Abstract
The Disability Adjusted Life-Year (DALY) heralded a new age in the development of an evidence base for priority setting and resource allocation. The DALY was intended to represent sound measurement of the incidence and prevalence of conditions in a process by which burden of disease would be determined, health conditions prioritised and interventions evaluated. However, in the reification of objectivity, sight was lost of critical aspects of health and disease, namely that they are not independent of the context in which they occur. This is powerfully illustrated by many reproductive health conditions. Priority setting and resource allocation exercises need to take into account both objective measures and contextually relevant factors. Based on comparative data that highlights the effect of the development gradient on the burden of disease, this paper discusses the implications of context in the assessment of population health and priority setting, with a focus on reproductive health.
Résumé
Le concept d’année de vie ajustée sur l’incapacité (DALY) a marqué un tournant dans l’élaboration d’une base d’éléments pour définir les priorités et allouer les ressources. La DALY devait représenter une mesure fiable de l’incidence et de la prévalence d’affections dans un processus permettant de déterminer la charge de morbidité, de classer par ordre de priorité les problèmes sanitaires et d’évaluer les interventions. Néanmoins, dans cette matérialisation de l’objectivité, on a perdu de vue des aspects essentiels de la santé et de la maladie, à savoir qu’elles ne sont pas indépendantes du contexte où elles se produisent. Ce phénomène est illustré par nombre d’affections de santé génésique. La définition des priorités et l’allocation des ressources doivent tenir compte à la fois de mesures objectives et de facteurs pertinents dans le contexte. Se fondant sur des données comparées qui mettent en lumière l’effet de la courbe du développement sur la charge de morbidité, cet article évoque les conséquences du contexte dans l’évaluation de la santé de la population et la définition des priorités, en mettant l’accent sur la santé génésique.
Resumen
El Año de Vida Saludable (AVISA) marcó el inicio de una nueva era en el desarrollo de una base de hechos que sirve para establecer prioridades y asignar recursos. Con el AVISA se pretendió representar una medida fidedigna de la incidencia y prevalencia de condiciones de la salud en un proceso mediante el cual se determinarı́a la carga de enfermedad, se priorizarı́an las condiciones de la salud, y se evaluarı́an las intervenciones. Sin embargo, al reificar la objetividad, se perdieron de vista aspectos crı́ticos de la salud y la enfermedad, es decir que estas no ocurren independientes del contexto en que se encuentren. Muchas condiciones de la salud reproductiva ofrecen poderosas ilustraciones de este nexo. Los ejercicios diseñados para establecer prioridades y asignar recursos deben tomar en cuenta tanto medidas objetivas como factores contextuales relevantes. Basándose en datos comparativos que destacan el efecto del nivel de desarrollo sobre la carga de enfermedad, este artı́culo examina la incidencia del contexto en la evaluación de la salud poblacional y el establecimiento de prioridades, con un enfoque en la salud reproductiva.
Health resources are not infinite and therefore some mechanism is required for deciding upon their allocation. Tools and policies are needed for this process and underpinning these, is a measure of the health of the population. What is required is an objective or “true” measure of a whole population’s health that accounts for both the mortality and morbidity attributable to disease, one that can be disaggregated in such a way that health conditions and determinants of those conditions can be identified and prioritised, i.e. the burden of disease.
The Disability Adjusted Life-Year (DALY) heralded a new age in the development of an evidence base for priority setting and resource allocation. It was intended to represent sound measurement of the incidence and prevalence of conditions in a process by which burden of disease would be determined, health conditions prioritised and interventions designed and evaluated. This process would reflect merit instead of noise; objectivity rather than advocacy Citation[1]. The role of the advocate, characterised as partisan and unreliable, could be replaced by the diligent efforts of content-free managers who were able to study league tables of DALYs and determine the appropriate steps to maximise population health.
It should be noted, however, that in general, burden of disease measurements aggregate the health of populations, but do not look at the distribution of health within populations. This is as true of the DALY as it is of other measures.
