Abstract
China’s rural health care system has undergone major changes since the early 1980s, when the country began privatising rural health services. Following fiscal devolution, the rural primary health service was transformed into a fee-for-service system, dependent on the availability of local resources. This article reports some of the results of a study undertaken in 1994–96 to examine the impact of privatization on financing, provision and use of reproductive health services by women in two rural counties in Yunnan Province, China. The most common self-reported symptoms of reproductive morbidity were abnormal vaginal discharge and vaginal tears during home delivery, which went mostly untreated. Hospital-based delivery and use of antenatal care was very low, adversely affected by costs and perceived low quality. Service quality was affected by low investment in training, maintenance and supervision of workers. Most of the burden for maternal and child health care fell on local health workers, yet resources for these services had declined from 1985 to 1995. Only support for family planning services, which were funded and provided separately, had increased. Rural women’s reproductive health needs were inadequately attended to by rural health services following reforms. Our data has helped to increase attention to those needs within planned reform efforts.
Résumé
Le système de santé en Chine rurale s’est profondément transformé quand le pays a commencé à privatiser les soins de santé primaires au début des années 80. Après la décentralisation fiscale, ces services sont devenus payants, dépendant donc des ressources locales. En 1994–95, une étude a examiné l’impact de la privatisation sur le financement, l’offre et l’utilisation des services de santé génésique par les femmes dans deux comtés du Yunnan. Les femmes se plaignaient le plus fréquemment de pertes vaginales anormales et de déchirures pendant les accouchements à domicile, qui ne recevaient généralement pas de traitement. Les femmes recouraient rarement aux soins prénatals et aux accouchements en milieu hospitalier, onéreux et de qualité jugée médiocre. La faiblesse des investissements dans la formation, l’entretien et la supervision du personnel abaissait la qualité des services. Les agents de santé assumaient l’essentiel des soins de santé maternelle et infantile, pourtant les ressources allouées à ces services avaient décliné de 1985 à 1995. Seul le soutien aux services de planification familiale, financés et dispensés séparément, a augmenté. Après les réformes, les services de santé répondaient mal aux besoins en santé génésique des rurales. L’étude a attiré l’attention sur ces besoins dans le cadre d’efforts planifiés de réforme.
Resumen
El sistema de la salud rural en China ha cambiado desde los años 80 cuando se comenzó a privatizar los servicios de salud rural. Este artı́culo presenta algunos resultados de un estudio realizado en 1994–95 acerca del impacto que tuviera la privatización sobre el financiamiento, prestación y uso de los servicios de la salud reproductiva para mujeres en dos condados rurales en la Provincia de Yunnan, China. El uso de los servicios de atención antenatal y de parto hospitalario era muy bajo debido a sus costos y una percepción negativa de su calidad que estaba afectada por la baja inversión en la capacitación, mantención y supervisión de los trabajadores. Aunque la mayor parte de la carga de atención en salud materno-infantil recaı́a en los trabajadores de salud locales, entre 1985 y 1995 se disminuyeron los recursos asignados a dichos servicios. Únicamente el apoyo a los servicios de planificación familiar, los cuales eran financiados y prestados aparte, fue incrementado. Después de las reformas, las necesidades de las mujeres rurales en cuanto a la salud reproductiva no recibı́an una atención adecuada de los servicios de salud rural. Nuestros datos han ayudado a aumentar la atención a dichas necesidades dentro del contexto de las reformas.
Many countries worldwide are undergoing structural adjustment programmes in which public health systems are being reformed and privatised, in some cases encouraged and catalyzed by international donors and multilateral institutions Citation[1]. A driving force has been pressure on government budgets, often exacerbated or caused by the pressure of international debt repayments. Other countries are undergoing self-imposed fiscal devolution and privatization of health service delivery. While the causes of health sector reform in countries may differ, the manifestations are very much the same: fiscal devolution and decreasing state subsidy for public sector health services, decentralization of budgets and decision-making, efforts at cost recovery and more reliance on fees-for-service. The role of the public and private sectors are also changing as increasing numbers of people seek health care from private sources.
Prior to 1980 all health services in China, including family planning, were the responsibility of the Ministry of Health and its network of health bureaus and institutions at provincial, county, township and village levels. Although not driven by external forces, China’s health system has undergone a major transformation since the era of community-based primary health care in the 1960s–70s, symbolized by the barefoot doctor and touted as a model in the 1978 Alma Ata Conference (whose slogan was “Health for All by the Year 2000”).
