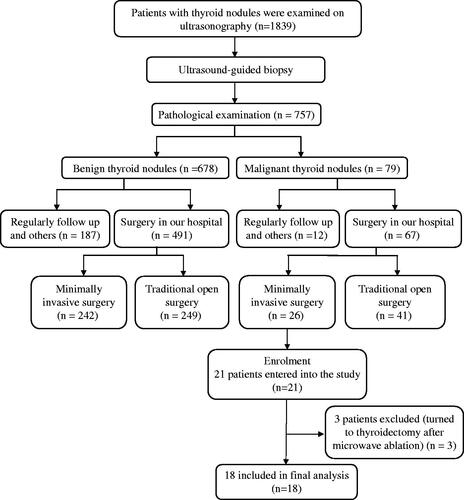
Figures & data
Table I. Demographic and clinical characteristics of papillary thyroid microcarcinoma by MW ablation.
Figure 2. Photographs of MW antennae. (A) The 16-gauge antenna in this study is 10 cm over the entire length, and 3 mm between the narrow radiating segment and the tip of antenna. It is specially designed to treat superficial neck organ nodules less than 10 mm in diameter. (B) Usually, for tumours larger than 20 mm in diameter the antenna with 5 mm between the narrow radiating segment and the tip of the antenna was used. (C) The 14-gauge antenna, 20 cm over the entire length, 11 mm between the narrow radiating segment and the tip of antenna (arrow), is used for abdominal tumours.
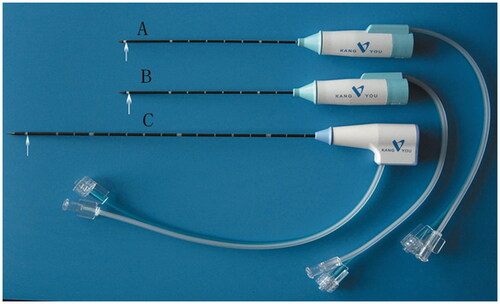
Figure 3. On transverse scan, we can divide the thyroid gland into four quadrants. For a nodule located in the lower inner quadrant, the MW ablation was conducted through lateral cervical approach (R1), but for a nodule located in the lower outer quadrant, a median line approach MW ablation therapy was used (R2). If the nodule was located in one of the other two quadrants, either approach was acceptable. The core principle of the puncture route we adopted was not only that the MW antenna could be percutaneously inserted into the tumour and positioned in its designated place, but that injury of the major structures (carotid artery, trachea, oesophagus) could also be avoided. CCA, common carotid artery; M, tumour.
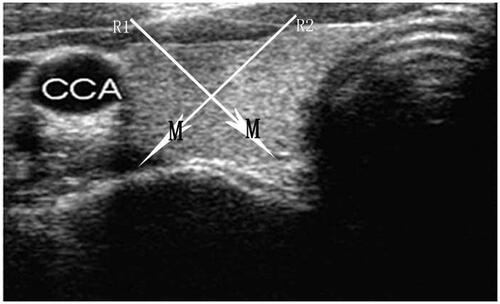
Figure 4. A 48-year-old woman (Patient 11) had a papillary carcinoma in the left lobe of her thyroid gland. The key procedure of the MW treatment is shown here, and the changes in the volume of the tumour before MW ablation and at 1-month follow-up are also presented. (A) Before the ablation, ultrasound examination with ultrasound-guided biopsy confirmed the tumour as papillary thyroid carcinoma 96 mm3 in volume, with inhomogenous internal echoes and microcalcification. (B) Under local anaesthesia a mixture of 0.9% lidocaine and physiological saline was infused into the surrounding thyroid capsule to achieve a ‘liquid isolating region’ (arrow) protecting the vital structures of the neck (carotid artery, oesophagus, nerve) from thermal injury. (C) Under the guidance of ultrasound, a thyroid-dedicated cooled shaft antenna was positioned in the tumour. A sonogram obtained during treatment shows the typical hyperechoic region (arrow) surrounding the antenna. (D) For the PTMC, we achieved slightly more necrosis than the preoperation nodule, evaluated with the contrast-enhanced ultrasound just at the end of each procedure. (E) At follow-up ultrasonography examination 1 month after treatment, the nodule exhibited change to a hypoechoic nature, with a pin site hyperechoic inside (arrow) and a little larger in size (121 mm3 in volume).
