Abstract
Misoprostol is being used widely by women throughout Latin America, often based on instructions passed along through friends, acquaintances or professionals who may have little information about safe and effective use. This paper presents the experience of a Latin American clinic working in a legally restrictive setting that offers misoprostol as one option to women seeking early pregnancy termination. Between February 2001 and June 2002, 3,225 women who attended the clinic chose to use misoprostol rather than vacuum aspiration. 89.9% returned for follow-up, of whom 76.4% had had a complete abortion within 72 hours, using one, two or three doses of 800 micrograms of misoprostol administered by the woman herself vaginally every 24 hours. The first 78 women who returned for follow-up at 72 hours responded to a questionnaire regarding their experiences. Satisfaction with the abortion process was high, despite some pain, chills, diarrhoea and/or nausea. Seventy-two of the 78 women said they would use misoprostol again if they needed to terminate another pregnancy and would recommend it to a friend. Having a clinic where staff are knowledgeable and experienced in misoprostol use is particularly important in settings where abortion is stigmatised, unsafe abortion common and access to safe services limited.
Résumé
Le misoprostol est largement utilisé par les femmes en Amérique latine, souvent sur le conseil d’amis, de connaissances ou de professionnels qui peuvent Átre mal informés de son utilisation s re et efficace. Cet article présente l’expérience d’un dispensaire latino-américain travaillant dans un environnement juridiquement restrictif qui offre le misoprostol comme option aux femmes souhaitant interrompre précocement une grossesse. De février 2001àjuin 2002, 3255 femmes s’étant rendues au dispensaire ont choisi d’utiliser le misoprostol plutÁt qu’une aspiration. Des 89.9% de femmes revenues pour un contrÁle, 76,4% avaient avorté complètement dans les 72 heures, avec une, deux ou trois doses de 800 microgrammes de misoprostol qu’elles s’étaient administrées par voie vaginale toutes les 24 heures. Les 78 premières femmes revenues pour un contrÁle 72 heures après ont réponduàun questionnaire. Le taux de satisfaction était élevé, malgré quelques douleurs, des frissons, et des épisodes de diarrhée et/ou de nausées. Soixante-douze femmes sur 78 ont déclaré qu’elles utiliseraientànouveau le misoprostol si elles souhaitaient interrompre une autre grossesse et le recommanderaientàune amie. Quand l’avortement est stigmatisé, les avortements non médicalisés sont fréquents et l’accèsàdes services s rs est limité, il est particulièrement important de compter sur un dispensaire où le personnel connaît et sait utiliser le misoprostol.
Resumen
El misoprostol es utilizado ampliamente por las mujeres en toda Latinoamérica, quienes se basan a menudo en las indicaciones de sus amigas, conocidas o profesionales quienes posiblemente tengan poca información sobre su uso seguro y eficaz. En este artáculo se expone la experiencia de una clánica latinoamericana, en un entorno legalmente restrictivo, que ofrece el misoprostol como una opción para las mujeres que desean interrumpir su embarazo en etapas iniciales. Entre febrero de 2001 y junio de 2002, 3,225 mujeres que consultaron a esta clánica optaron por utilizar el misoprostol en vez de la aspiración endouterina. El 89.9% regresó a consulta de control; de éstas, el 76.4% presentó un aborto completo dentro de las 72 horas posteriores a la autoadministración de una, dos o tres dosis de 800 microgramos de misoprostol por váa vaginal cada 24 horas. Las primeras 78 mujeres que regresaron a control indicaron una alta satisfacción con el proceso de aborto, pese a algunos dolores, escalofráos, diarrea y/o náuseas. De las 78 mujeres, 72 expresaron que volveráan a usar el misoprostol si necesitaran interrumpir otro embarazo y se lo recomendaráan a una amiga. En los entornos donde el aborto es estigmatizado, el aborto inseguro es común y el acceso a los servicios seguros es limitado, es importante contar con una clánica cuyo personal posea conocimientos y experiencia en el uso del misoprostol.
