Figures & data
Table I. Evaluation of surgical splints with regard to clinical usability.
Figure 1. Virtual splint generation. The desired virtual occlusion can be determined after segmentation of scanned dental casts (upper row). A virtual surgical splint can subsequently be designed and datasets can be transformed to .stl files which are required for further computer-assisted manufacturing (lower right).
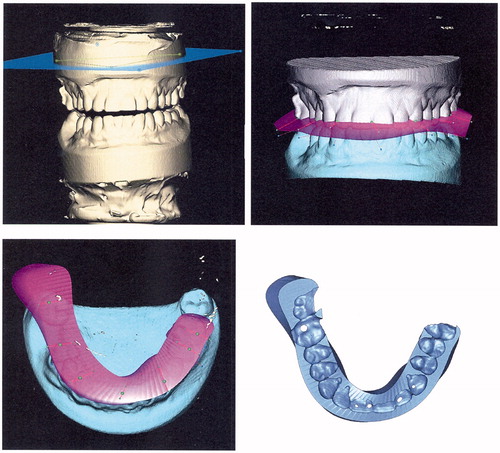
Figure 2. Top row: Prior to surgery, both splints were tested on dental casts with respect to occlusal fitting. In the first patient of the pilot series, the virtual splint (right) is still thicker than the conventional splint. Middle row: Occlusal impressions of both splints are comparable – the posterior extension of the transparent virtual splint (right) was intended to allow an assessment of the possibility of intraoperative grinding of the splint. Bottom two rows: Both splints were inserted during surgery and showed equivalent occlusal fitting with respect to the midline. Laterognathia to the right side (bottom left) was obviously improved after combined orthodontic and surgical treatment (bottom right).
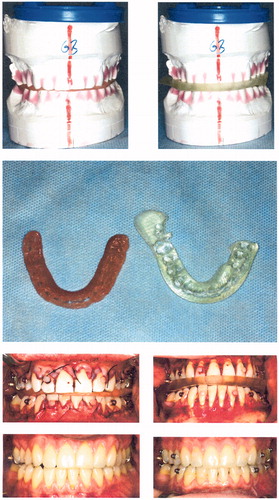
Figure 3. Top row: Preoperative clinical situation in patient 2, a young male affected by amelogenesis imperfecta causing a severe skeletal open bite, after insertion of fixed prosthodontic bridgework. Middle row: Virtual surgery and splint design by RapidSplint: both jaws were repositioned in order to close the open bite and correct dental midlines, and a virtual splint (pink) was designed accordingly. Bottom row: Virtual splint as an .stl-file (left) and after fabrication (right) by 3D printing technology (FullCure™ 720; PolyJet™).
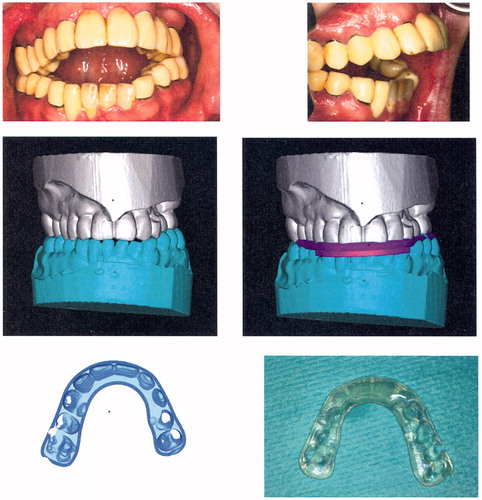
Figure 4. Upper row: The corresponding model situation for patient 2 before surgery (left) and after reorientation of the mandibulomaxillary complex. The desired occlusal relations are safeguarded by the virtually designed splint (right). Lower row: The corresponding situation during surgery. The occlusion of the mandibulomaxillary complex is safeguarded by the virtual splint (left). The final clinical situation (right) corresponds well to the virtually planned situation before surgery ().
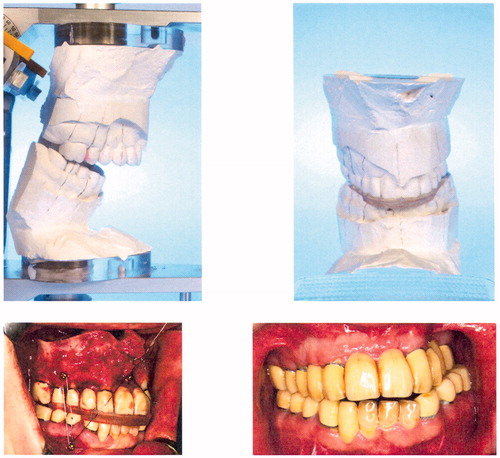
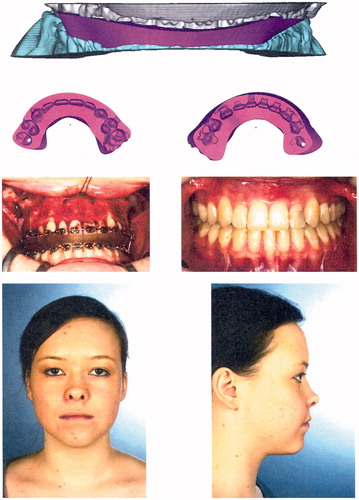
Figure 5. Top row: Preoperative situation in patient 3, a young female with skeletal class III malocclusion due to maxillary hypoplasia. Middle row: Intraoral situation before surgery and after orthodontic treatment. Bottom row: Intended virtual occlusal situation after two-jaw surgery.
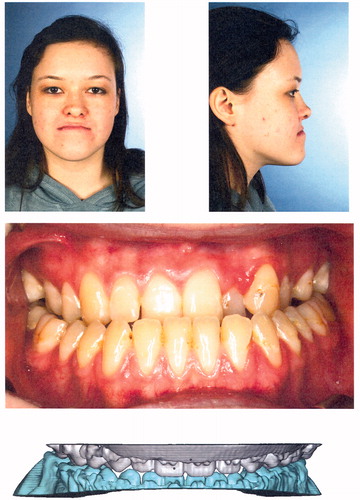
Figure 6. Top row: Virtually designed splint for patient 3 generated using reduced datasets containing only occlusal information for faster data processing. Second row: Detailed reproduction of occlusal impressions of both dental arches. Third and fourth rows: Intraoperative situation with a virtually designed splint safeguarding occlusal relations of the mandibulomaxillary complex (third row, left); final occlusion and final clinical result after termination of combined orthodontic-surgical treatment: class I occlusion, with improved facial balance and harmony.