Figures & data
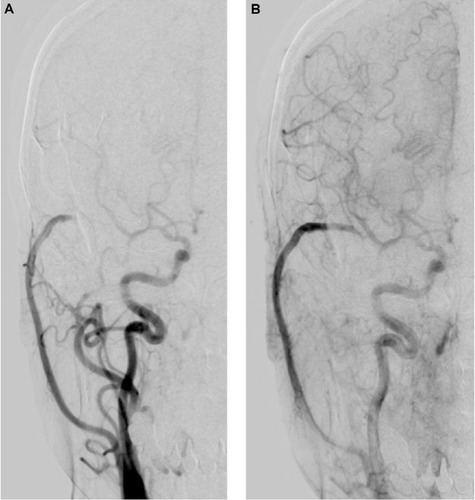
Figure 1 Preoperative computed-tomography angiography demonstrates a ruptured blood blister-like aneurysm (solid-line arrow) in the ophthalmic segment of the right internal carotid artery. The arrow head indicates ophthalmic artery, and the dotted-line arrow indicates the posterior communicating artery.
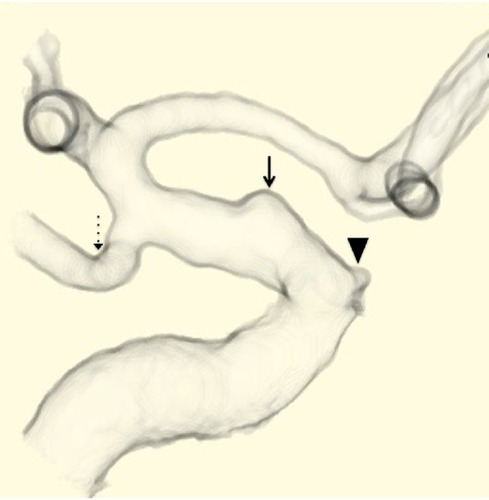
Figure 2 The cortical cerebral blood flow (CoBF) in the frontal lobe decreases immediately after clip-trapping between the area just distal of the origin of the ophthalmic artery and the area just proximal to the origin of the posterior communicating artery, including the ruptured blood blister-like aneurysm (BBA), in the internal carotid artery (ICA). CoBF after clip-trapping decreases by 56% in the right frontal lobe and returns to pre-clamping levels immediately after de-clamping of the ICA.
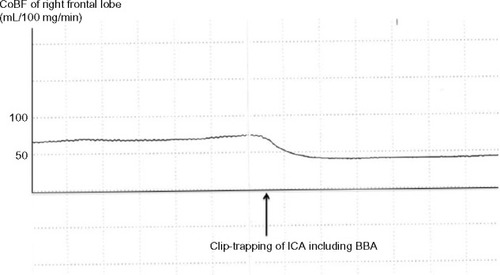
Figure 3 Postoperative right carotid angiogram performed 7 days after surgery demonstrates that (A) the ipsilateral middle cerebral artery (MCA) area is supplied by the patent high-flow bypass during the arterial early phase of angiography; and (B) resolution of the blood blister-like aneurysm and no stenosis in the affected intracranial internal carotid artery (ICA), however, moderate narrowing (arrow) of the proximal segment in the MCA. During the arterial late phase, anterograde filling via the ICA is shown (B).
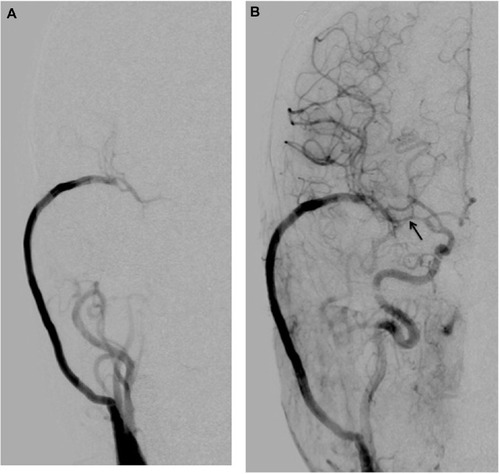
Figure 4 (A) Follow-up right carotid angiogram performed 1 year after the surgery reveals that the ipsilateral middle cerebral artery area is supplied by anterograde filling via the internal carotid artery during the arterial early phase of angiography. (B) During the arterial late phase, retrograde filling via the patent high-flow bypass is shown.