Keywords:
Throughout the world, unsafe abortion continues to be a public health problem and one of the main causes of mortality and morbidity in women of reproductive age, particularly among poorer women living in rural and marginalised urban settings.Citation1 Abortion laws in Latin America and the Caribbean are highly restrictive, except in Cuba and Guyana, making it difficult for many women to obtain safe abortions. An estimated 3.7 million unsafe abortions are carried out each year in the region, the highest rate of unsafe abortions in the world: 29 per 1000 women aged 15—44, or one unsafe abortion for every three live births.Citation2 There are some 3700 maternal deaths each year in the region, of which 17% are attributed to complications of unsafe abortion.
Hence, improving women’s access to medical abortion, particularly with misoprostol alone, could become an important strategy for reducing morbidity and mortality related to unsafe abortion. Misoprostol is widely available in the region and its low cost makes it a viable option for women who might otherwise turn to expensive or risky services. Its use, with and without medical supervision, has been linked in some settings to a decrease in complications from unsafe abortion.Citation3
Misoprostol, a prostaglandin E1 analogue, is approved for use in the prevention and treatment of gastric ulcers. Increasingly, it has been used in obstetrics and gynaecology, including for labor induction, first trimester missed abortion, second trimester abortion, prevention and treatment of post-partum haemorrhage, cervical preparation prior to surgical abortion and treatment of incomplete abortion. In clinical trials, a combination of mifepristone and misoprostol for early first trimester termination of pregnancy has a high completion rate of 96—98% up to 63 days of pregnancy.Citation4 Citation5 Citation6 However, mifepristone is not available in any Latin American or Caribbean country. Thus, misoprostol alone, or a combination of methotrexate and misoprostol,Citation7 are medical alternatives for safe, early abortion.
Although widespread, the experiences of women and health care providers with misoprostol for early pregnancy termination are, to date, generally undocumented in Latin America. This article summarises the results from one clinic in Latin America during the initial stages of offering misoprostol alone for early medical abortion to women in a legally restrictive setting. The findings contribute to our understanding of the feasibility, efficacy, acceptability and challenges of offering such services in contexts where unsafe abortion is a major public health problem.
Background
Studies on the use of misoprostol alone for first-trimester pregnancy termination have aimed to demonstrate its safety and effectiveness from 56 to 84 days of pregnancy, dating from the first day of the last menstrual period (LMP). In most studies misoprostol is administered vaginally, as this is more effective than oral administration.Citation8 Citation9 Citation10 Citation11 Citation12 Citation13 Citation14 Citation15 Citation16
A number of clinical trials have sought to determine the optimal regimen for use of misoprostol alone.Citation17 Citation18 Citation19 In July 2003, an expert meeting on misoprostol was held in Washington DC, resulting in a consensus statement on use of misoprostol alone for abortion induction in pregnancies up to nine weeks (63 days) LMP.Citation20 The recommended regimen was 800 micrograms (mcg) administered vaginally with the same dose repeated after 24 hours, for a total of two applications.
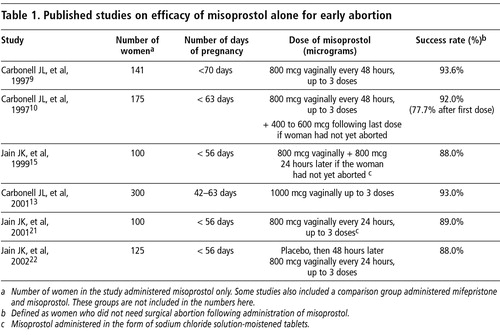
presents a summary of clinical research on use of misoprostol alone. Citation9 Citation13 Citation15 Citation21 Citation22 In the majority of studies, women used 800 mcg every 24 to 48 hours, administered vaginally for up to three doses. These studies also document prostaglandin-related side effects, particularly vomiting, diarrhoea, fever and chills, as common. Uterine pain or cramping and bleeding are also listed as side effects, although some researchers and practitioners consider these effects as being inherent in the abortion process itself, as misoprostol causes the uterus to contract and expel the products of conception.
A comprehensive review of studies on the use of misoprostol alone for termination of pregnancy was conducted and results were discussed by clinic staff before coming to a consensus regarding the regimen that would be used in offering misoprostol to women as an alternative to vacuum aspiration. Ultimately, the protocol that was agreed upon considered effectiveness, ease of application, safety, and acceptability (for both women and providers) as key factors. This included reducing the need to return to the clinic for follow-up visits, given that many women have limited time and resources. Clinic safety was also taken into account since services were offered in a legally restrictive setting.
