Figures & data
Table I. Clinical features of patients and tumours.
Figure 1. Artificial ascites technique in assisting MW ablation of hepatic tumours adjacent to the gastrointestinal tract. (A) A 16-gauge IV catheter (arrowheads) is inserted into the space between the surface of the liver and the gastrointestinal tract along the edge of the liver under ultrasound guidance. (B) The outer catheter (arrowheads) is advanced further to close to the index tumour whenever possible; then the inner stylet (arrow) is removed. (C) CEUS is helpful to best display the position of catheter (arrow). (D) Artificial ascites (*) successfully separates the gastrointestinal tract (☆) from the ablated area (arrow). The drip infusion is continued via the catheter (arrowhead) during the MW ablation procedure.
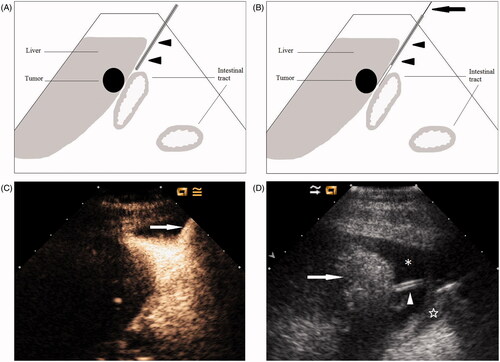
Figure 2. A 73-year-old man with a 2.7-cm HCC in the right lobe of the liver. (A) Ultrasound shows that artificial ascites (*) successfully separates the intestine (☆) from the index tumour (arrow) located at the edge of hepatic segment V. Note the IV catheter (arrowheads). (B) A thermocouple (arrowheads) is placed into artificial ascites (*) between the index tumour (arrow) and the intestine (☆) under ultrasound guidance. (C) Coronal contrast-enhanced MRI before MW ablation shows a tumour (arrow) located at the edge of segment V close to the intestine. (D) Coronal contrast-enhanced MRI 1 month after MW ablation shows the ablation zone (arrow).
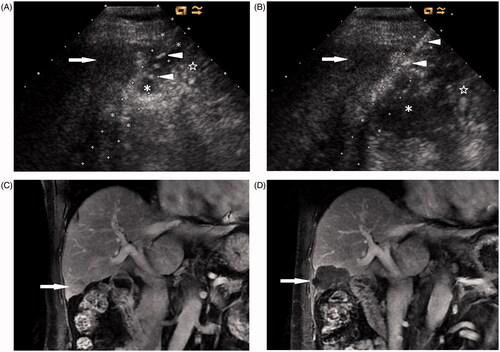
Table II. Relationship between separability and history of laparotomy or TACE.
Figure 3. A 42-year-old woman with metastatic liver cancer in the left lobe of the liver. (A) Ultrasound shows a 1.7-cm hypoechoic nodule (arrow) located at the edge of hepatic segment III adjacent to the stomach (arrowheads). (B) After the induction of artificial ascites (*), the stomach (☆) is successfully separated from the ablated area (arrow). (C) Transverse contrast-enhanced MRI before MW ablation shows a tumour (arrow) with ring enhancement located at the edge of segment III adjacent to the stomach. (D) Transverse contrast-enhanced MRI 1 month after MW ablation shows that the tumour is completely ablated (arrow).
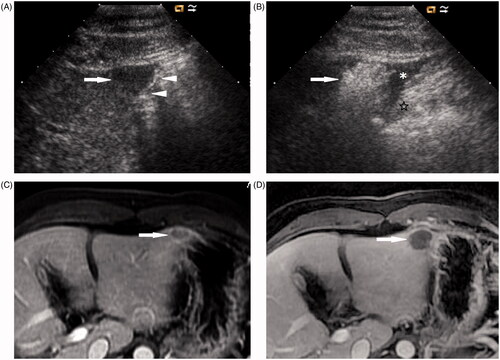
Table III. Characteristics of cases with local tumour progression.
