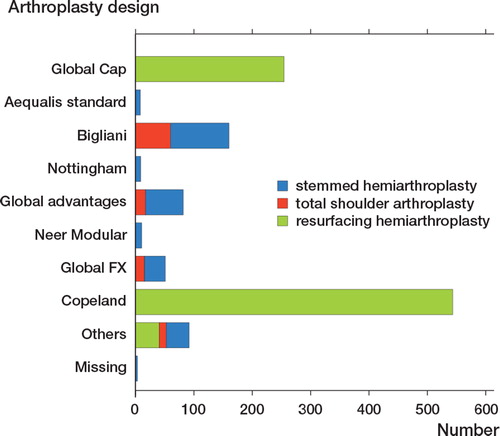
Figures & data
Figure 1. Pathological changes associated with glenohumeral osteoarthritis. Flattening of the humeral head; glenoid wear; posterior subluxation; and osteophytes around the glenoid and the humeral head.

Figure 2. A radiograph showing the classical findings of subchondral sclerosis, joint space narrowing, marginal osteophytes and subchondral bone cysts in a patient with glenohumeral osteoarthritis.

Figure 3. The first known shoulder arthroplasty developed and implanted by Jules Émile Péan in 1893. It is made of a platinum tube and fixated with use of screw holes at the distal end. The proximal ball consists of rubber, hardened by boiling in paraffin. The arthroplasty is on display in the Smithsonian Institute in Washington D.C., USA (Reprinted with permission from the American Journal of Roentgenology).

Figure 4. A modular stemmed hemiarthroplasty with the head connected to the stem by a taper locking system with the possibility of different head-stem combinations depending on the size of humerus.

Figure 5. A hydroxyapatite coated resurfacing arthroplasty with a central grooved impact-fit taper peg for cementless fixation.

Figure 6. The cumulative revision rate after resurfacing hemiarthroplasty presented with numbers at risk and 95% CI showing a 5-year revision rate of approximately 10%.
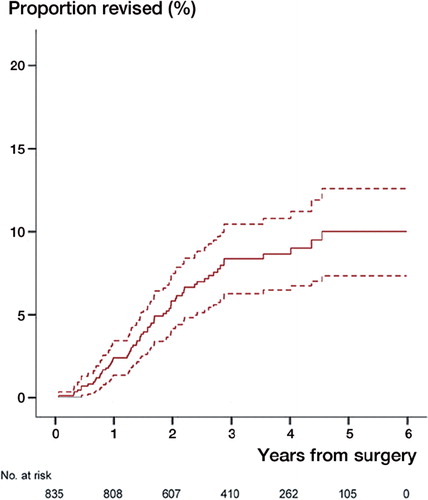
Table 1. The reasons for non-responding with number and percentage of all included arthroplasties
Table 2. The reasons for revision presented with number, percentage of all included arthroplasties and percentages of revisions
Figure 7. The cumulative revision rate for patients age 55 years or younger (brown) compared to patients older than 55 years (black) showing no significant difference, p=0.30.
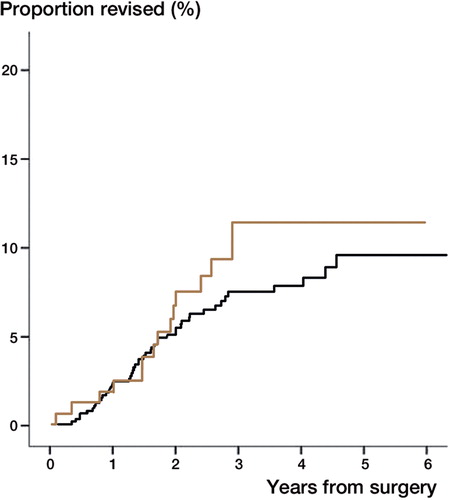
Table 3. The differences in demographics between hemiarthroplasty and total shoulder arthroplasty with number and percentage (in brackets) and mean age with SD (in brackets)
Figure 9. The cumulative revision rate for hemiarthroplasty (red) and total shoulder arthroplasty (grey) showing no difference between arthroplasty designs, p=0.96.
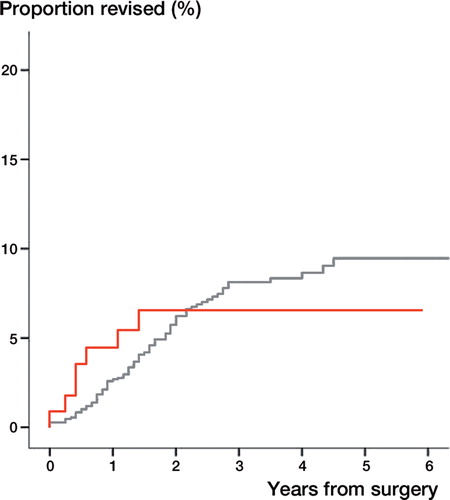
Table 4. The differences in demographics between resurfacing hemiarthroplasty and stemmed hemiarthroplasty with number and percentage (in brackets) and mean age with SD (in brackets).
Figure 10. The cumulative revision rate of stemmed hemiarthroplasty (blue) and resurfacing hemiarthroplasty (green) showing no difference between arthroplasty designs, p=0.93.
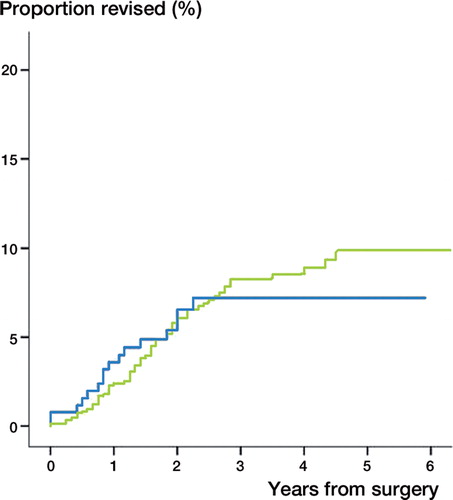
Table 5. Baseline characteristics. Mean values with SD in brackets
Table 6. Outcome scores at one year. Mean values with SD in brackets.