The services described in this article are used by women of all socio-economic levels. Prior to the introduction of misoprostol in the clinic, both manual and electric vacuum aspiration were (and still are) being offered. The clinic is urban-based but serves thousands of women from both urban and rural areas. It also offers a range of sexual and reproductive health services, including contraceptive counselling and methods, prevention and treatment of cervical and breast cancer, prevention and treatment of sexually transmitted infections, and has a number of community outreach programmes.
Methods
In February 2001, the clinic began offering misoprostol as an option to women who chose to terminate their pregnancies. Clinic staff were interested in the experiences of women choosing this option in order to ensure that this new service was meeting their needs. During the first few months, attending physicians asked women to complete a brief questionnaire during the follow-up visit regarding their experiences with pain, bleeding and tissue expulsion throughout the abortion process, and their satisfaction with the treatment. The purpose was to monitor the provision of a new service and was not designed as a research instrument. Interviews were conducted with the first 78 women who used misoprostol and returned for follow-up, scheduled at three days after the first vaginal application of the drug. Their responses were included in their clinical records. When staff determined that they had sufficient information to merit a decision to continue the service, they ceased asking women to complete the questionnaire.
The clinic continued to fill in the standard medical record of every woman who had a medical abortion, and when more than 3,000 women had used the method, clinic staff and administrators decided to create a database comprised of information about the characteristics of the women and the effectiveness of the method from those records. The database upon which the results reported here were generated included 3,225 women who used misoprostol between 1 February 2001 and 30 June 2002. To maintain confidentiality, no identifiers, such as names or addresses, were included in the database. The results presented in this article, therefore, are not the product of a controlled clinical trial but rather based on the daily experience of a clinic in the early stages of using a new protocol for abortion care. No systematic comparison was made between the characteristics of women who chose misoprostol and those who chose vacuum aspiration.
During this first phase of misoprostol provision, women were given misoprostol at the first visit to insert at home, and asked to come for an initial follow-up visit three days after the first insertion and again 15 days later. The information presented here was garnered during the initial visit and the first follow-up visit 72 hours after the first insertion of misoprostol. All women who attended for the follow-up at 72 hours left the clinic with a complete abortion, either due to the misoprostol alone or via vacuum aspiration. No information is reported from the follow-up visit at 15 days.
Of the 3,225 women, 325 (10.1%) did not return for the first follow-up, so their health status and the effectiveness of misoprostol could not be determined. This may have biased our results, but it is unclear in which direction. Clinic records show that up to 30% of women who have vacuum aspiration never return for follow-up either (Personal communication, clinic researcher, June, 2004). Clinic physicians consider that many of the women who do not return may have been sure their abortion was complete and had no complications, or, their life circumstances may not have permitted them to come back.
Univariate and bivariate analyses were carried out using SPSS 8.0 to describe the characteristics of women who attended for follow-up versus those who did not, and those who had a complete abortion using the regimen defined by the clinic versus those who required vacuum aspiration after using misoprostol. We did not perform statistical significance testing or calculate sample size since the project was not designed as a research project and sampling was not random.
Clinical protocols
During the initial visit, the physician would take the woman’s clinical history, perform a physical and gynaecological examination, and estimate number of weeks of pregnancy. A combination of determinants were used, including first day of last menstrual period (LMP); positive pregnancy test; trans-abdominal ultrasound with either absence of gestational sac (pregnancy less than 4 weeks), gestational sac of <10mm diameter (pregnancy of approximately 4 weeks), gestational sac of 10—20mm diameter (pregnancy of 5 weeks) or presence of embryo or fetus (pregnancy of 6—10 weeks).
The criteria for offering misoprostol as an alternative to vacuum aspiration included: maximum length of pregnancy ten weeks (70 days), overall good health, no history of allergy to prostaglandins (including misoprostol), and commitment to return to the clinic for a follow-up visit and to undergo vacuum aspiration if a complete abortion was not achieved with misoprostol. With eligible women, a counsellor would present information about the benefits, risks, possible side effects and efficacy of the two method options.