China’s rural health system has lost much of its guaranteed public funding, with little left of its earlier public health orientation Citation[2]. Over 70% of China’s population resides in rural areas. Prior to 1978, public health services were paid for by a rural health insurance system called the Cooperative Medical Scheme (CMS) and delivered through a three-tiered system at county, township and village level. The CMS covered 90% of the rural population in 1976 Citation[3], and was funded by a combination of subsidies from higher levels, commune welfare funds generated from yearly mandatory contributions by the population (0.5–2% of annual income), and small co-payments at the point of service. CMS funds were managed locally by the village and township.
When rural economic reforms were introduced in 1978, collective funds used to support the CMS all but disappeared, especially in poorer areas. By the late 1990s, only about 12% of the rural population were still covered by the CMS Citation[4]. It was replaced by a fee-for-service system, with people paying for medical care out-of-pocket. Doctors at the village level now operate entirely as private practitioners for fees and township hospital doctors supplement their public salaries through private practice.
At the same time, fiscal decentralization severely limited financial subsidies for social services, including health care Citation[4]. Prior to the 1980s the central government had used surpluses from state enterprises as revenue to fund these services. In the economic reforms beginning in the late 1970s, state-owned enterprises were allowed to keep some of their profits and these revenues declined. Central government revenues dropped from 36% to 14.2% of GDP between 1978 and 1999 Citation[2]. Local officials gained the power to set health budgets but had to rely on locally collected taxes to finance services and meet recurrent costs. The problem of dealing with financial constraints in poor areas was thus transferred to lower levels of government. Some better-off areas established non-agricultural rural enterprises which have been able to generate surplus funds to finance the provision of public services, but this is not the norm. Wherever resources are tight, health spending has become a low priority.
Thus, the burden of financing health services has shifted to local areas and onto individuals. There have been a number of adverse effects of these changes, especially in poor areas. The limited health budget available is used mainly to subsidize salaries of staff at the county and township levels, with little or nothing left to fund services. Lack of funds has resulted in salaries being only partially subsidized for these workers, who must earn the balance of their wages from client fees for curative care and sales of drugs. Critical management responsibilities such as supervision, monitoring and in-service training are supported inconsistently by higher levels. Preventive services such as health education have decreased relative to curative care as local doctors at village level earn their income from fees and the sale of drugs. Some extra budgetary funds may come from higher levels to fund specific programmes, such as immunization campaigns, or for major capital costs. Quality of services at lower levels, however, varies widely depending on availability of funds.
Only family planning among preventive services has fared differently. Since the early 1980s, provision of contraception has been through family planning service stations, under the direction of the State Family Planning Commission and its network at provincial, county, township and village levels Citation[5]. Family planning has been a national priority since the 1970s, and generously funded, especially since 1980 when the one-child policy began. (This policy restricts urban residents to one child and most rural couples to two, although ethnic minorities are allowed more.) Because family planning is mandated by the national government, services must be fully subsidized. Local governments are required to fund free contraceptive services (mainly for IUDs, sterilization and abortion), and poor counties receive financial support from provincial level if needed. The withdrawal of family planning funding from the mainstream public health system, however, removed a guaranteed funding stream which helped to subsidize related services, such as obstetric and gynaecological care and follow-up for problems with contraceptives.
Reproductive health problems affect nearly every Chinese family and require a broad range of both preventive and curative services, mainly for women. In an attempt to better understand how privatization and other changes in financing have affected rural Chinese women’s utilization of reproductive health services, we conducted a study in rural counties of Yunnan Province in 1994–96. We hypothesized that the introduction of fees for reproductive health services would lower utilization of these services and result in poorer health outcomes, especially in poorer areas.
Methodology
The data in this paper were drawn from a larger study conducted in Yunnan Province in southwest China. The province as a whole is relatively poor and below the national average. Only Tibet and Guizhou have a lower average Citation[6]. The province borders Burma, Laos and Vietnam, and the mountainous terrain complicates the extension of health services to the rural poor. By the end of 1991, 71% of counties in Yunnan had shifted to a full fee-for-service health financing mechanism.
