Abstract
A third of adolescent girls in South Africa become pregnant before the age of 20, despite contraception being free and mostly accessible. This qualitative study was undertaken in Limpopo Province in 1997 on the barriers to adolescent girls accessing clinic services for contraception. Thirty-five in-depth interviews and five group discussions were conducted with girls aged 14—20, and interviews with nursing staff at 14 clinics. Many of the girls described pressure from male partners and family members to have a baby or prove their fertility. Other barriers to sustained contraceptive use included medically inaccurate notions about how conception occurs and fears about the effects of contraception on fertility and menstruation, which were not taken seriously by nurses. Nurses' attempts to stigmatise teenage sexuality, their scolding and harsh treatment of adolescent girls, and their unwillingness to acknowledge adolescents' experiences as contraceptive users, undermined the effective use of contraception by girls. Youth need better information on reproductive physiology and sexual health, and detailed information on contraception. Tools to enhance the accuracy and availability of knowledge in the clinic setting have a role, but need to be introduced along with initiatives to ensure that services are adolescent-friendly and do not stigmatise adolescent sexual activity.
Résumé
En Afrique du Sud, un tiers des adolescentes sont enceintes avant l'âge de 20 ans, malgré la gratuité et l'accessibilité de la contraception. Cette étude qualitative, réalisée dans la province de Limpopo en 1997, a analysé les obstacles empêchant les adolescentes d'accéder aux services de contraception. Elle a mené 35 entretiens et 5 discussions de groupe avec des jeunes filles de 14 à 20 ans, et des entretiens avec des infirmières dans 14 dispensaires. Beaucoup d'adolescentes ont décrit les pressions de leurs partenaires et des membres de la famille qui les incitent à avoir un bébé ou à prouver leur fécondité. L'utilisation suivie de contraceptifs était aussi entravée par des notions erronées sur la conception et des craintes quant aux conséquences de la contraception sur la fécondité et les menstruations, que les infirmières ne prenaient pas au sérieux. Les tentatives des infirmières de stigmatiser la sexualité des jeunes, leurs réprimandes, leur brusquerie et leur refus de tenir compte des expériences des adolescentes comme utilisatrices de contraceptifs contrariait l'utilisation efficace de la contraception chez les adolescentes. Les jeunes doivent être mieux informés de la physiologie reproductive, de la santé génésique et de la contraception. Des outils pour améliorer la fiabilité et la disponibilité de connaissances dans les dispensaires jouent un rôle, mais doivent être introduits parallèlement à des initiatives pour que les services soient adaptés aux adolescents et ne stigmatisent pas l'activité sexuelle des adolescents.
Resumen
Una tercera parte de las adolescentes en Sudáfrica quedan embarazadas antes de cumplir los 20 años, pese a que los anticonceptivos son gratis y accesibles. Este estudio cualitativo sobre las barreras que enfrentan las adolescentes al intentar acceder a los servicios clínicos de anticoncepción, se llevó a cabo en la Provincia Limpopo, en 1997. Se realizaron 35 entrevistas a profundidad y cinco discusiones en grupo con mujeres jóvenes entre 14 y 20 años, así como entrevistas con el personal de enfermería de 14 consultorios. Muchas de las jóvenes informaron presión de sus parejas y familiares para tener un bebé. Otras barreras al uso sostenido de anticonceptivos fueron: creencias erróneas sobre cómo ocurre la anticoncepción y temores sobre los efectos de anticonceptivos en la fertilidad y la menstruación, las cuales las enfermeras no tomaron en serio. Los efectos de los intentos de las enfermeras de estigmatizar la sexualidad de las jóvenes, sus regaños y trato duro de las mismas, y su renuencia a reconocer las experiencias de éstas como usuarias de anticonceptivos, debilitaron el uso eficaz de la anticoncepción por parte de las jóvenes. La juventud necesita mejor información sobre la fisiología reproductiva y la salud sexual, y datos detallados sobre los anticonceptivos. Las herramientas para mejorar la exactitud y disponibilidad del conocimiento en el ámbito clínico desempeñan un papel, pero se deben introducir junto con iniciativas para garantizar que los servicios sean amigables a las adolescentes y no estigmaticen su actividad sexual.
Research indicates that many young South Africans engage in sexual risk-taking, including early initiation of sexual activity, unprotected sex, and low levels of condom and contraceptive use, and often have concurrent partners.Citation1Citation2Citation3Citation4 Among sexually active black African women aged 15–24 years in South Africa, the prevalence of current modern contraceptive use is 64.4%. This may explain the 35% decline in childbearing amongst adolescent girls seen from the late 1980s to the late 1990s. Nonetheless, 35% of women experience pregnancy before the age of 20,Citation5 which is still a very substantial proportion for this age group.
