Figures & data
Table 1. Subject, tumour and imaging characteristics, and outcomes of patients receiving thermal ablation for non-small cell lung cancer local recurrence after radiotherapy.
Table 2. Treatment characteristics of patients receiving thermal ablation for NSCLC local recurrence after radiotherapy.
Figure 1. Kaplan–Meier curve of time to local progression (TTLP) for recurrent non-small cell lung caner (NSCLC) treated with thermal ablation in patients previously receiving radiation therapy (n = 17). The median TTLP is 14 months (95% CI: 8, 19).
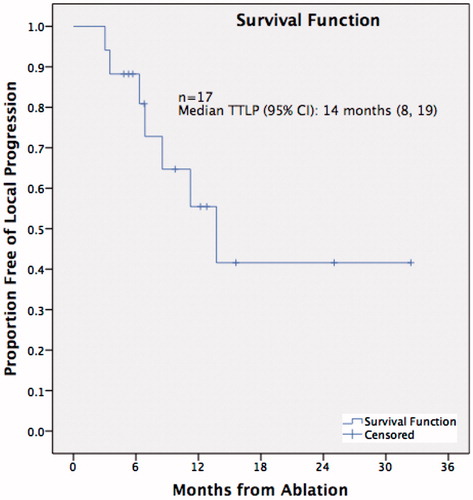
Figure 2. A 55-year-old patient with recurrence of right upper lobe (RUL) non-small cell lung cancer (NSCLC) after 60 Gy of radical external beam radiation. (a) Axial CT lung window shows lobulated RUL mass. (b) Central position of microwave antenna within the tumour. (c) Axial CT scan 24 h after MWA shows surrounding ground-glass opacity (GGO) around tumour (arrows); medial lack of GGO at level of dashed arrows. (d) Volumetric comparison between 3 months post-ablation scan and 6 months post-ablation scan showing reduction in size by 30%, qualifying as partial response under RECIST criteria.
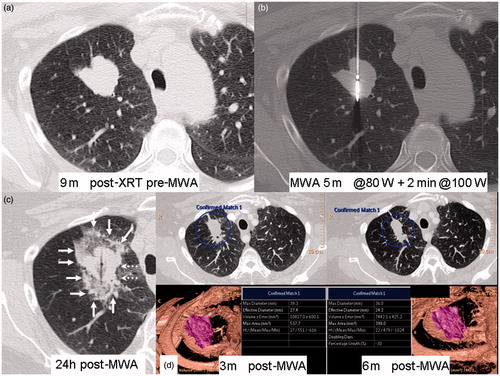
Figure 3. A 55-year-old patient with recurrence of right right upper lobe (RUL) non-small cell lung cancer (NSCLC) after 60 Gy of radical external beam radiation, treated with MWA. Residual avidity on FDG-PET scan 6 months post-ablation (see ). (a) CT-guided core biopsy RUL lesion. (b) CT-guided microwave re-ablation 12 months after initial ablation (c) Axial CT scan 24 h after re-ablation shows large circumferential area of GGO and partial atelectasis. (d) CT scan 6 months after re-ablation shows cavitating non-enhancing ablation site.
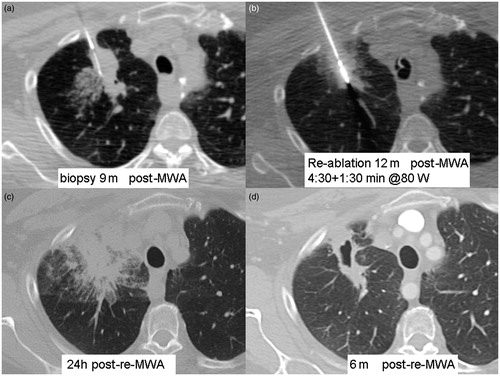
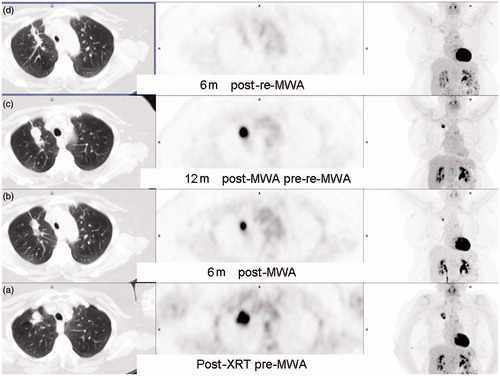
Figure 4. A 56-year-old patient with right upper lobe (RUL) non-small cell lung cancer (NSCLC) with FDG-PET scan series. (a) After 30 cycles x 2 Gy of radical external beam radiotherapy. (b) Six months after MWA shows residual inferior FDG uptake, best appreciated on the coronal MIP. (c) welve months after MWA shows enlarging RUL mass with increasing FDG uptake. (d) Six months after re-MWA shows shrinking focus with no residual FDG uptake.