Figures & data
Table 1. The total study group of 174,192 THA patients up to 73 years of age (those with femoral fractures excluded) who were operated 1995 through 2007
Table 2. HRA implant designs in the NARA database, 1995–2007
Table 3. Unadjusted revision rates and reasons for aseptic revision up to 2 years
Figure 1. Unadjusted Kaplan-Meier-estimated cumulative survival (CS ± 1.96 SE) for 1,638 HRAs with estimated 2-year CS of 96.7% (95% CI: 95.7–97.8; no. remaining = 547) and 172,554 THAs with estimated 2-year CS of 98.8% (95% CI: 98.7–98.8; no. remaining = 135,173); p < 0.001 (log-rank test).
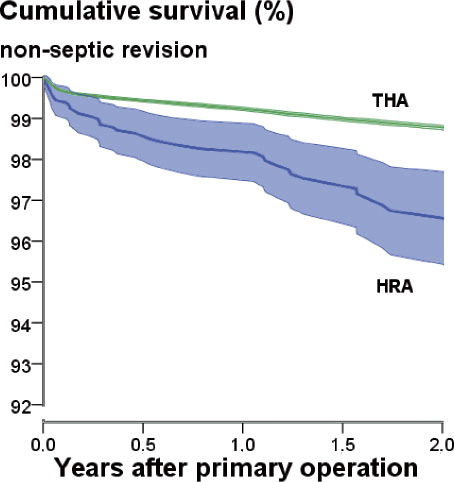
Table 4. Age- and sex-stratified relative risk of aseptic revision within 2 years after primary operation. HRA was compared to all other types of conventional THA or only to the all-cemented (all-c THA) subpopulation. Data are based on a Cox regression model adjusted for operated side, nationality, diagnosis, and type of implant
Table 5. Relative risk of aseptic revision up to 2 years (RR) with 95% confidence interval (CI) in 1,611 hip resurfacings (35 revisions). Data are based on a Cox regression model including age (< 50 or ≥ 50 years), sex, diagnosis, hospital production volume, and the 4 most common HRA designs with BHR as reference
Table 6. The same type of analysis as in Table 5 except that femoral head diameter (categorized as ≤ 44mm, 45–49 mm, 50–54 mm, and ≥ 55 mm) has been added, resulting in 1,552 hip resurfacings (35 revisions) available for analysis
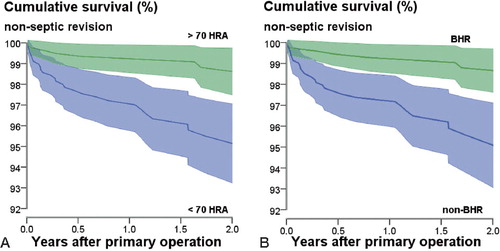
Figure 2. Unadjusted Kaplan-Meier-estimated cumulative survival (CS) of the group of the 4 most common types of HRA, subgroups with significant influence on early non-septic revision rate (CS ± 1.96SE). A. Hospital with ≥ 70 HRAs: n = 820, 2-year CS = 98.8% (95% CI: 97.9–99.8; no. remaining at 2 years = 269). Hospital with < 70 HRA: n = 791, 2-year CS = 95.5% (95% CI: 93.7–97.2; no. remaining at 2 years = 272); p < 0.001 (log-rank test). B. BHR: n = 780, 2-year CS = 98.8% (95% CI: 97.9–99.7; no. remaining at 2 years = 341). Non-BHR: n = 831, 2-year CS = 95.6% (95% CI: 93.8–97.3; no. remaining at 2 years = 200); p < 0.001 (log-rank test).