Figures & data
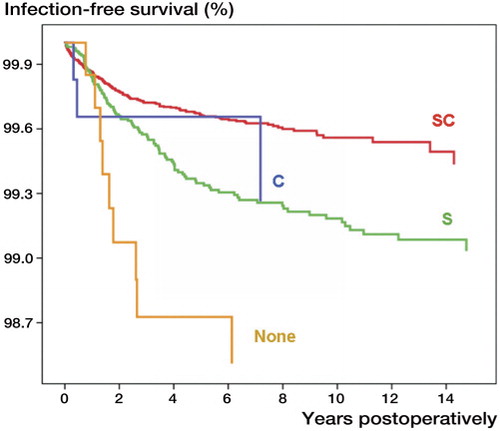
Figure 1. The cumulative revision rates (CRRs; the proportion of operated patients who underwent revision with time) with revision for infection as endpoint in consecutive cohorts of primary total knee arthroplasties (TKAs) performed in patients with osteoarthritis (OA) in 1976–2007 in Sweden. The colored areas represent the 95% confidence intervals for the cumulative revision rates for different time periods. Source: the Swedish Knee Arthroplasty Register, Citation2009.
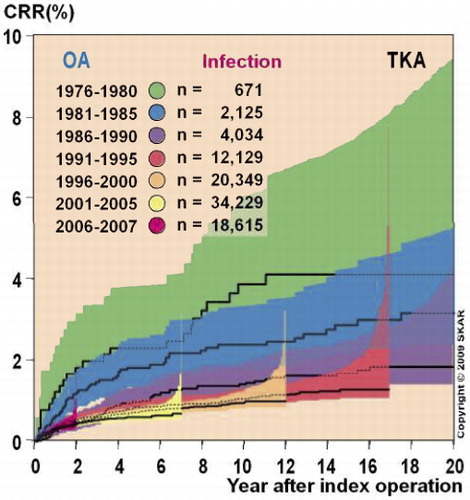
Figure 2. The proportions of infections, aseptic loosening, instability, and pain for all reasons for revision knee replacements in 1997–2008 in Denmark. Source: the Danish Knee Arthroplasty Register, Annual Report 2009 (available online at www.dkar.dk).
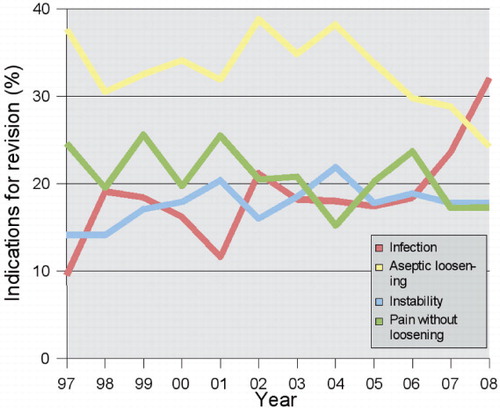
Figure 3. Prosthesis survival with revision due to infection as endpoint following 45,250 primary total hip replacements, performed in Norway in 1987–2007, where no antibiotic prophylaxis (None), intravenous antibiotic prophylaxis (S), antibiotic-impregnated cement (C), or both intravenous antibiotic prophylaxis and antibiotic-impregnated cement (SC) was used. 2,137 operations were performed in a clean-air enclosure, 21,627 in operating theaters with laminar flow, and the remaining operations in operating theaters with standard air ventilation.