Women who chose misoprostol would receive 12 tablets of 200 mcg, along with instructions to insert four tablets (800 mcg) deep in the vagina every 24 hours, over three days. At the time of each insertion, they were instructed to take two 400 mg tablets of ibuprofen orally as prophylaxis against pain and to continue taking one ibuprofen every four hours, according to the level of pain, to a maximum of six to eight tablets per 24 hours (maximum dose 3200 mg/day).
As this was the clinic’s first experience of offering misoprostol, they did not know what to expect in terms of women’s reactions to the treatment. Some of the staff feared that if a woman experienced heavy bleeding or severe pain before the follow-up appointment was due, they might seek assistance from other health care providers, potentially compromising the confidentiality of the clinic. This is why all women were scheduled for follow-up visits 72 hours after administration of the first dose of misoprostol. At that visit, they had a physical examination and trans-abdominal ultrasound to determine whether the abortion was complete, followed by contraceptive counselling.
Attending physicians used three parameters to determine if the abortion was complete: 1) women’s reports of bleeding and expulsion of products of conception, 2) medical examination that showed uterine involution and 3) an ultrasound showing no gestational sac or products of conception. The ultrasound was the most important indicator. If the abortion was incomplete, the attending physician completed the process using electric or manual vacuum aspiration at that visit. All women were scheduled for a follow-up visit 15 days later.
Characteristics of women who chose misoprostol
Most of the 3,225 women who chose to use misoprostol were 20—29 years old (52%), had completed secondary school or had some level of university or technical education (98%), and were either students (38%) or employed (27%). Most were single (70%). About 25% were in steady relationships and about 80% identified themselves as middle class. Most had had no previous induced abortion (68%), and almost all arrived at the clinic in the very early stages of pregnancy, 4—7 weeks of pregnancy (85%) (data not shown). Almost all women (87%) were accompanied during their initial visit to the clinic, most often by their male partners (52%).
Effectiveness of misoprostol
Of the 2,900 women who returned for follow-up, 2,216 (76%) had complete abortions using the clinic-defined criteria at 72 hours after first insertion. Whether completion occurred after the first, second or third dose of misoprostol was not determined, although clinical studies show that a high proportion of women successfully abort after the first dose of 800 mcg administered vaginally.Citation12 Citation15 Citation21 Citation22
Higher percentages of women with the following characteristics had complete abortions after 72 hours post-first insertion: those 15—19 years old (80%), 20—24 years old (78%) or over the age of 35 (78%), university education (80%), single (78%), students (80%) and employees (76%) of higher socio-economic status (81%) and no previous surgical abortions (78%). A higher percentage of those aborting at 4—7 weeks of pregnancy had complete abortions (77%) than those at 8—10 weeks of pregnancy (70%).
Women’s experiences using misoprostol
Women’s descriptions of their experience of misoprostol were obtained through a questionnaire applied to the first 78 women who attended for follow-up. The variables explored were the same as those used in most studies of the acceptability of medical abortion, including pain and bleeding, chills, diarrhoea and vomiting, as well as overall satisfaction with the treatment.
All 78 women reported having experienced some level of pain and bleeding. Most women (91%) felt some pain during the first four hours after vaginal insertion of misoprostol, with the most intense pain coming between the fifth and seventh hour after inserting the first dose. More than half the women (58%) rated the pain as double or more than double than that experienced during menstruation. For most, the pain was worse during the first day and disappeared or diminished significantly during the following days; 16% experienced consistent pain during all three days after inserting the misoprostol.
The majority (60%) reported that bleeding began during the first four hours after the first insertion of misoprostol. Bleeding was most abundant 5—12 hours after the first insertion of misoprostol. 63% said that the amount of bleeding was at least double that of their last menstrual period, and that it diminished or disappeared during the second or third day. Additionally, 60% of the women had chills, 44% had diarrhea, 31% nausea, 23% headache and 10% fever.
