Figures & data
Figure 1. Mean preoperative tibial ACL footprint as determined using sagittal and coronal MRI with overlay on an axial image. The maximum sagittal and coronal widths of the tibia were determined, and the anterior, posterior, medial and lateral extents of the ACL were measured on MRI and expressed as a percentage of the maximum tibial width from the most anterior and medial aspects of that width. The mean center of the footprint is also expressed as a percentage width.
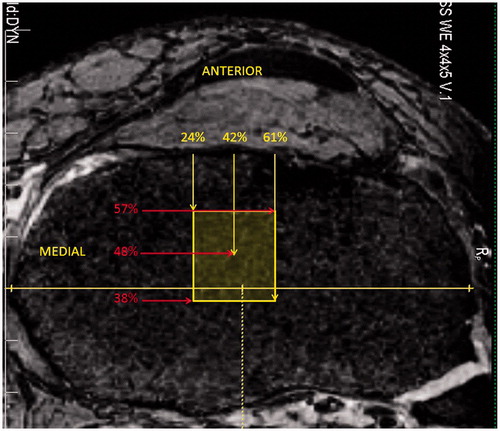
Figure 2. Computer-assisted navigation graphical user interface as used by the novice surgeon group, allowing the operator to understand the location on the tibial plateau and lateral femoral condyle of the right knee. (A) The interface for the tibial side. (B) The interface for the femoral side.
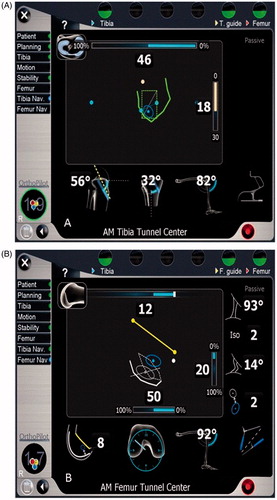
Figure 3. Tibial measurements were made using sagittal and coronal MR images. The maximum sagittal width of the tibia parallel to the joint line, S, was measured and copied to all images (A). The slice at which the AM or PL tunnel broke the subchondral bone of the tibial plateau was located and measured perpendicular to line S. The distance S1 was expressed as a percentage of the maximum sagittal width (B). The maximum coronal width was measured and represented by line C (C). The slice at which the AM or PL tunnel broke the subchondral bone was identified and measured perpendicular to line C. The distance C1 was expressed as a percentage of the maximum coronal width (D).
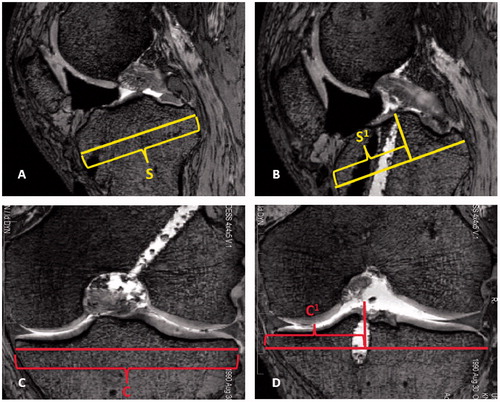
Figure 4. Femoral measurements were made on sagittal MR images of the lateral femoral condyle using modifications to the quadrant technique described by Bernard et al. [Citation4]. First, the most proximal aspect of the femoral notch was identified, correlating to Blumensaat’s line (A). Next, the maximum sagittal width along Blumensaat’s line (W) was identified, measured, and copied to all images (B). The most distal aspect of the lateral femoral condyle was then identified and a line drawn tangential to that point. The perpendicular distance from Blumensaat’s line to this line was the notch height, H (C). Lastly, the slice at which the AM or PL tunnel broke the subchondral bone of the lateral femoral condyle was identified. Measurements were made perpendicular to lines W and H in order to locate the center of the tunnel. The center of the tunnel was expressed as a percentage along Blumensaat’s line and the notch height, displayed as W1 and H1, respectively (D).
![Figure 4. Femoral measurements were made on sagittal MR images of the lateral femoral condyle using modifications to the quadrant technique described by Bernard et al. [Citation4]. First, the most proximal aspect of the femoral notch was identified, correlating to Blumensaat’s line (A). Next, the maximum sagittal width along Blumensaat’s line (W) was identified, measured, and copied to all images (B). The most distal aspect of the lateral femoral condyle was then identified and a line drawn tangential to that point. The perpendicular distance from Blumensaat’s line to this line was the notch height, H (C). Lastly, the slice at which the AM or PL tunnel broke the subchondral bone of the lateral femoral condyle was identified. Measurements were made perpendicular to lines W and H in order to locate the center of the tunnel. The center of the tunnel was expressed as a percentage along Blumensaat’s line and the notch height, displayed as W1 and H1, respectively (D).](/cms/asset/9ba84f98-de45-4040-bc0a-64ae2bff0848/icsu_a_795244_f0004_b.jpg)
Table I. Preoperative dimensions of the tibial ACL footprint.
Table II. Comparison of tunnel placement by experienced and novice surgeons expressed as percentage values.
Figure 5. Centers of the anteromedial (AM) and posterolateral (PL) tunnels mapped on the lateral femoral condyle for each knee studied. Tunnel location was determined using the extension of Blumensaat’s line and notch height on sagittal MRI. Novice surgeon computer aided AM and PL tunnels were significantly anterior to tunnels made by experienced surgeons. The range of AM and PL centers from previous anatomic studies are also mapped on the lateral femoral condyle for comparison.
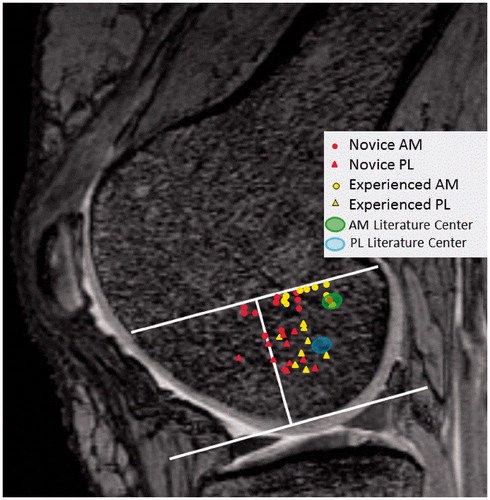
Table III. Overview of studies evaluating the femoral and tibial insertion of the AM and PL bundles compared to tunnel position in the present study. All numerical values are percentages.