Figures & data
Table 1. Comparison of clinical data in the study and control groups.
Figure 1. The MW antenna (long arrow) was placed into the tumour and thermal monitoring needle (short arrow) was placed into the tumour margin proximal to the gallbladder (GB) for real-time temperature monitoring during the MW ablation.
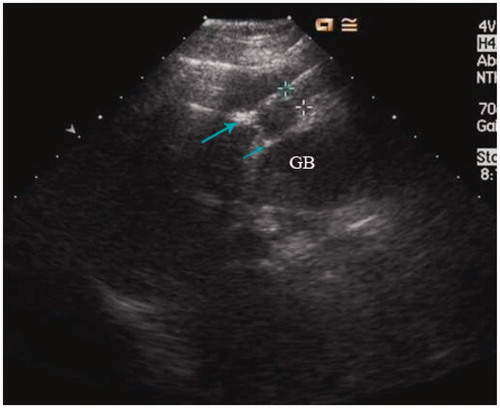
Figure 2. The curves of temperature monitoring during MW ablation for a tumour adjacent to the gallbladder. The temperature of marginal tumour tissue adjacent to the gallbladder was monitored and controlled to fluctuating between 45 and 54 °C during the whole treatment procedure.
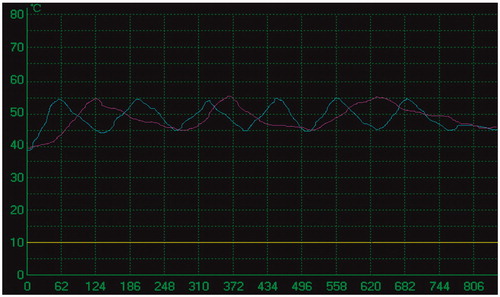
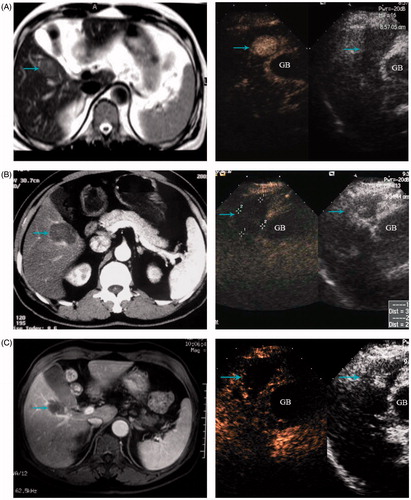
Figure 3. A 68-year-old man treated with MW ablation for HCC adjacent to the gallbladder. (A) Before ablation the tumour (arrowhead) is seen in MRI scans. (B) Six months after ablation, the ablation zone (arrowhead) has no arterial enhancing in CT scans (left) and contrast enhanced ultrasound (right). (C) MRI scans (left) and contrast enhanced ultrasound (right) from 1-year follow up show the ablation zone (arrowhead) had no local tumour progression.