Only six women were not satisfied with the treatment; it was not effective for five of them and they felt unsure it would work. The other 72 said they would use it again if they needed an abortion in future and would recommend it to a friend. Regardless of the level of satisfaction, they appreciated the possibility of avoiding a surgical procedure and the fact that misoprostol could be self-administered privately at home. Effectiveness was also mentioned as important. Those who had previously had a surgical abortion highlighted that misoprostol use was “easy,” “simple,” “normal”or “natural”
Discussion
The success rate with misoprostol alone in this Latin American clinic setting was lower than that found in clinical studies where the same dose and route of administration were employed.Citation9, Citation15, Citation21 One key difference is the short amount of time allowed (72 hours) after treatment for completion of the abortion. Medical abortion is a process that takes time, unlike with early surgical methods, where the abortion is complete within a few minutes. It is likely that with more time, perhaps even up to two more weeks, a far greater number of women would have had complete abortions using misoprostol alone. Given that this was the clinic’s first experience using misoprostol for pregnancy termination and that they were working in a legally restrictive setting, clinic staff were concerned to ensure that women had a complete abortion and in some cases, physicians may have used vacuum aspiration even when it was unnecessary.
The relatively low success rate may also be related to other factors, such as the timing and dose of each misoprostol application. Women’s compliance with the treatment protocol was not recorded, but physicians noted anecdotally that women described different experiences with insertion. While most women were probably well able to follow instructions on timing and placing the tablets high in the vagina, others may not have done so. In order to contain costs, tissue extracted through vacuum aspiration is visually inspected but not analysed pathologically, so there are no data on the number of aspirations in which the abortions were actually already complete with misoprostol alone. Finally, there is no way to determine the abortion outcome for women who did not attend for follow-up. However, if it is assumed that all of them had a complete abortion with misoprostol alone, the success rate would go up to 78.8% (2,541 of 3225 women).
The findings regarding acceptability and levels of satisfaction with misoprostol of the 78 women who answered the questionnaire, although the numbers in this case are small, are consistent with findings from other parts of the world, among relatively larger numbers of women, where abortion is legal.Citation9 Citation10 Citation11
The data summarised here allowed clinic staff to discuss ways to modify the protocols so as better to meet the needs of women and address the concerns of providers. For example, because one in every ten women did not return for follow-up, women are now asked to return only at 15 days post-first insertion and greater emphasis is placed by staff on the importance of returning for the follow-up visits. We do not yet have enough data to know whether or not this has resulted in a higher return rate.
Another important change made in the protocols was that if the abortion is not complete at the 15-day follow-up visit, women are given three options: continuing to wait for completion for another week to two weeks, or at that same visit, inserting an additional 800 mcg of misoprostol or undergoing vacuum aspiration.
Conclusions
This paper documents the successful experience of one Latin American clinic in expanding the options available to women who seek early pregnancy termination, ensuring their access to the latest technology. Although working in a legally restrictive environment, clinic staff had the vision and courage to be innovative in their approach to offering women the range of services that exists to meet their needs.
Clinic staff working where abortion is legally restricted face challenges to service delivery that may not exist where abortion legislation is more liberal. For example, in this clinic women are urged not to go elsewhere for follow-up care so that they do not need to explain their situation or answer questions that might be posed by other health care providers, which could raise suspicion or put women in a vulnerable position. As in any high quality health service, staff want to ensure that the outcomes of care are positive. In this setting, in addition, ensuring that women leave the facility with complete abortions is related not only to the quality of care but also to the safety and protection of women and clinic staff. These factors affect the protocols to be used because the law limits possibilities for care.
We conclude that use of misoprostol alone is an important alternative to surgical abortion and to other regimens of medical abortion when mifepristone is not available. Given that this is a legally restricted environment, the high level of satisfaction is a compelling illustration of the extent to which high quality services can be offered despite real and perceived barriers. Misoprostol is being used more widely than ever by women throughout Latin America, oftentimes based on instructions passed along through friends, acquaintances or professionals who may have little information about safe and effective use. Having a clinic where staff are knowledgeable and experienced in its use is particularly important in settings where abortion is stigmatised, unsafe abortion common and access to safe services limited.
Acknowledgements
The authors would like to thank colleagues Dr Barbara Crane and Dr Janie Benson for comments on this manuscript, the health care providers working in the clinic for their vision and commitment, and colleagues in the clinic whose courage propels them to provide safe abortion services to women in a setting with many obstacles.
References
- SK Henshaw, S Singh, T Haas. The incidence of abortion worldwide International Family Planning Perspectives. 25(Suppl.): 1999; S30–S38.
