Figures & data
Figure 2 Apo B lipoprotein with neutral lipids contained in the core.
Reproduced with permission from Koschinsky ML, Marcovina SM. In: Ballantyne, CM, editor. Clinical Lipidology: A Companion to Braunwald’s Heart Disease. Philadelphia: Saunders Elsevier; 2009:130–143.Citation13 Copyright © 2009 Elsevier.
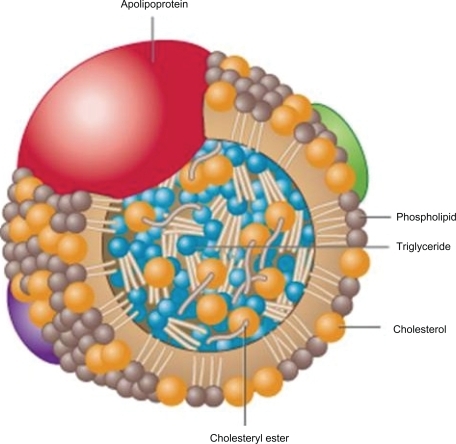
Table 1 Optimal lipid goals in high risk patients.
Figure 3 Increases in triglycerides associated with increases in CHD risk: a meta-analysis of 17 prospective studies.
Abbreviations: CHD, coronary heart disease; CV, cardiovascular; TG, triglycerides.
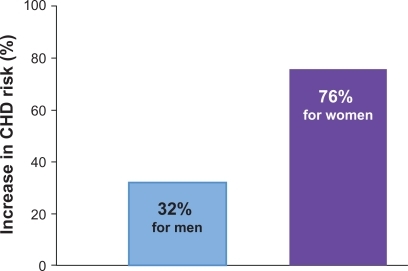
Figure 4 Prevalence of dyslipidemias in men <60 years with angiographic evidence of coronary atherosclerosis. Drawn from data of Genest et al.Citation23
Abbreviations: HDL, high-density lipoprotein; LDL, low-density lipoprotein; Lp(a), lipoprotein a; TG, triglycerides.
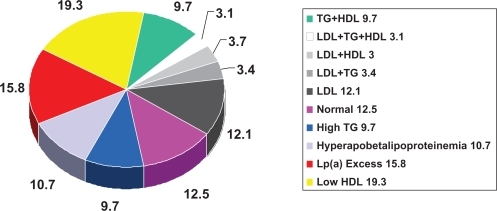
Figure 5 The average RRR for CV events in the secondary population even in the most intensive statin studies is 30%. This leaves significant residual risk for recurrent events. Superko and KingCitation32 compared a variety of studies utilizing LDL lowering versus LDL lowering and HDL elevation. This latter combined approach resulted in projected RRR of 71% to 6% with a NNT of 9.6 overall and 3.4/year.
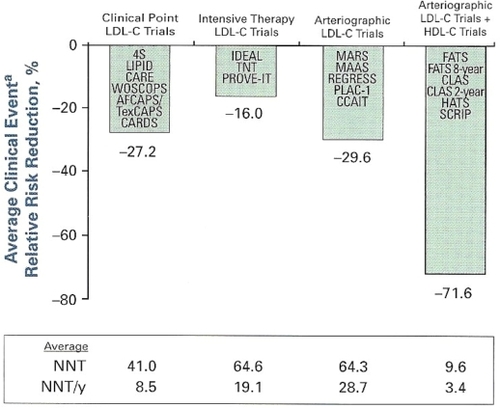
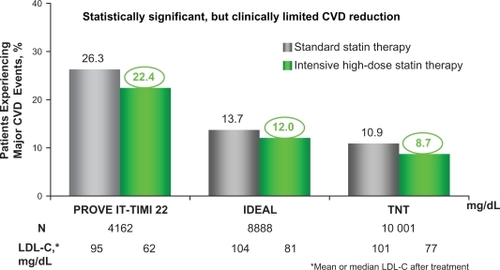
Figure 6 Residual CVD risk in patients treated with intensive statin therapy.
A closer look at 3 trials investigating intensive LDL-C lowering with statin therapy in patients with CHD revealed that residual CVD risk remains in these patients even after aggressive LDL cholesterol lowering therapy. All 3 trials compared LDL-C lowering to ∼100 mg/dL with more intensive LDL-C lowering to ∼70 mg/dL as a means of preventing major CVD events in patients with a history of CHD or acute coronary syndromes. In the Pravastatin or Atorvastatin Evaluation and Infection Therapy-Thrombolysis in Myocardial Infarction 22 (PROVE IT-TIMI 22) study (N = 4162), pravastatin 40 mg reduced LDL-C to 95 mg/dL and atorvastatin 80 mg reduced LDL-C to 62 mg/dL in patients who had been hospitalized for an acute coronary syndrome. After 2 years, 22.4% of patients treated with intensive statin therapy (atorvastatin 80 mg/dL) suffered a major CVD event.Citation4 In the Incremental Decrease in End Points Through Aggressive Lipid Lowering (IDEAL) study (N = 8888), simvastatin 20 mg reduced LDL-C to 104 mg/dL and atorvastatin 80 mg reduced LDL-C to 81 mg/dL in patients with a history of acute myocardial infarction. After 4.8 years, 12.0% of patients experienced a major CVD event even after intensive LDL-C lowering with statin therapy (atorvastatin 80 mg).Citation6 Finally, in the Treating to New Targets (TNT) study (N = 10,001), 10 mg atorvastatin reduced LDL-C to 101 mg/dL and 80 mg atorvastatin reduced LDL-C to 77 mg/dL in patients with stable CHD. After 4.9 years, a major CVD event occurred in 8.7% of patients receiving intensive statin therapy (80 mg atorvastatin).Citation5
These 3 trials reveal that significant residual CVD risk remains in patients even after intensive statin treatment.