The DALY was motivated by the perceived need to develop an evidence base that could:
| • | uncouple epidemiology from advocacy, thereby creating an objective measure of the mortality and morbidity attributable to different diseases Citation[1]Citation[2], and | ||||
| • | provide a single measure of the burden associated with a disease that combined years of life lost due to premature mortality and years of life lived with disability (or healthy years lost due to disability) Citation[3]. | ||||
In effect, the DALY measures the deficit in a healthy life, attributable to any single condition. The measure is moderated by four factors Citation[2]:
| • | A 3% annual discount rate on years of disability or premature mortality. | ||||
This means three years of life would be lost from a death at 73 years where the life expectancy was 76. However, the first “lost year” is worth a whole year, the second 97% of a year and the third year about 94% of a year due to discounting; a total loss of 2.91 years, not three.
| • | Age weighting. | ||||
Deaths or disabilities occurring in childhood or old age accrue fewer DALYs than deaths or disabilities occurring in the middle years of life, accounting for the greater social value of people in their middle years of life.
| • | Adjustment for sex. | ||||
For the same condition, women with a particular health condition accrue more DALYs than men, because they have a longer life expectancy. The distinction is made here between a social preference based on gender and a biological difference based on sex. It is the latter that is included in the DALY.
| • | Severity impact. | ||||
A health condition with a severity weight of 0 has no adverse impact and a condition with a severity weight of 1 is equivalent to death. The adverse effects of a health state are determined by an “expert” panel based on an “average handicap” associated with the health condition. Average handicap here is based on the disability defined according to the International Classification of Impairments, Disabilities, and Handicaps (ICIDH) Citation[4] living in an “average social milieu” Citation[5].
One of the groups of diseases assessed in the 1990 Global Burden of Disease (GBD) study was reproductive health. This study estimated that reproductive morbidity accounted for 36% of the total disease burden in women aged 15–44 Citation[6]. The 1993 World Development Report assigned 22% of the total burden of disease to women in their reproductive years; and in sub-Saharan Africa as much as 40% of the burden of disease was attributed to reproductive morbidity Citation[7]. This reporting of reproductive morbidity presented a major advance over assessments based solely on maternal deaths which, though devastating, are epidemiologically rare events. The GBD therefore enabled reproductive morbidity to become more prominent in the global health and development agenda Citation[6].
Criticisms of the DALY
Notwithstanding the growing influence of the DALY in population health, and the improvements in demonstrating the burden of reproductive morbidity, the DALY has not been without its critics Citation[6]Citation[8]Citation[9]Citation[10]Citation[11]Citation[12]Citation[13]Citation[14]Citation[15]Citation[16]Citation[17]Citation[18]Citation[19]Citation[20]Citation[21]Citation[22]. Some have criticised it on grounds of equity Citation[9]Citation[10]Citation[12]Citation[15], others for its failure to account adequately for the burdens associated with specific diseases or in specific populations Citation[6]Citation[8]Citation[13]Citation[21]. Arnesen and Nord Citation[11] and Groce et al Citation[14], criticised it because it explicitly values the life of a disabled person as less than that of a person without a disability. The criticisms relate both to the calculation of the DALY itself as an indicator and to its application in global and local burden of disease studies. Robust criticisms have been made of the use of the DALY in reproductive health Citation[6]Citation[8]Citation[16] some of which are highlighted below.
Criticisms of the DALY in reproductive health pertain both to maternal health and other related problems. Primarily, reproductive morbidity is not fully appreciated within the DALY framework, which is based on the assessment of the shortfall attributable to single diseases Citation[16]. The list of potential conditions that contribute to reproductive morbidity is long, many with complex aetiologies and multiple chains of causation. For instance, should the DALYs associated with severe malaria during pregnancy be considered a reproductive health issue or a tropical diseases issue? A decision as apparently simple as this can have profound consequences for where health resources are ultimately placed.
