Figures & data
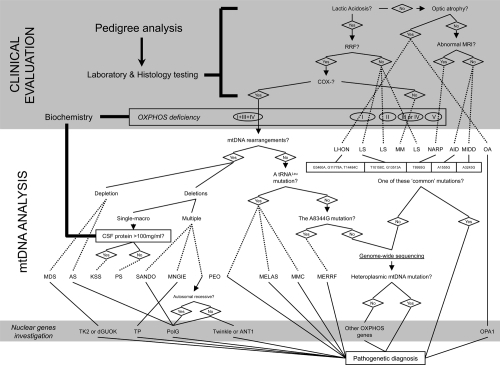
Figure 1 Mitochondrial disease evaluation flowchart, from a clinical suspect to the molecular diagnosis. When a mitochondrial illness is suspected, laboratory testing is the usual method physicians go about evaluating patients for disorders of energy metabolism. If the suspect a mitochondrial defect is confirmed, more integrated tests are a must and include: the biochemical analysis of the respiratory chain and the screening of the most frequent mtDNA mutations. If necessary, sequencing the so-far-known nuclear genes responsible for mitochondrial diseases and the complete sequence analysis of the entire mitochondrial genome are another chances for selected cases. A scattered line states when a diagnosis could be done.
Abbreviations: AID, aminoglycoside-induced deafness; AS, Alper’s Syndrome; COX, Cytochrome c OXidase; CSF, cerebrospinal fluid; KSS, Kearns-Sayre syndrome; PS, Pearson’s syndrome; LHON, Leber’s hereditary optic neuropathy; LS, Leigh’s syndrome; MDS, MtDNA depletion syndrome; MELAS, mitochondrial myopathy, encephalopathy, lactic acidosis, and stroke; MERRF, myoclonus epilepsy with ragged red fibers; MIDD, maternal inherited diabetes and deafness; MM, mitochondrial myopathy; MMC, maternal myopathy and cardiomyopathy; OA, optic atrophy; MNGIE, mitochondrial neurogastrointestinal encephalopathy; MRI, magnetic resonance imaging; NARP, neurogenic weakness, ataxia and retinitis pigmentosa; PEO, progressive external ophthalmoplegia; RRF, ragged red fibers; SANDO, sensory ataxic neuropathy, dysarthria, and ophthalmoparesis.