- E Áhman, I Shah. Unsafe Abortion: Global and Regional Estimates of Incidence of Unsafe Abortion and Associated Mortality in 2000. 4th ed, 2004; World Health Organization: Geneva.
- SH Costa, MP Vessy. Misoprostol and illegal abortion in Rio de Janeiro, Brazil Lancet. 341: 1993; 1258–1261.
- PW Ashok, GC Penney, GMM Flett. An effective regimen for early medical abortion: a report of 2000 consecutive cases Human Reproduction. 13(10): 1998; 2962–2965.
- EA Schaff, SL Fielding, C Westhoff. Vaginal misoprostol administered 1, 2, or 3 days after mifepristone for early medical abortion: a randomized trial JAMA. 284: 2000; 1948–1953.
- K Abuabara, J Blum. Providing medical abortion in developing countries: an introductory guidebook. Results of a team residency at the Bellagio Study and Conference Center. 2004; Gynuity Health Projects: New York.
- See http://www.medicationabortion.org/sidebars/misoprostolstudies.html, http://www.ipas.org/english/publications/abortion.asp and http://www.medicationabortion.org/methotrexate/index.html. Accessed 9 December 2004.
- A Bugalho, A Faúndes, L Jamisse. Evaluation of the effectiveness of vaginal misoprostol to induce first trimester abortion Contraception. 53(4): 1996; 243–246.
- JL Carbonell, L Varela, A Velazco. The use of misoprostol for termination of early pregnancy Contraception. 55: 1997; 165–168.
- JL Carbonell, L Varela, A Velazco. The use of misoprostol for abortion at less than or equal to 9 weeks’ gestation European Journal of Contraception and Reproductive Health Care. 2(3): 1997; 181–185.
- JL Carbonell, L Varela, A Velazco. Vaginal misoprostol for late first trimester abortion Contraception. 57(5): 1998; 329–333.
- JL Carbonell, L Varela, A Velazco. Vaginal misoprostol for abortion at 10—13 weeks’ gestation European Journal of Contraception and Reproductive Health Care. 4(1): 1999; 35–40.
- JL Carbonell, J Rodriguez, S Aragon. Vaginal misoprostol 1000 micrograms for early abortion Contraception. 63(3): 2001; 131–136.
- MD Creinin, E Vittinghoff. Methotrexate and misoprostol vs. misoprostol alone for early aborton: a randomized controlled trial JAMA. 272: 1994; 1190–1195.
- JK Jain, KR Meckstroth, DR Michell Jr. Early pregnancy termination with intravaginally administered sodium chloride solution-moistened misoprostol tablets: historical comparison with mifepristone and oral misoprostol American Journal of Obstetrics and Gynecology. 181(6): 1999; 1386–1391.
- A Velazco, L Varela, R Tanda. Misoprostol for abortion up to 9 weeks’ gestation in adolescents European Journal of Contraception and Reproductive Health Care. 5(4): 2000; 227–233.
- K Blanchard, B Winikoff, K Coyaji. Misoprostol alone: a new method of medical abortion? JAMWA. 55(3 Suppl.): 2000; 189–190.
- K Blanchard, B Winikoff, C Ellertson. Misoprostol used alone for the termination of early pregnancy: a review of the evidence Contraception. 59(4): 1999; 209–217.
- World Health Organization. Safe Abortion: Technical and Policy Guidance for Health Systems. 2003; WHO: Geneva.
- Consensus Statement: Instructions for Use — Abortion Induction with Misoprostol in Pregnancies up to 9 Weeks LMP. Expert Meeting on Misoprostol sponsored by Reproductive Health Technologies Project and Gynuity Health Projects. Washington DC, 28 July 2003. At: www.gynuity.org. Accessed 30 August 2004.
- JK Jain, B Harwood, KR Meckstroth. Early pregnancy termination with vaginal misoprostol combined with loperamide and acetaminophen prophylaxis Contraception. 63(4): 2001; 217–221.
- JK Jain, C Dutton, B Harwood. A prospective randomized, double-blinded, placebo-controlled trial comparing mifepristone and vaginal misoprostol to vaginal misoprostol alone for elective termination of pregnancy Human Reproduction. 17(6): 2002; 1477–1482.