Related to the DALY framework is the need to classify conditions according to the International Classification of Diseases. The classification of reproductive morbidity is complicated because of the involvement of multiple body systems and the differential influence of context Citation[6]. Morbidities classified according to anatomical structure would limit reproductive morbidity to diseases affecting the genito-urinary system. Conditions related to reproductive function would include other organs as well. Many reproductive health conditions span other body systems, for example, pregnancy-induced hypertension, post-partum and other pregnancy-related mental disorders, pre-existing conditions that may be aggravated by pregnancy, and complications of pregnancy that arise as a result of co-morbidities Citation[6]Citation[8]Citation[16]. The problems in the definition of reproductive morbidity are highlighted but not adequately addressed in a specialized volume of the GBD Citation[23]. Unfortunately, without a clear understanding of (or agreement about) what constitutes reproductive morbidity, providing an accurate picture of the burden is not possible Citation[6]. A further concern with the DALY is that it fails to account for the burden associated with intra-partum or late fetal deaths Citation[6]. Complications that cause death and morbidity in pregnant women often result in perinatal mortality with up to 5 million neonatal deaths a year Citation[6]. DALYs, however, are accrued from the moment of birth. Because a late fetal death never involves a live birth, no DALYs are accrued, and there is necessarily no burden of disease associated with the loss Citation[5]. Some find this counting rule offensive Citation[24].
A common problem in reproductive health is under-reporting Citation[16]. For the burden of disease associated with a health condition to be well estimated, there needs to be sound epidemiological data about its incidence (or for some conditions, the prevalence). If a health condition is under-reported, the incidence data will be wrong. Conditions that are under-reported fall largely into two groups: conditions that are under-reported because they are unrecognised or undiagnosed and conditions that are under-reported for social and cultural reasons. Unrecognised or undiagnosed conditions include sexually transmissible infections that may produce pathologies in women, even though they are often asymptomatic Citation[16]. Conditions under-reported for socio-cultural reasons, such as fear, shame or stigmatisation, include a range of conditions that are met with social opprobrium – specific conditions vary from culture to culture but may include induced abortion, infertility, sexually transmissible infections and HIV. Gender-based violence is also under-reported in many cultures and is a risk factor for reproductive morbidity. Pregnancy itself increases the risk of violence as well Citation[16]. A further reason for under-reporting, particularly pertinent in reproductive health, is poor access to health services.
The last criticism of the DALY presented here relates to the methodology for determining the severity weight associated with each health condition Citation[5]Citation[6]Citation[8]Citation[9]Citation[10]Citation[12]Citation[13]Citation[25]. The criticisms range from questioning the appropriateness of using “expert” panels to determine severity weights, to the appropriateness of the use of the person trade-off as a valuation exercise. Proponents of the DALY have argued that it is precisely the use of this kind of methodology that ensures consistency and supports the objectivity of the DALY Citation[1]Citation[2].
Role of context in burden of disease
An important criticism that has been raised but often dismissed in the DALY literature is to do with the context in which a health condition is experienced Citation[9]. It will be recalled that associated with each health condition is a severity weight intended to capture the impact of the health condition on life in an average social milieu. Thus, when estimating the severity weight for a health condition X, the panel of judges estimating the severity weight should take account of both the functional loss associated with X (i.e. the disability) and the impact that the “average conditions of individuals and social responses” Citation[1] (p. 8) or “average social milieu” would have on life lived with X. The problem with using the average social milieu of an entire population is that the average person who has a vaginal fistula will not be the average person in the population. The woman with the fistula will, therefore, not be exposed to the average social conditions in the population as a whole, but to a more extreme version of the population’s social response. Given that poor health is commonly associated with poverty, the average social condition of those with poor health will not be the same as for the general population. The notion of averages is therefore intangible.
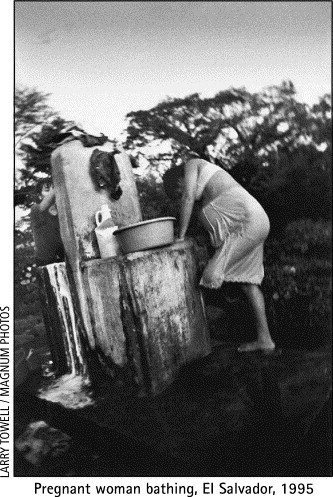
A study by Reidpath et al was designed to examine the effect of social, cultural and environmental contexts on the impact of clinically similar presentations of specified health conditions in a developed country (Australia) and a developing country (Cameroon) Citation[5]. The process of choosing the conditions for this study provides some evidence of the importance of context. Menstrual disorders, as a group of conditions, were considered for cross-country comparison. However, it was found that gynaecologists in Australia, for instance, would describe menstrual disorders under the broad headings of dysmenorrhoea, amenorrhoea, menorrhagia and so on. Women in developing countries, on the other hand, experience a range of menstrual disorders that relate to the lack of availability of sanitary products and the cultural and personal space in which to maintain personal hygiene, creating a powerful link with a number of reproductive tract infections. A study in Kerala state in India described chronic problems of bladder retention for women who, because of modesty and shame, were unable to use toilet facilities during the day. For the same reason, women were compelled progressively to increase the layers of menstruation-soiled fabric underneath their clothes Citation[26]. Whittaker described similar findings in women in southern Thailand Citation[27].
