Figures & data
Figure 1 Pre- and postoperative MRI of a 56-year-old male with recurrent LDH who underwent revision PELD. The patient presented with recurrent pain of his low back and left lower extremity 12 months post the primary L5/S1 PELD surgery, but the conservative therapy failed to relieve the recurrent pain. Physical examinations on admission showed numbness involving the inferior aspect of his left foot, 3/5 strength in his left peroneus muscle, and 60° positive left straight leg raise test while the contralateral test proved negative. MRI demonstrated recurrent disc herniation on L5-S1, which was confirmed during the secondary L5/S1 PELD surgery afterwards. The patient had prominent pain relief and functional recovery postoperatively, and postoperative MRI showed decompressed spinal canal and foraminal area.
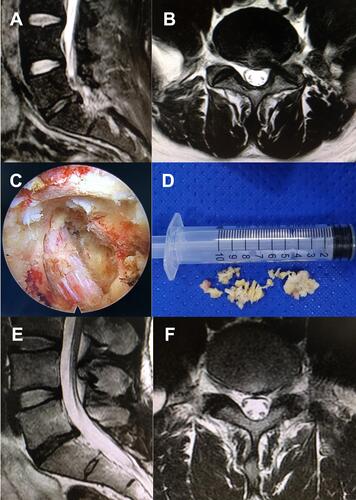
Figure 2 A 52-year-old female diagnosed with recurrent LDH 17 months after primary PELD and underwent revision MIS-TLIF. The patient presented with pain of his low back and left lower extremity that failed to be relieved with conservative therapy. Physical examinations showed 50° positive left straight leg raise test, and MRI demonstrated recurrent disc herniation on L5-S1. She received primary L5/S1 PELD surgery and had prominent pain relief postoperatively. Postoperative MRI at 12 months post primary PELD showed decompressed spinal canal and foraminal area. However, 14 months after the primary operation, the patient started to feel pain of her lower back and right lower extremity. The symptoms aggravated and she detected weakness of her right foot during walking over the next three months, but the effect of conservative treatment including oral analgesics and physical therapy proved to be poor. Physical examinations on admission showed 3/5 strength in her right peroneus muscle. Right straight leg raise test was 40° positive, while the contralateral test was 60° positive. MRI demonstrated recurrent disc herniation on L5-S1. The patient received the revision L5/S1 MIS-TLIF surgery, and she had prominent pain relief and functional recovery postoperatively.
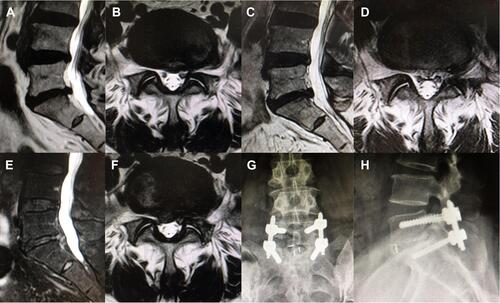
Table 1 Preoperative Data of PELD and MIS-TLIF Groups
Table 2 Perioperative Outcomes, Complications, and Recurrence
Table 3 Clinical Outcomes of PELD and MIS-TLIF Groups