There are some 10–20 townships per county in Yunnan. The data and results presented here focus on three townships. The poorest, both in Shuangbei County, were Ejia Township, with a per capita income of around 325 yuan (US$1=8.25 yuan) and Dazhuang Township, with a per capita income of 340 yuan in 1995. Pubei Township in Yimen County was the better-off of the three, with a per capita income of around 905 yuan in 1995. The distance from the county centre, where the county hospital and reasonable medical care are to be found, is 176 kms from Ejia, 31 kms from Dazhuang and 8 kms from Pubei.
The study utilized questionnaire surveys with 1,766 women of reproductive age, about 600 per township, representing 10.3%, 10.8% and 16.6% of married, reproductive age women in Ejia, Dazhuang and Pubei respectively. Among the surveyed women, 545, 423 and 550 in the three townships had given birth in the last eight years. Although eight years was considered too long a period for accurate recall of maternity events, given China’s low birth rate, this was the minimum amount of time needed to obtain a reasonable sample of women who had given birth. Within the survey townships, stratified cluster sampling was used to select survey villages. Within these villages, all women who gave birth in the last eight years and some other reproductive age women were interviewed using a standard, pre-tested questionnaire. The questionnaire obtained information on symptoms of reproductive morbidity, service utilization, and constraints to utilization. Morbidity was measured using a detailed symptom list that corresponded to symptoms of serious problems of pregnancy, delivery, the postpartum period, contraceptive use and RTIs. These included abnormal vaginal discharge, vulval itch or burning, abnormal bleeding – e.g. during pregnancy or more than two weeks postpartum – abdominal pain, pain during intercourse, fever, and others. While imperfect as a method of measuring morbidity, since symptoms do not always correspond to actual illness (especially for RTIs), they indicate whether women sought care for symptoms that should be seen by a doctor. Interviews were conducted by women teachers and second-year medical students from Kunming Medical College specializing in maternal and child health, who were intensively trained by the research team in gender-sensitive methods of interviewing and role-play. The estimated response rate was over 80%. Data were entered and cleaned by the students who conducted the interviews. SPSS software was used for the analysis and a significance level of 0.05% was used for all analyses, including stepwise regression.
Three additional questionnaires were used to collect community-level financial and other data for the villages, townships and counties studied, to interview all health providers providing reproductive health services to the women surveyed, and to gather budget and financial information from all health facilities serving the women sampled. Community-level data were gathered on trends in maternal mortality and infant mortality, per capita income, health budgets, and financing of reproductive health services, especially family planning versus maternal and child health (MCH) services. Budgets and records of accounts were examined and interviews conducted with local health officials and health institution managers and providers to obtain information on resource flows, time allocation, criteria for budget setting, and clinical data on visits for different reproductive health problems.
Quantitative data were supplemented with information obtained through informal interviews with rural women, rural doctors and health personnel in village, township and county level institutions. Participatory rural appraisal (PRA) activities Citation[7] were carried out over six days in four villages of Dazhuang Township by a team consisting of two teachers (one of the authors, who teaches at Kunming Medical College, and one from Yunnan Institute of Nationalities) and six social work students. Four men and 34 women villagers participated in mapping, oral histories, ranking, group interviews and individual interviews on pregnancy and delivery experiences. These PRA activities gathered further information on reproductive health beliefs and behaviours and barriers to service utilization, both actual and perceived. A complete description of the methodologies used in this study and the larger study from which this article is drawn can be found in previous publications Citation[8]Citation[9].
This paper reports on the most common symptoms of reproductive morbidity reported by the women surveyed, whether they sought care for these, and whether or not they utilised antenatal care or delivery with a trained attendant. It also analyses the impact of changes in health financing and fiscal devolution on local expenditure on family planning vs. maternal and child health servicess and training and maintenance of local health service providers.
Symptoms of reproductive morbidity and health care seeking
Fig. 1 Women’s self-reported reproductive morbidity (at least one symptom), 1995Footnote1.
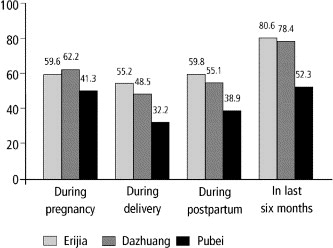
Fig. 2 Women’s health seeking for reproductive health morbidity, 1995Footnote2.