The conditions that were chosen as more appropriate for the study were epilepsy and paraplegia. Approximately equal numbers of male and female, rich and poor, urban and rural participants were recruited. The participants filled in quality of life (ComQoL) and health status (SF12) instruments. Based on photographs taken by the participants, which portrayed the nature of their lives with their health condition, they were also interviewed in depth.
There was a substantial variation between Cameroon and Australia on the health-related and subjective quality of life measures for both epilepsy and paraplegia, with “development” overwhelming accounting for most of the variance in the dependent measures of the SF12 and ComQoL. These results were supported strongly by the qualitative data. Participants in Cameroon with paraplegia, for instance, reported that they were the “fortunate” ones because they were still alive; the general reported life expectancy following injury for people with paraplegia is about two years; many die from septicaemia as a result of untreated pressure sores. A woman described, in some detail, having to negotiate her way onto a pit latrine by rolling and crawling, including negotiating her way around human waste. Others described the difficulty of carrying a pregnancy and taking care of children, a role that was important for them, in order to maintain some respect and self-esteem within the community. Participants with paraplegia in Australia also reported some problems, but these related mainly to stigmatisation and difficulties negotiating access to facilities that were provided by government and community groups.
For paraplegia, there were clear country differences in the macro (e.g. paved roads and user-friendly housing) and micro (e.g. wheelchairs) infrastructure that improved mobility. Thus, one might expect a gradient of severity, with severity lessening as the level of development of a country improves. Similarly, with the advent of modern medicine, later age at childbirth and an improvement in nutrition, fistulae, which were once widespread in Europe and America, seldom occur in these regions. The structural and contextual factors that saw the reduced incidence there remain neglected in developing countries.
The effect of the development gradient has implications for the estimates of burden of disease that have been made at the country and regional level. In the less developed countries (where severity is worse than that indicated by thinking about some putative “average social milieu”) the burden of disease will be greater than the estimates, and in the more developed countries, it will be less than the estimates. Thus, allocating resources on the basis of an “average” severity would therefore further exacerbate inequalities between developed and developing countries.
Criticisms of context
It would seem patent that context is important to the impact of a health condition and, therefore, a severity weight that remained constant over all contexts would be unusable practically and arithmetically Citation[5]. However, there has been a reluctance to accept “contextualised” severity weights because of the potential, so the criticism goes, to reduce the “objectivity” of the DALY, thereby making it largely worthless for comparisons between countries or regions Citation[1]. The arguments are summarised thus: the inclusion of context in the measurement of the burden of disease makes the task too complicated; the inclusion of context misses the point about where the focus ought to lie, which is on those factors that are intrinsic to the individual and result directly from the pathology. Finally, it is argued that those who claim that context is important base their claim on a misunderstanding. They believe that the exclusion of context is paramount to excluding an examination of the social determinants of the burden of disease. These points are discussed seriatim.
The first criticism is that context is problematic because it adds a level of complexity to the issue of modelling population health. The added complexity requires not only empirical data to support it, but significant theoretical work. While it may be true that a rich model of health requires the inclusion of context, a more parsimonious model of population health may be adequate for most purposes, including resource allocation and priority setting. Taking the notion of context to its limit, every non-fatal health outcome is unique:
“… characterized by the initial pathological process, by its antecedent biological, social, economic causes, by the characteristics of the individual affected and the characteristics of the social milieu and by society’s response to the individual with the condition” Citation[1] (p. 22–23).
