Figures & data
Figure 1 Relationship between odds ratios for cardiovascular events and corresponding differences in systolic blood pressure. Reprinted with permission from Staessen JA, Wang JG, Thijs L. 2003. Cardiovascular prevention and blood pressure reduction: a quantitative overview updated until 1 March 2003. J Hypertens, 21:1055–76. Copyright © 2003 Lippincott Williams & Wilkins. The left-hand panel shows the relationship between odds ratios for cardiovascular events (experimental treatment versus reference treatment) and differences between treatments in achieved systolic blood pressure using data from clinical trials of antihypertensive drugs. The meta-regression line, which is shown with its 95% confidence interval, was weighted for the inverse of the variance of the individual odds ratios. The right-hand panel shows the results of more recent trials superimposed on the meta-regression line.
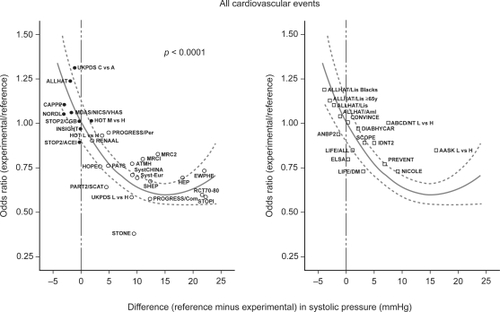
Figure 2 Risk ratios for mortality as a result of cardiovascular disease and coronary heart disease in patients treated for hypertension compared with gender- and age-matched hypertensive and normotensive subjects (Derived from CitationBenetos et al 2003).
CitationBenetos et al (2003) used data from 8893 treated hypertensive patients and 25,880 untreated age- and gender-matched normotensive and hypertensive control patients to determine the influence of hypertension on cardiovascular mortality. Cardiovascular and coronary mortality were two-fold higher in the treated population. After adjustment for systolic blood pressure (SBP) using Cox regression analysis, the differences between the treated and untreated populations decreased from 96% to 14% (cardiovascular mortality, P = 0.05) and from 99% to 16% (coronary heart disease mortality, p = 0.08). Subsequent adjustment for diastolic blood pressure (DBP) had no further effect on the risk ratios.
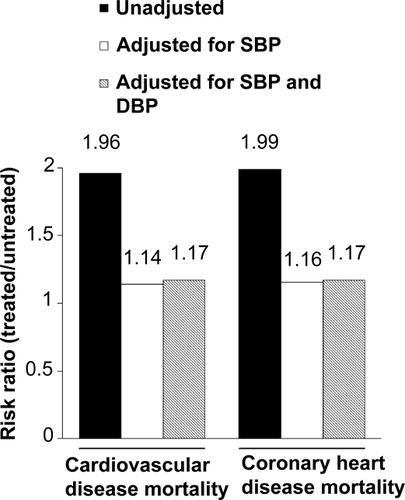
Table 1 Impact of systolic and diastolic blood pressure on risk of an adverse renal outcome (doubling of serum creatinine or progression to end stage renal disease) (Reproduced with permission from Pohl MA, Blumenthal S, Cordonnier DJ, et al. 2005. Independent and additive impact of blood pressure control and angiotensin II receptor blockade on renal outcomes in the irbesartan diabetic nephropathy trial: clinical implications and limitations. J Am Soc Nephrol, 16:3027–37. Copyright © 2005 American Society of Nephrology).
Figure 3 Achievement of blood pressure goals in controlled trials of antihypertensive agents. Reproduced with permission from Mancia G, Grassi G. 2002. Systolic and diastolic blood pressure control in antihypertensive drug trials. J Hypertens, 20:1461–4. Copyright © 2002 Lippincott Williams & Wilkins.
CitationMancia and Grassi (2002) summarized the effects of antihypertensive treatment on systolic and diastolic blood pressure (SBP and DBP, respectively) in clinical trials involving patients with essential hypertension. The data show that higher initial blood pressures (B) are associated with larger reductions during treatment (T). Target blood pressure values (SBP, 140 mmHg; DBP, 85–90 mmHg), shown as dotted lines on the graphs, were achieved more frequently for DBP than for SBP. See legend for key to trial names.
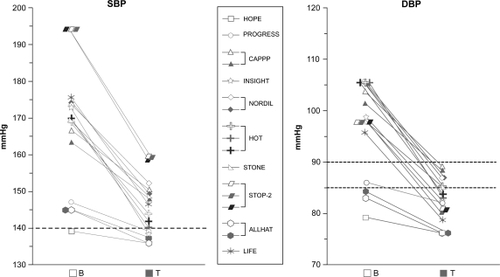
Figure 4 Percentage of patients who achieved SBP <140 mmHg and retained DBP ≥ 90 mmHg compared with percentage of patients who achieved DBP < 90 mmHg and retained SBP ≥ 140 mmHg. Reproduced with permission from Waeber B, Mourad JJ. 2006. Targeting systolic blood pressure: the key to controlling combined systolic/diastolic hypertension. Am J Hypertens, 19:985–6. Copyright © 2006 Nature Publishing Group.
Data from the STRAtegies of Treatment in Hypertension: Evaluation (STRATHE) study show that patients who achieve a target systolic blood pressure (SBP) < 140 mmHg are also likely to achieve a diastolic blood pressure < 90 mmHg. In contrast, a substantial proportion of patients who achieve DBP < 90 mmHg fail to achieve adequate control of SBP. As demonstrated by the figure, this finding is consistent across a range of treatment regimens.
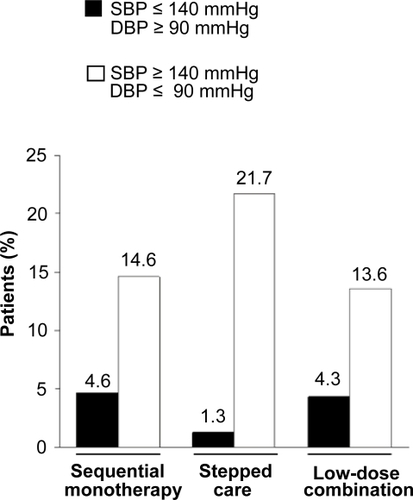
Figure 5 Systolic blood pressure reductions achieved with a combination of amlodipine and olmesartan (CitationChrysant et al 2008).
In the COACH study (Combination of Olmesartan medoxomil and Amlodipine besylate in Controlling High blood pressure), patients with a seated diastolic blood pressure of 95–120 mmHg at baseline were randomized to receive daily treatment with placebo, olmesartan/amlodipine 20/5 mg, 40/5 mg, or 40/10 mg. The figure shows the mean reduction from baseline in seated systolic blood pressure (SBP) after 8 weeks of treatment.
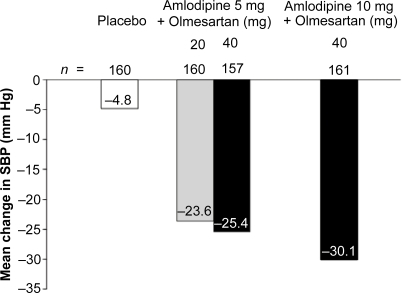
Table 2 Reductions in systolic and diastolic blood pressure achieved with aliskiren monotherapy and with amlodipine/valsartan, amlodipine/olmesartan, and aliskiren/hydrochlorothiazide combination therapy regimens