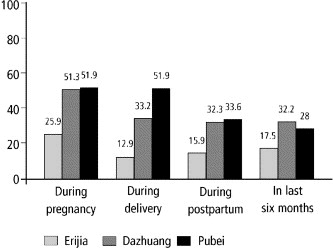
Morbidity reported from common reproductive health problems was substantial among women from all three townships while health care seeking for problems was low, especially in the poorest township, Ejia. Many women experienced symptoms during pregnancy such as headache and swelling, possible signs of hypertension of pregnancy (the third most important cause of maternal mortality in rural China) Citation[10]; only one-third of women in Ejia sought care compared to two-thirds of women in Pubei, the best-off township, closest to county level facilities. The highest reported morbidity in the previous six months was from abnormal vaginal discharge, suggestive of RTI, followed by vaginal tearing during delivery, and problems following IUD insertion or abortion (data not shown). Low rates of delivery attended by a trained attendant contributed to vaginal tears, and few women (9%) had vaginal tears repaired.
Few women sought diagnosis or treatment for RTIs either. Few village and township-level facilities were equipped to diagnose and treat RTIs, and health providers were not well trained to do so either. In all three townships surveyed, only three of the 57 village clinics had speculums. Documented rates of RTIs among rural women in Yunnan are as high as 50%, including a rate of candida of about 20%, trichomonas 16.2% bacterial vaginosis 14.7%, chlamydia 5.5% and gonorrhoea about 0.5% Citation[11], yet most women with symptoms in our study were never seen by the health system. Male rural doctors expressed their unwillingness to do this work, and local women expressed embarrassment and reluctance to see a male doctor for such problems.
Antenatal and delivery care with a trained birth attendant
Table 1 Service utilization for delivery, 1988–1995, (n=1518)
Table 2 Reasons women gave for not having any antenatal care, 1995, (n=423)
Impact of health financing on family planning vs. MCH services
Many of the problems described above are directly related to shortages of funds for local health services. In contrast, local funds for family planning services were widely available. While the MCH budget of local health bureaus has remained fairly constant in the last decade, it has actually been decreasing in real terms because of inflation, while the family planning budget has increased.
Table 3 Family planning and MCH expenditures per married woman, Dazhuang and Ejia Townships, Shuangbei County, 1985–95Footnotea
Table 4 Percentage FP and MCH expenditure generated from user fees, Dazhuang and Ejia Townships, Shuangbai County, 1985–95Footnotea
The MCH system has been losing ground and an increasing burden of health expenditure has fallen on pregnant women and local government. After deflation, total government MCH expenditures per married woman in Ejia and Dazhuang were 0.66 yuan and 1.05 yuan in 1995, down from 1.59 yuan and 1.74 yuan respectively in 1985. Family planning expenditure per married woman, in comparison, was 22.22 yuan and 32.28 yuan in 1995, up significantly from 10 yuan and 13.74 yuan respectively in 1985. User fees accounted for 51% and 54% of all MCH expenditure in 1995 compared to 32% and 38% in 1985. In contrast, user fees accounted for 22% and 25% of family planning expenditure in 1995, up from 10% and 11% in 1985.
A comparison of trends in government and service user burden for MCH and family planning shows that county government budgets for family planning were from two to ten times higher than for MCH, and the annual increase for family planning consistently higher from 1990–95. In the two counties where our survey was carried out, the MCH budget in 1995 was 188,000 yuan in Shuangbai and 490,000 yuan in Yimen, compared to an FP budget of 1,380,000 yuan in Shuangbai and 798,000 yuan in Yimen. The annual increase in the MCH budget between 1990 and 1995 was minus 1.2% in Shuangbai after deflation compared to 8.9% for family planning, and in Yimen was minus 6.6% for MCH compared to 1.6% for family planning.
Although family planning was better funded, much of the real burden of reproductive health work fell within the mandate of the MCH worker at the local level: antenatal care, health education, delivery, postnatal checkups, immunizations for infants, statistics gathering and reporting for the routine MCH management information system, and frequently follow-up for problems of contraception. In theory routine screening for RTIs was included, though not in practice. In contrast, the family planning worker’s main tasks were the provision of contraception, statistics gathering and reporting, and contraceptive promotion. This disproportionate balance of work compared to financing was a fundamental obstacle to the improvement of the quality and reach of basic reproductive health services for rural women in Yunnan.
The MCH system has operated on a fairly fixed (but actually declining if inflation is taken into account) budget for the last several decades. Staff salary subsidies, especially at county and township level, took up a disproportionate share of limited resources for MCH. At the County MCH Hospital, government funding accounted for 37–45% of total revenue, with most of this amount going to salaries for the MCH clinic doctors. Yet bed occupancy rates for deliveries at the hospital MCH clinic were only 13% in Shuangbai and 10% in Yimen, while the outpatient work of MCH clinic staff was mainly for county town residents. Funds for village-level preventive MCH work and salaries had to be generated from user fees.