Consequently, there would need to be a separate severity weight for every person with a health condition, because each person embodies a unique context, making the inclusion of context untenable.
In reality, there has to be a balance between the assumption that the entire world is one context, and that each individual belongs to his or her own unique context. In effect, what is needed is to find those elements of the context that affect populations, not individuals. There is no absolute rule about what effects should be characterised as contextual. Different countries will be more or less homogenous over a range of different social, cultural and environmental factors. This should be viewed as a challenge for health research and not an insurmountable obstacle. There is almost no research that looks at this aspect of health outcomes. Ignoring the problem, however, is not the answer.
In our research, we utilised a combination of participatory research methods, in-depth interviews and self-report quantitative scales to develop a picture of the individual, lived experience, and the degree to which the context rather than the individual factors might contribute to the impact of the health conditions. This provided a balanced approach, whereby the qualitative data supported and enhanced the quantitative data. In addition, it was possible to identify the contextual factors that affected populations as well as those that pertained to individual, lived experiences. The fact that the morbidity data relied on self-report, however, will be of concern to some.
Self-report has been criticised because people’s reports about their own experience are not necessarily reflective of a broader reality Citation[28]Citation[29]. For instance, the population in Bihar in India reported better health than the population in Kerala. However, Keralites have a higher life expectancy and lower rates of clinically verified morbidity than the people of Bihar, presenting a paradox in the interpretation of the self-reported data Citation[29]. This paradox is seen as evidence of a general criticism of self-reported data because it does not reflect the “external reality” Citation[29] vis-à-vis a population’s health.
Interestingly enough, even among those distrustful of self-reported health, pain appears to be an exception to the rule. In the development of the burden of disease work, expert panels considered three states – rheumatoid arthritis, angina, and severe sore throat Citation[1] (pp. 94–96) – in which pain was acknowledged to be a significant factor contributing to the burden of the disease. In general, the experience of pain is unverifiable, and reliant on highly privileged access to an internal state. That this should be permissible, but other self-reported data should not be, is noteworthy, particularly in light of the fact that the experience of pain appears also to be affected by context Citation[30]Citation[31]. Less stressful environments not only improve the degree to which people cope with pain, they appear to reduce the pain itself.
However, even if one were to reject the internal experience as a basis for assessing morbidity, this does not mean that we should reject self-reported data. Self-reported data can frequently be externally verified. We can check whether, as one of the Cameroon women with paraplegia in our sample reported, “[c]arrying a pregnancy and to be creeping on the ground is very bad and difficult”. That being eight months pregnant with paraplegia makes mobility harder than not being pregnant with paraplegia is verifiable. That “creeping along the ground” would diminish a woman’s humanity in the eyes of casual observers could be verified, as could other stigmatisation. Further weight would, of course, be added when data were collected from other women who say it slightly differently, but with the same material import.
Another woman from Cameroon with paraplegia reported:
“[I]n this room I do everything, it’s a kitchen, bedroom, sitting room and toilet. Because I have no control, they have made a hole in the middle of the bed so whether I am lying down or sitting up in the bed, it passes through and into a pot under the bed. Because the room now smells very much, I don’t have anybody come and see me.” Citation[5]
All of these could be verified: the odour, the social isolation, the physical isolation and so on. Similarly, stigmatisation and social isolation associated with odours from women with faecal and urinary incontinence from recto-vaginal or vesico-vaginal fistulae, respectively, are externally verifiable. Self-reported data per se are not the problem; indeed, they are essential to developing a true picture of lived experience and the place of context in influencing that experience. Without the richness of these contexts, “burden of disease” becomes a rather hollow concept.
One suggestion, to avoid the need for consideration of context, is to focus on health dimensions such as impairments and activity limitations that lie “within the skin” or are intrinsic to the person, thereby ignoring the interaction between environmental and social contexts and the individual Citation[32]Citation[33]. This, in effect, would result in the description of a disease process that would be fairly uniform and standardised, based on the condition and ignoring any other influences on how the disease may be experienced. However, there are major problems with the evaluation of the severity of a health condition in the absence of any contextual information. If the intention were to provide a measure of the burden of disease in populations, then it is important that the burden is measured, as much as possible, as it truly occurs. Health conditions are necessarily an interaction between a person and their social, cultural, and environmental contexts.
