Figures & data
Figure 1 First-level approach to patients presenting with lymphoproliferation.
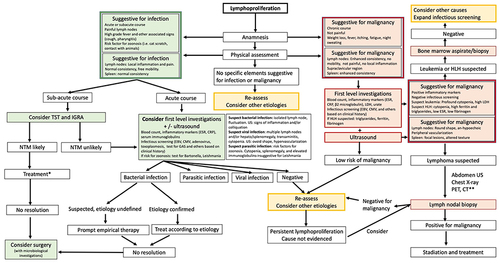
Figure 2 US findings in lymphadenopathies with different etiology.

Figure 3 US findings in splenomegaly with different etiology.
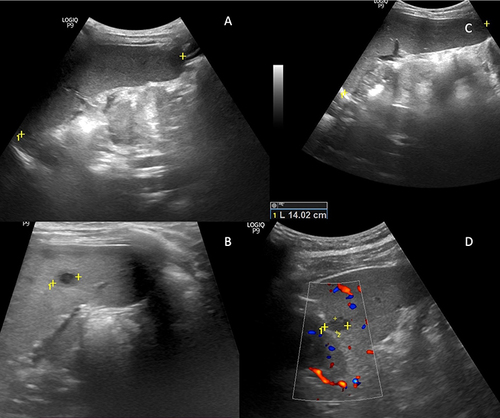
Table 1 Inborn Errors of Immunity Associated with Lymphoproliferation
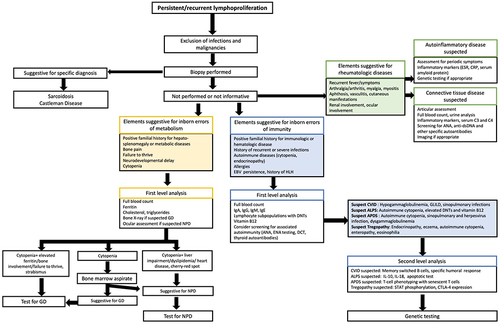
Figure 5 Diagnostic algorithm for the identification of rare causes of lymphoproliferation.