As more fiscal responsibility for health service provision devolved to local government, poor counties were increasingly unable to provide adequate subsidy to workers, maintain health facilities and equipment or provide in-service training to health workers. Length of training for lower-level health workers is low (68% of rural doctors reported having six months or less of training) and supervision by higher levels is lacking (only 43% of township-level providers reported being supervised by county level personnel). Only 19 out of 26 township health centre doctors reported that they supervised village level workers. They themselves were supervised even less: only 8 out of 40 county hospital-based MCH doctors and 26 out of 48 county MCH centre doctors reported supervising township level health personnel. This has contributed to deteriorating quality of rural delivery services.
In 1995, most local women in Ejia and Dazhuang were unwilling to pay the 15 yuan charge for a home delivery attended by a trained birth attendant (plus extra costs for medicines). Yet a hospital delivery in those townships cost 200 yuan in that same year. These fees have escalated to 30 yuan at village level, 250 yuan at township level and 600–800 yuan at county level institutions for a normal delivery in 2002.
Thus, lack of resources on the part of both township and village health services and lack of sufficient income to pay user fees and other charges on the part of individual women were the major determinants of deteriorating quality of care and low utilization of reproductive health services by women at township and village level.
Discussion
In rural China, illness has a close correlation with poverty. Not only has the cost of medical services been shown to be a major factor influencing hospital utilization by the poor, but medical costs contribute to households falling into poverty. A 1995 survey of 60 poor families in another rural area of China cited major medical expenses as the most important cause of poverty Citation[12]. A 1998 survey of health conditions in 30 impoverished counties throughout China, conducted by the Ministry of Health, found 23% of rural households citing illness as the main reason for poverty, second only to insufficient labour power (25.7%). Cost was affecting hospital utilization for all illnesses, not just deliveries, and 65.3% of respondents cited economic hardship as the reason for not staying in hospital Citation[13]. A 1993–94 survey in three poor counties in Guangxi, Shanxi and Guizhou Provinces found that 45% did not receive hospital care when it was needed (compared to 9% in rich counties), of whom 63% said the reason was cost Citation[14].
Our study paints a picture of a rural health system in crisis, where health-seeking among women for all reproductive health problems was very low. While basic reproductive health services in the two counties existed to some degree, the health system was being pushed by market forces and the first two decades of health sector reforms in directions detrimental to women’s health. The devolution of fiscal responsibility to lower levels of government and to service users placed an increasing burden on local governments to guarantee basic services. Because China’s population growth reduction goals are prioritized over health goals, the separation of health and family planning services in the 1980s, just as health services began to privatize, siphoned off limited local resources in poor areas from essential primary health care delivery. The separation of family planning from MCH and other reproductive health services appears to have been detrimental to women’s reproductive health. Urgent action is needed to mitigate the worst effects of these changes on poor rural women in communities where local governments do not have adequate resources and where women’s health needs are a low priority in the allocation of household resources.
The findings from this study were brought to the attention of a wide audience of health researchers and government officials involved in policymaking for China’s rural health reform programme in 1997 in a special issue of China’s premier public health journal, Chinese Primary Health Care Citation[9]. Recommendations included that the rural health services better respond to reproductive morbidity, especially symptoms of RTIs and the lack of utilization of delivery care; reconcile the imbalance in funding for MCH and family planning to better correspond to the workloads of rural health workers; spend more of the county MCH budget on supporting township-and village-level subsidies and training and supervision of health workers at those levels; and subsidize salaries of township and village level workers to provide more health education and other preventive care to rural women. Furthermore, there is a crucial need for more women doctors with appropriate training to provide services for RTIs to rural women in Yunnan.
In 1997, China’s Ministry of Health with support from the World Bank and the Department for International Development UK began a national rural health reform demonstration project entitled “Reform of the Basic Health Services in China”. The project, in seven provinces in China (though not Yunnan), aims to reform the financing, training, supervision, management, equipment and clinical service provision of China’s rural primary health care system. A companion project, the “Reproductive Health Improvement Project (RHIP)”, initiated in 1998 and formulated within the framework of the larger project, aims to incorporate basic reproductive health services into a revitalized primary health care system in poor areas. Promotion and provision of safe delivery services and prevention and treatment of RTIs, as well as husband involvement in both services, were identified as key priorities, following upon the findings and recommendations from our research, and baseline surveys and PRA studies undertaken early in the RHIP project. These problems had not previously been identified by national experts for the larger project. The results of the baseline surveys and PRA studies in the four RHIP counties were also published as a special issue of Chinese Primary Health Care Citation[15] and reached a wide audience of health planners. It is our hope that these developments signal belated attention to women’s reproductive health in the health sector reform process in rural China.