Indeed, the edges between functional limitations that are intrinsic and extrinsic begin to blur as those limitations are examined in different contexts. In Australia, people with paraplegia have wheelchairs and for some, the wheelchairs are even motorised so that the loss of mobility is further reduced. In Cameroon, many people with paraplegia do not have wheelchairs, and their mobility is severely restricted. Wheelchairs do not lie within the skin; hence, it is the interaction between the individual and things extrinsic (i.e. the wheelchair) that improves the mobility. Advocates of the DALY would suggest that provision of a wheelchair amounts to treatment and therefore relates to the intrinsic nature of the condition. If this point were conceded, however, moving the treatment one step further away from “within the skin” is not hard. Wheelchairs alone are of no use unless the environment is designed to support their use. Australia has building codes and laws covering equity of access for people with disabilities, which have led to an improvement in access to buildings and public spaces for people in wheelchairs. In Cameroon, the basic infrastructure to support the free movement of a wheelchair does not exist. Hence, the provision of a wheelchair in one context would not have the same “treatment effect” that it would have in another context. This is a classic example of the effect of the development gradient on the burden of disease. The focus on pathology necessarily excludes a range of potential interventions to reduce the burden of disease.
Social determinants
It has been said of the DALY that it is too biomedical in its focus and that it does not permit an analysis of the social determinants of the burden of disease Citation[6]Citation[9]Citation[10]Citation[12]. Certainly the use of the “within the skin argument” and the rejection of context because it is too complicated, lends weight to this sense. The criticism has been rejected, however, by Mathers Citation[33] who attributed the criticisms of the DALY’s “excessive” biomedical focus to a conceptual fallacy (p. 21), arguing that the DALY was actually very useful in the analysis of the social determinants of the burden of disease. Critics of the DALY, he argued, had failed to realise that an outcome measure of population health need not include all the important determinants of that outcome in order to be used in analyses that look at the relationship between the determinants and the outcome measure. Indeed, it has become a common refrain of DALY proponents that it can be used to examine the social determinants of the burden of disease (see Citation[1]Citation[32]).
However, this argument missed at least one part of the point of the critics. In order to detect a relationship between two measures, they must co-vary (e.g. as one changes, so too does the other). If a single global severity weight is used for each health condition, it is by definition fixed in all contexts and cannot co-vary with any factors. Any analysis, therefore, of effects of context on the severity (if a single global severity weight is used), will show no association.
There has been a failure to recognise that two different types of social determinants of the burden of disease exist. There are (a) the social determinants of the incidence of disease and (b) the social determinants of the severity or impact of the disease. For instance, poverty is a social determinant of (or risk factor for) vaginal fistulae. Poverty would also affect a woman’s options for reducing the associated odour, which would in turn affect the manner in which others related to her – a social determinant of the severity. Poor access to health services, if it persisted, would also contribute to the severity.
Another stark example of the difference between the social determinants of incidence and the social determinants of the impact is provided by infertility. Poverty is a social determinant of infertility (because of the higher rates of STIs among the poor), but it is the social and cultural views of the failure to reproduce and the social construction of gender roles that affect the impact of infertility.
HIV/AIDS is a further example of how the two types of social determinants differ from and yet are related to each other. The level of stigmatisation in some societies negatively affects the lives of those who are HIV positive and thus increases the severity of the condition. Those living in more stigmatising societies would warrant a higher severity weight than those living in less stigmatising societies. Stigmatisation also drives the disease underground and makes it harder to deliver health promotion and safe-sex messages, which in turn increases the population’s risk of infection. A complete analysis of the social determinants of disease would reveal both aspects. Unfortunately, under the current paradigm Citation[33], only half of the equation is recognised.
By ignoring the social determinants of the severity of disease, a critical opportunity is lost to avert part of the burden of disease. The use of the global severity weight hinders the accurate measurement of population health, and therefore interferes with the possibility of sound management.
