anterior interosseous nerve; PQB, pronator quadratus branch.
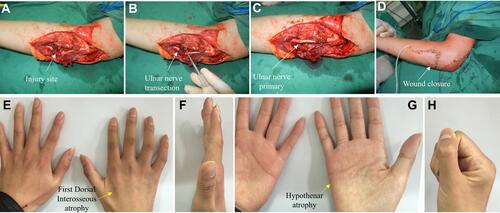
Table 2 MRC Muscle Strength Grading Modified by Brandsma
Table 3 Sensory Nerve Recovery Grading Modified by Mackinnon and Dellon
Figure 7 The results of typical case 1 at the 48-month follow-up. (A–C) Completely normal finger flexion and extension; (D–F) The function of the intrinsic muscles of the hand was determined to be normal by observing abduction motions of fingers 1–5; (F) Froment’s sign was negative, and atrophy of the first interosseous dorsal muscle was not apparent; (G, H) Normal forearm pronation and supination; (I) Flexor muscle strength was scored as level 5; (J) The grip strength of the affected hand (the patient was right-hand dominant) was 35 kg; (K) The pinch strength of the affected hand was 9.5 kg; (L) On the affected side, static two-point discrimination of the fingertips was equal to 6 mm.
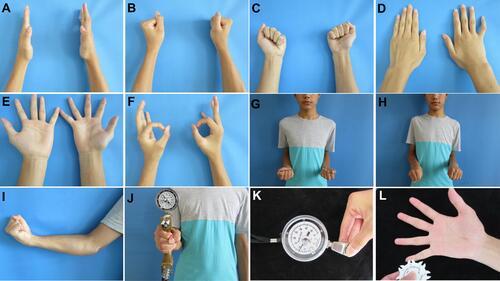
Table 4 Outcome of Patients (Based on the Latest Follow-Up)
Table 5 Outcome of Minority Patients of End-to-Side Anastomosis and Sural Nerve Grafting (Based on the Latest Follow-Up)
