Figures & data
Table 1. Classification of the hips according to Eftekhar (1978) and Hartofilakidis et al. (1996)
Table 2. Clinical characteristics at the time of primary arthroplasty
Figure 1. A 54-year-old woman who had high congenital dislocation of both hips. At the age of 17, she had undergone a bilateral high-seated Schanz osteotomy to reduce limp. A. Preoperatively. B. 9 years after a cementless total hip arthroplasty of the left hip and 8 years after a similar procedure on the left hip. Both hips underwent femoral shortening and advancement of the greater trochanter. The leg-length discrepancy was 1 cm (the left side being shorter). There were no radiographic signs of loosening of the components and no signs of polyethylene wear.
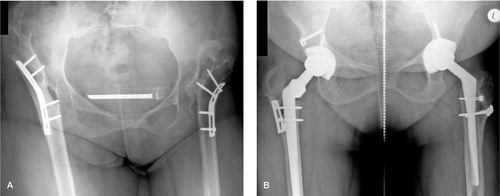
Figure 2. Osteotomies used for various deformities of the femur. The femoral shaft is usually transected distal to the lesser trochanter, as shown by the transverse solid line in (A). A dotted line demonstrates the most distal possible level of the osteotomy. A. Proximal shortening osteotomy with distal advancement of the greater trochanter (vertical solid line) in hips with a previous proximal Schanz osteotomy. B. Segmental shortening with angular correction for hips with a previous, more distal Schanz osteotomy. Copyright for the illustrations in this figure is owned by The Journal of Bone and Joint Surgery, Inc. (published in Eskelinen et al. Cementless total hip arthroplasty in patients with high congenital hip dislocation, J Bone Joint Surg Am. Citation2006; 88: 80-91). Reproduced with permission.
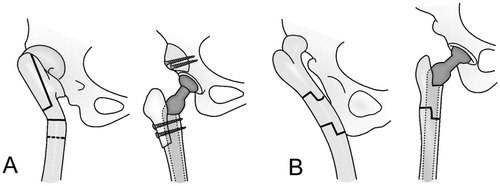
Table 3. Prosthetic components
Table 4. Clinical results of intact and revised hips
Figure 3. Kaplan-Meier survival curve for the press-fit porous-coated Figure 4. Kaplan-Meier survival curve for the CDH femoral compo-acetabular components, with cup revision because of aseptic loosennents, with stem revision for any reason as the endpoint. CI: confi-ing and cup revision for any reason as the endpoints. CI: confidence dence interval. interval.
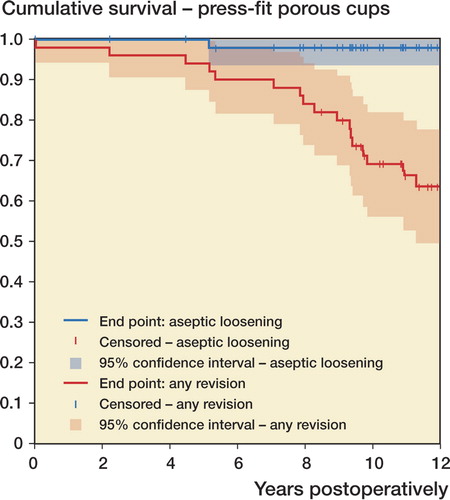
Figure 4. Kaplan-Meier survival curve for the CDH femoral components, with stem revision for any reason as the endpoint. CI: confi-dence interval.
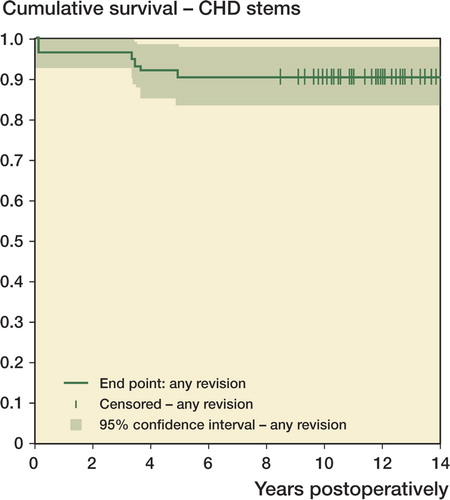
Table 5. Complications