Conclusion
Getting the measure right is critical, not only for the local resource allocation but also the GBD studies because the DALY is intimately bound to the GBD work. The issue of health resource allocation may be less of an issue in places like North America, Australia and Western Europe than it is in sub-Saharan Africa, Asia and Latin America. The former, wealthy regions, have (a) more dollars per head of population to allocate to health and (b) the financial and technical facility to develop their own burden of disease estimates using any number of different approaches. The latter, poorer regions frequently rely on (a) others’ assessments of their burden of disease, and (b) money from large international agencies to fund them. These international agencies are more likely to look to the GBD study for information about health priorities than an in-country assessment that is criticised because it was not “objective” or accurate, and was not conducted with a tool that carried the imprimatur of agencies like the World Health Organization or the World Bank.
The DALY and GBD methodologies have provided a broad and innovative structure within which to begin to conceptualise the health of populations, prioritise health needs and distribute resources. However, they are based primarily on a biomedical model of health and disease and are top-down in their approach. The objectivity is culture-bound within a view of health and disease that is informed by models and assumptions derived from theories in economics and medicine. The denial of the contribution and value of the contextual factors that contribute to the severity of a condition within the process of allocating resources would seem manifestly unfair – disempowering for those for whom decisions are being made and by design likely to increase inequalities.
Obermeyer has described reproductive health as a concept that extends beyond specific organs, ages and events; it is a concept that can only be fully understood when situated within a social and economic context Citation[34]. This inclusion of context is contained within the framework of principles adopted by the Cairo Agenda. It is insufficient, however, merely to acknowledge the importance of context. There remain gaps in our understanding of the effects of these socio-cultural and economic factors on the determinants of disease and the determinants of the severity of disease. To begin to capture accurately the level of need of individuals, communities and populations, and to ensure the equitable distribution of resources, we need to understand the interplay between the contextual and the biomedical.
The purpose of this paper is not to advocate for the treatment of each individual as belonging to their own unique context but rather to propose a research agenda that enables the development of the evidence required to begin to assess those elements of context that affect populations Citation[5]. There is a need to better understand the conditions that contribute to reproductive morbidity, taking a comprehensive view of reproductive health rather than individual diseases Citation[6], particularly because there are major benefits from reproductive health interventions that do not fall within a disease model.
Acknowledgements
We would like to acknowledge our co-investigators on the original study, Bob Cummins and Aka Kouamé.
References
- C.J.L Murray. Rethinking DALYs. C.J.L Murray, A.D Lopez. The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability from Diseases, Injuries, and Risk Factors in 1990 and Projected to 2020. 1996; Harvard School of Public Health: Cambridge, MA, 1–98.
- C.J.L Murray, A.K Acharya. Understanding DALYs. Journal of Health Economics. 16(6): 1997; 703–730.
- C.J Murray. Quantifying the burden of disease: the technical basis for disability-adjusted life years. Bulletin of World Health Organization. 72(3): 1994; 429–445.
- World Health Organization. International Classification of Impairments, Disabilities and Handicaps. Geneva: World Health Organization, 1980
- Reidpath DD, Allotey PA, Kouamé A et al. Social, Cultural and Environmental Contexts and the Measurement of the Burden of Disease: An Exploratory Study in the Developed and Developing World. Melbourne: Key Centre for Women’s Health in Society, University of Melbourne, 2001
- C AbouZahr. Disability adjusted life years (DALYs) and reproductive health: a critical analysis. Reproductive Health Matters. 7(14): 1999; 118–129.
- The World Bank. World Development Report: Investing in Health. Washington DC: World Bank, 1993
- C AbouZahr, J Vaughan. Assessing the burden of sexual and reproductive ill-health: questions regarding the use of disability adjusted life years. Bulletin of World Health Organisation. 78(5): 2000; 655–666.
- S Anand, K Hanson. Disability-adjusted life years: a critical review. Journal of Health Economics. 16(6): 1997; 685–702.
- S Anand, K Hanson. DALYs: efficiency versus equity. World Development. 26(2): 1998; 307–310.
- T Arnesen, E Nord. The value of DALY life: problems with ethics and validity of disability adjusted life years. BMJ. 319(7222): 1999; 1423–1425.