Acknowledgements
The data presented in this article were drawn from a larger study in 1994–96 entitled the Financing, Provision and Utilization of Reproductive Health Services in China, funded by the Ford Foundation and conducted by researchers at Shanghai Medical University (Gu Xingyuan, Su Baogang), Kunming Medical College (Zhang Kaining, Fang Jing, Liu Wei, Li Xiaomei, Qi Bingxian, Wang Ailing, Tang Songyuan), Abt Associates Inc (Joan Kaufman, Anne Faulkner), and the Institute for Development Studies, University of Sussex (Gerald Bloom).
Notes
References
- M Bangser. Policy environments: macroeconomics, programming, and participation. G Sen, A George, P Ostlin. Engendering International Health. 2002; MIT Press: Cambridge, MA, 257–280.
- Saich A, Kaufman J. Financial reform, poverty, and the impact on reproductive health provision: evidence from three rural townships. Paper presented at Workshop on Financial Sector Reform in China, Center for Business and Government, Kennedy School of Government, Harvard University, Cambridge, 11–13 September 2001
- W Hsiao. Transformation of health care in China. New England Journal of Medicine. 310: 1984; 932–936.
- G Carrin, R Aviva, J Yu. Reforming the rural Cooperative Medical System in China: a summary of initial experience. IDS Bulletin. 28(1): 1997
- J Kaufman, Z.R Zhang, X.J Qiao. The creation of family planning service stations in China. International Family Planning Perspectives. 18(1): 1992; 18–23.
- National Bureau of Statistics. China Statistical Yearbook 1990 (Zhongguo tongji nianjian). Beijing: Statistics Publishing House, 1999. p. 339 (in Chinese)
- Chambers R. Rural appraisal: rapid, relaxed and participatory. Discussion paper. Institute of Development Studies, University of Sussex, Brighton, UK, 1992
- Zhang KN, Qi BX, Fang J, editors. Reproductive Health Services and Relative Research: Theories and Practices (Shengyu weisheng fuwu jiqu xiangguan yanjiu). Beijing: People’s Medical Publishing House, 2000 (in Chinese)
- A Study of the Financing, Provision, and Utilization of the Reproductive Health Service in Rural China. Chinese Primary Health Care (Zhongguo Chuji Weisheng Baojian) 1997;11(9), Summary 134 (in Chinese)
- Zhang L. Maternal mortality and analysis of cause of death from data in 21 provinces, cities and municipalities in China, 1984–1988. In: Hua G et al, editors. Maternal Health Care (Funu Baojianxue). Beijing: China Population Publishing House, 1992. p. 68–99 (in Chinese)
- J Kaufman, L.Q Yan, T.Y Wang. A study of field-based methods for diagnosing reproductive tract infections in rural Yunnan province, China. Studies in Family Planning. 30(2): 1999; 112–119.
- Kaufman J. Financing, provision and use of reproductive health services in rural China. Report of the meeting Implications of Health Sector Reform on Reproductive Health and Rights. Working Group on Reproductive Health and Family Planning, Population Council, Center for Health and Gender Equity, Washington DC, 1998. p. 68–78
- Meng Q, Hu A. Health poverty reduction: a strategic priority of China’s health reform (Xiaochu jiankang pingkun ying chengwei nongcun weisheng gaige yu fazhen de youxian zhanlue). In: Report of a Conference on China Rural Health Reform and Development, 7–9 November 2000. Beijing: China Health Economic Institute and Institute for Development Studies, p. 72–83 (in Chinese)
- G Bloom, S.L Tang, X.Y Gu. Financing rural health services in China in the context of economic reform. Journal of International Development. 7(3): 1995; 423–441.
- A Study of Reproductive Health Improvement in Rural China (Gaishang shengyuweisheng fuwu yanjiu zhuanji). Chinese Primary Health Care (Zhongguo Chuji Weisheng Baojian) 2000;14(9), Summary 173 (in Chinese)