Figures & data
Figure 1 shows improvement of vision following bevacizumab injection which is maintained up to the end of follow up.
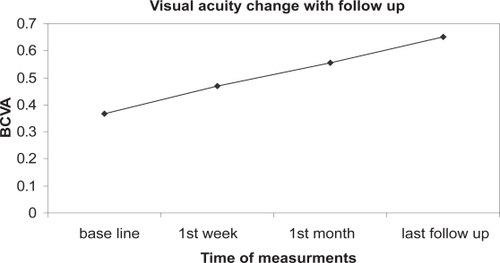
Figure 2 This 53 years old patient presented with dense vitreous hemorrhage obscuring fundus details 4 months after having intensive laser therapy. One month after first bevacizumab injection, (A) Fundus details could be partially seen due to starting absorption of the blood and (B) the angiogram showed NVD. C, One month after second bevacizumab injection, the blood was completely absorbed and the angiogram (D) showed complete regression of the NVD.
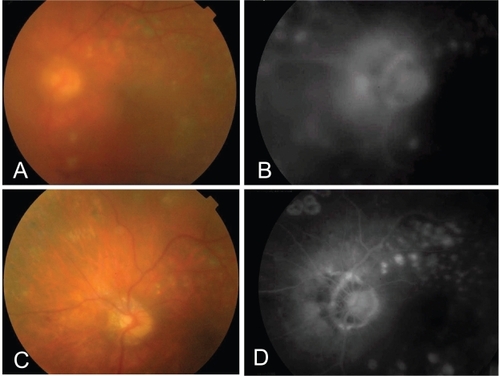
Figure 3 A 40 years old patient with PDR and vitreous hemorrhage (A). B, The fluorescein angiogram showed evident neovascularization at the disc (NVD) with evident nasal ischemia. C, One month following bevacizumab injection there was near complete absorption of vitreous hemorrhage with a fibrous tuft arising from the optic disk (arrow). The macula looks dry with marks of previous grid. The angiogram (D) showed near complete regression of the neovascularization. E, three months following single injection, the angiogram showed evidence of reperfusion of NVD. F, 2 weeks following re-injection, the angiogram showed again complete regression of the NVD.
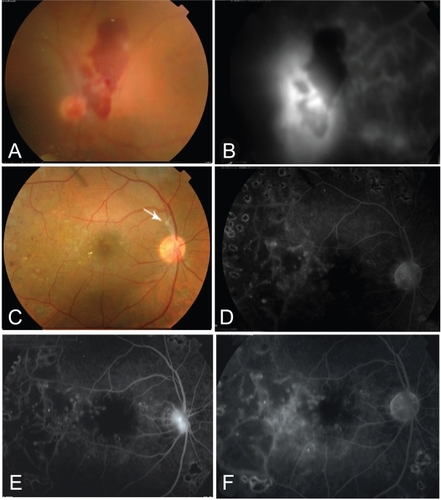
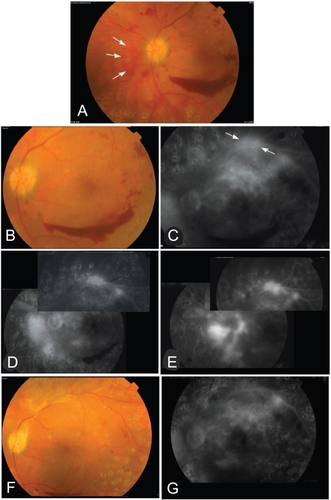
Figure 4 This 43 years old patient presented with mild vitreous hemorrhage and preretinal hemorrhage 3 months after complete PRP. A, showed NVDs on the disk and a tuft of neovessels nasal to the disk (arrows). NVE on the upper arcade are not shown in the color photo. He had visual acuity of 0.6. One month after first bevacizumab injection, (B) showed better visualization of the retinal details and regression of NVDs on the disk and (C) the angiogram showed no NVD on the disk with residual leakage from NVE on the upper arcade (arrows) and NVD nasal to the disk. There is upper macular intraretinal leakage (edema).The central macula however was dry. He was given a second injection. Six weeks after 2nd injection, D, angiogram showed residual activity of NVE on the upper arcade and nasal to the disk but no vessels on the disk. After 4 months from 1st injection, re-vitreous hemorrhage was observed. E, angiogram showed reperfusion of NVDs on and nasal to the disk and NVE on the upper arcade. A 3rd injection was given. F&G,4 weeks after injection, angiogram showed disappearance of NVD and NVE. Final visual acuity was 0.9. Cryopexy to the anterior retina was done to stabilize the final outcome.