Figures & data
Figure 1 Convergence of Virchow’s triad during pregnancy —endothelial trauma, venous stasis, and hypercoagulability—as well as postpartum. Coagulation is gradually activated to prepare the mother for delivery. The anticoagulant activity of protein S is reduced, and activated protein C resistance rises. A higher concentration of fibrinogen, factors V, IX, X, and VIII, enhances procoagulant activity, leading to increased thrombin production, as demonstrated by an increase in soluble fibrin and prothrombin levels. Reduced fibrinolysis results from increased plasminogen activator inhibitor type 1 and 2 and decreased tissue plasminogen activator (tPA) activity. Endothelial damage to the pelvic vessels results from mechanical stress during normal, induced, or operative vaginal delivery. Venous stasis occurs due to the combination of estrogen-induced venodilation, pelvic venous compression, and compression of the left iliac vein by the right iliac artery.
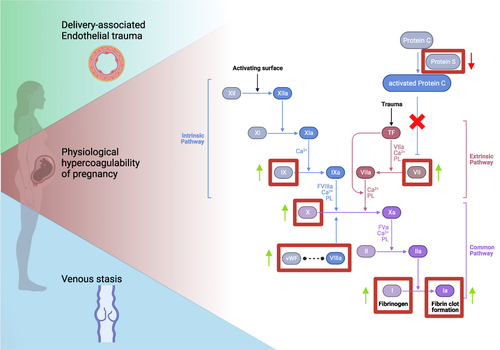
Table 1 Risk Factors Associated with Pregnancy-Associated VTE
Table 2 The Table Shows How the Following Clinical Criteria Would Perform in 1000 Women, of Whom 65 Had PE as per the DiPEP study
Table 3 Diagnostic Accuracy of Presenting Features as Calculated in the Study Population of DiPEP