- C Barker, A Green. Opening the debate on DALYs. Health Policy and Planning. 11(2): 1996; 179–183.
- H Bastian. A consumer trip into the world of the DALY calculations: an Alice-in-Wonderland experience. Reproductive Health Matters. 8(15): 2000; 113–116.
- Groce NE, Chamie M, Me A. Measuring the quality of life: rethinking the World Bank’s disability adjusted life year. On: <www.rehabinternational.org/measuringquality.html. Accessed 12 March 2001
- D.R Gwatkin, M Guillot, P Heuveline. The burden of disease among the global poor. Lancet. 354(9178): 1999; 586–589.
- Hanson K. Measuring up: gender, burden of disease, and priority setting techniques in the health sector. Global Health Equity Initiative. Cambridge MA: Harvard Center for Population and Development Studies, August 1999
- A.S Laurell, O Lopez. Market commodities and poor relief: the World Bank proposal for health. International Journal of Health Services. 26(1): 1996; 1–18.
- G Mooney, L Irwig, S Leeder. Priority setting in health care: unburdening from the burden of disease [editorial]. Australia New Zealand and Journal of Public Health. 21(7): 1997; 680–681.
- Nord E. Multi-attribute health states instruments and calculation of health status indices. 3-5 December. Report No.: Room Document No. 3: Working Party on Social Policy: Ad hoc meeting of experts in health statistics. Paris: OECD, 1997
- M Paalman, H Bekedam, L Hawken. A critical review of priority setting in the health sector: the methodology of the 1993 World Development Report. Health Policy and Planning. 13(1): 1998; 13–31.
- N Papreen, A Sharma, K Sabin. Living with infertility: experiences from urban slum populations in Bangladesh. Reproductive Health Matters. 8(15): 2000; 33–44.
- B.M Sayers, T.M Fliedner. The critique of DALYs: a counter reply. Bulletin of World Health Organisation. 75(4): 1997; 383–384.
- C.J.L Murray, A.D Lopez. Quantifying the health risks of sex and reproduction: Implications of alternative definitions. C.J.L Murray, A.D Lopez. Health Dimensions of Sex and Reproduction. 1998; Harvard University Press: Cambridge MA.
- Bobadilla JL. Searching for Essential Health Services in Low-and Middle-Income Countries. Policy Background Study, Report No. Soc-106. Washington DC: Inter-American Development Bank; June 1998
- E Nygaard. Is it feasible or desirable to measure burdens of disease as a single number?. Reproductive Health Matters. 8(15): 2000; 117–125.
- Mukherjee V. Gender dimensions of basic needs: women’s access to menstrual hygiene and RTIs. Kerala: MacArthur Foundation Fellowship for Population Innovation, 1999. (unpublished)
- Whittaker M. Recognition and treatment of vaginal discharges in Thailand [PhD]. Brisbane: University of Queensland, 1999
- C.J.L Murray, L.C Chen. Understanding Morbidity Change. L.C Chen, A Kleinman, N.C Ware. Health and Social Change in International Perspective. Cambridge MA: Department of Population and International Health. 1994; Harvard School of Public Health, 87–114.
- A Sen. Health Equity: Perspective, Measurability, and Criteria. T Evans, M Whitehead, F Diderichsen. Challenging Inequities in Health: From Ethics to Action. 2001; Oxford University Press: New York, 69–75.
- J.W Varni, M.A Rapoff, S.A Waldron. Effects of perceived stress on pediatric chronic pain. Journal of Behavioral Medicine. 19(6): 1996; 515–528.
- J.A Markenson. Mechanisms of chronic pain. American Journal of Medicine. 101(1a): 1996; 6s–18s.
- C Mathers, T Vos, C Stevenson. The burden of disease and injury in Australia. 1999; AIHW: Canberra.
- Mathers C. Health expectancies and DALYs: towards consistency of measures. 3–5 December 1997. 3-5. Report No.: Room Document No. 4: Working Party on Social Policy: Ad hoc meeting of experts in health statistics. Paris: OECD; 1997
- C Obermeyer. The cultural context of reproductive health: implications for monitoring the Cairo Agenda. International Family Planning Perspect. 25(Suppl): 1999; S50–S55.