Figures & data
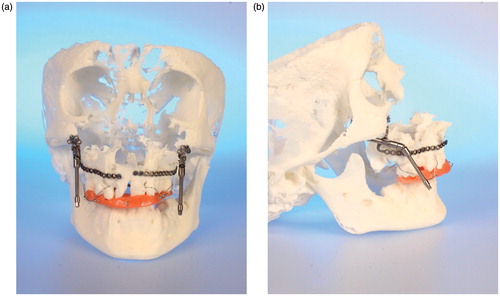
Figure 1. (a) Virtual model rendered by ILUMAVision software and (b) the corresponding SLS model. Individual anatomy is reproduced by SLS technology in detail (e.g., the left paramedian craniofacial cleft). A topographic survey by landmark measurements demonstrated variations between the models of less than 1 mm, which was assessed to be sufficient for surgical use. (c) Measurement of the left anterior orbital height on the virtual and SLS models.
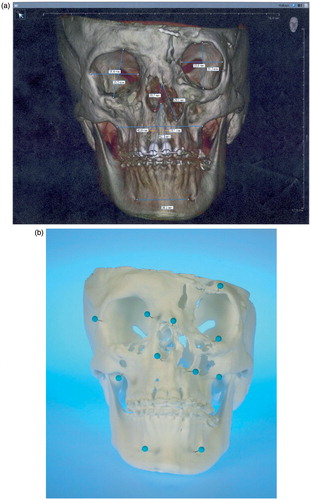
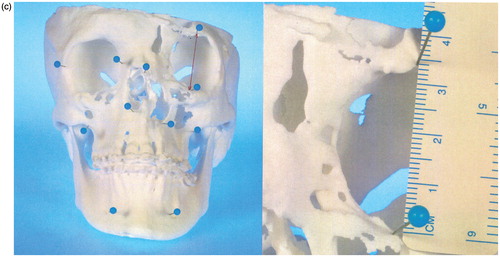
Figure 2. (a–c) CBCT-based models of the first clinical case, with a class III malocclusion and an edentulous maxilla (the models are available in different versions). A two-jaw model surgery was required for correct alignment of the alveolar processes prior to implant insertion. (d–e) The clinical situation before and after orthognathic correction supported by CBCT-based models.

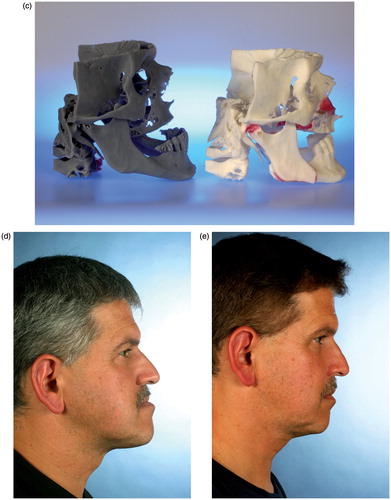
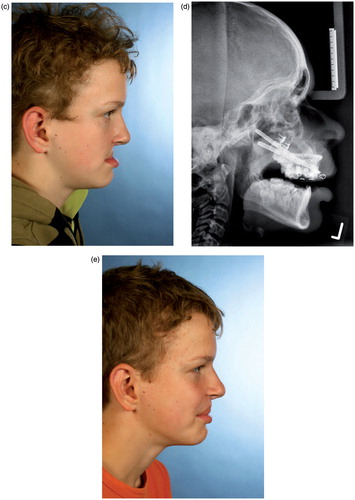
Figure 3. (a and b) CBCT-based models of a distraction case, showing the internal maxillary distraction device selected according to the model geometry, the additional acrylic splint to avoid occlusal interference, and the original devices mounted after removal of material. (c–e) Corresponding clinical pictures of the patient, who presented with a severe maxillary deficiency due to bilateral cleft: (c) The preoperative situation. (d) A cephalogram acquired during the active distraction phase. (e) The clinical situation after six months of consolidation.