Figures & data
Table 1. Patient population and tumour characteristics.
Figure 1. Diagram illustrating the technical essentials for thermal ablation of a tumour adjacent to the liver marginal angle (LMA). (A) For small tumours the microwave ablation (MWA) antennae should be placed on the lateral margin of the target lesion opposite the angle side to achieve a segmental block of the entire acute angle. (B) Larger tumours tend to be exophytic towards the extrahepatic organs. Initially, the feeding artery should be blocked under the guidance of contrast imaging to improve the thermal efficiency. Next, the MWA needle should be placed intralesionally to achieve a conformal ablation. GIT, gastrointestinal tract.
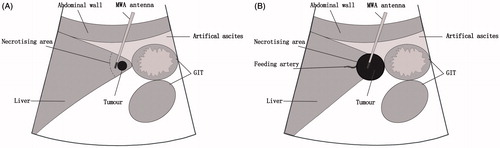
Figure 2. Ablation in a 62-year-old man with a liver tumour adjacent to the right inferior marginal angle in segment V. (A) Preoperative contrast magnetic resonance imaging revealed heterogeneous but obvious enhancement in the arterial phase (long arrow). (B) A computed tomography scan obtained 6 months after ablation found no enhancement of the ablation zone in the entire LMA.
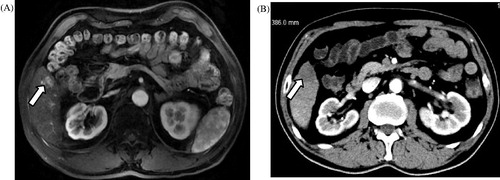
Figure 3. Contrast-enhanced ultrasound (CEUS)-guided MWA in a 62-year old man with primary liver cancer in the vicinity of the LMA. (A) Diffusion-weighted imaging obtained before ablation revealed a small hyperintense area in the left lateral segment (long arrow). (B) The injection of normal saline to separate the liver margin and the stomach wall (arrowhead). (C) Intraoperative CEUS revealed hyper-enhancement (long arrow). (D) US obtained before ablation indicates that the MWA antenna (arrowhead) was placed in the right lateral margin of the target lesion (long arrow). (E) CEUS obtained 6 days after ablation revealed no enhancement (swallowtail arrow). (F) A follow-up contrast magnetic resonance imaging obtained 6 months after ablation displayed no enhancement in the ablation zone of the entire LMA (swallowtail arrow).
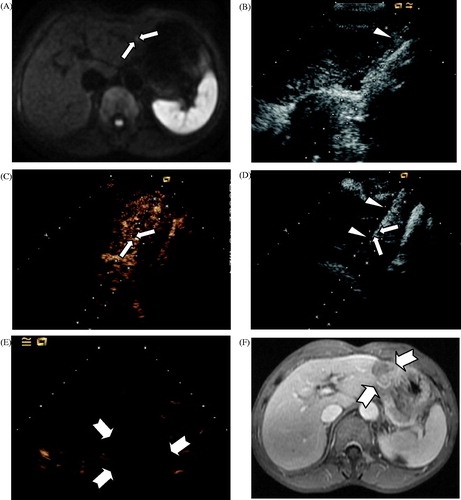
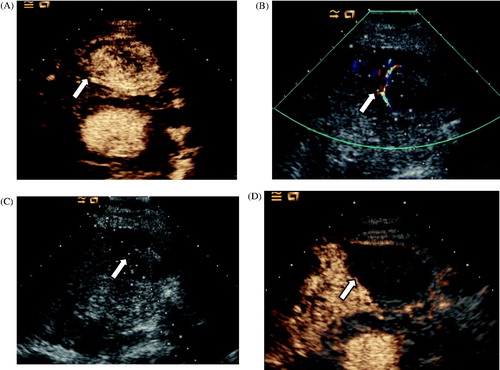
Figure 4. Ablation in a 76-year old man with hepatocellular carcinoma adjacent to the LMA in segment III. (A) CEUS obtained before ablation showed obvious enhancement in the arterial phase (arrow). (B) Colour Doppler ultrasonography depicts feeding arteries entering the tumour on the right side (arrow). (C) A small dose of ethanol was injected via a 21-gauge PTC needle to block the feeding arteries (arrow). (D) CEUS obtained 3 days after ablation showed no enhancement of the target lesion (arrow).