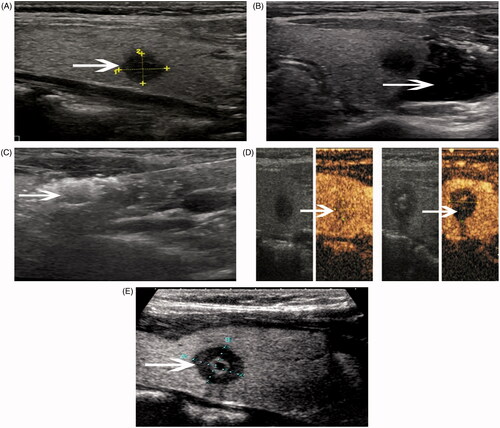
Figure 5. A 50-year-old woman (Patient 3) had a papillary carcinoma in the right lobe of her thyroid gland. The changes in the volume of the nodules before MW ablation and at each follow-up period were presented in the following pictures. (A) Ultrasound examination revealed the solid nodule to be 102 mm3 in volume before MW ablation. (B) Three months after the ablation, the volume of the nodule decreased to 966 mm3. (C) Six months after the ablation, the volume of the nodule decreased to 541 mm3. (D) At another follow-up of this patient approximately 12 months later, we could not find any evidence of tumour and there was no scar at the previous tumour site.
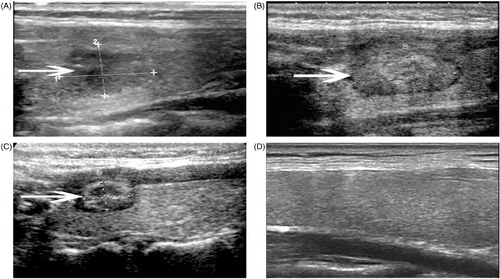
Figure 6. The papillary carcinoma in the left lobe of the thyroid gland of a 45-year-old man (Patient 21) in contrast-enhanced ultrasound and ultrasound-guided biopsy 6 months after MW ablation. (A) During the follow-up period, enhanced contrast ultrasound was performed on the patient. Pre-ablation of the nodule was enhanced inhomogeneously on enhanced contrast ultrasound, whereas non-enhancement (arrow) showed 6 months after the treatment. (B) Ultrasound-guided biopsy was performed 6 months after the MW ablation, and it showed some carbonisation (arrows) visible to the naked eye. The microscopic appearance of the thyroid nodule sample (C) showed necrosis with inflammatory cells in the patient. No cells were noted to be suspicious for malignancy on pathological analysis of the specimen (haematoxylin and eosin staining, original magnification: ×200).
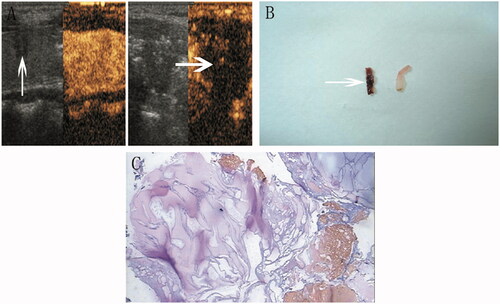
Figure 7. The graph reveals the mean volume reduction ratio at each follow-up visit after MW ablation. Because we achieved larger necrosis than the preoperation nodule, the mean volume of the tumours in the 3-month and the 6-month follow-up reduced more quickly than that in the 1-month follow-up.
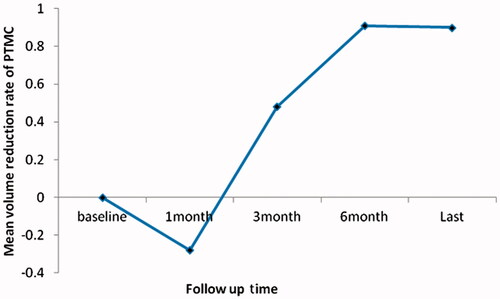
Table II. Outcome of MW ablation.