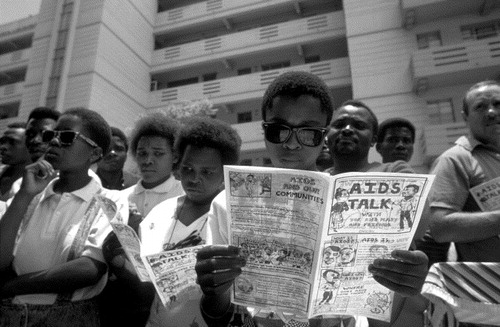
The decline in the proportion of adolescent girls giving birth is not visible to staff in health facilities because concomitant population growth has resulted in the absolute number of adolescent girls giving birth appearing to increase. Adolescent pregnancy is still regarded as a particularly taxing and intractable problem by many working in the health sector. All the more so because contraception is provided free of charge in a clinic-based programme whose national coverage is extensive, with mobile clinics serving most rural areas. Social and public health concern about adolescent sexuality and pregnancy has been heightened by the realisation that this age group is in the forefront of the HIV-AIDS epidemic, with the latest national seroprevalence survey indicating that 15.8% of pregnant women aged less than 20 years are infected.Citation6
Research on contraception in South Africa points to a number of barriers to effective use. Historically, the contraceptive service was developed within a political context of population control, with the emphasis on contraceptives which required minimal user involvement, notably injectable contraceptives; these remain the most commonly used method.Citation7Citation8 The 1998 Demographic and Health SurveyCitation5 found that 64.5% of black African women started contraceptive use with injectables and 23.4% with oral contraceptives, while among white women 5.0% started with injectables and 65.3% with oral contraceptives. There are two injectable progestogen-only contraceptives commonly used in public clinics, delivered by two- or three-monthly injections, always referred to by their brand names Nur-Isterate and Depo Provera respectively. Researchers have pointed to the broader social, economic and educational inequalities in the country in explaining racial differences in patterns of contraceptive use.Citation3Citation8 Other factors include the negative experiences of using services of many South African adolescents,Citation7Citation9Citation10 the role of gender inequalities and multiple forms of coercion in undermining women's capacity for making autonomous decisions about controlling their fertility (necessitating the use of contraceptive methods such as the injections that are easy to conceal),Citation4Citation11Citation12 and the importance to many of displaying fertility early.Citation13Citation14
Research methods and setting
The aim of this research was to gather information that could be used to improve access to and overall quality of contraceptive services for adolescent women in Limpopo Province. This province is located in the far north of the country and remains one of the poorest in South Africa. The research was mostly conducted in the semi-rural areas surrounding the main town. A network of integrated clinics in urban and semi-rural areas provide primary health care services.
A total of 35 individual, semi-structured interviews and five group discussions with groups of three to six informants were conducted with adolescent girls aged 14—20, who were recruited from either clinic waiting rooms or schools. Recruitment was opportunistic; exclusion criteria were not employed, except for age. The number of people interviewed was determined by the budget and focus of the study, and the point beyond which new ideas were no longer emerging with respect to the main areas of inquiry. In addition, individual and group interviews were conducted with nurses involved in contraceptive provision (to all ages) and working in the area from which the adolescents were recruited. Ten of the nurses were based in a semi-rural area, three in clinics in a township, and one in a clinic in the main town. Those interviewed were either those on duty when the clinic was visited or those who were said to see more adolescents for contraception. They were aged 30—50 and were all from the same or similar ethnic and cultural background as the adolescents.
Ethical approval for the study was given by the South African Medical Research Council's Ethics Committee. All participants gave verbal informed consent, were given a written participant information sheet and informed of the confidentiality of the research. Nurses were not involved in the recruitment of informants, and those young women who chose not to participate in the study were assured that this would not affect their health care in any way.
Interviews with the adolescent girls were conducted in the local language, Pedi, and those with the nurses in English. The first author conducted fieldwork over a three-week period, working with a local interpreter who was a female nurse with positive and non-judgmental attitudes towards adolescents. Interviews were tape-recorded after informed consent had been obtained (and taped), the data were transcribed and translated into English and a thematic analysis was carried out. The scope of inquiry covered the following areas: What were the circumstances of and influences on girls' contraceptive-seeking practices and decision-making? What were the barriers to access and how might they be overcome? What contraceptive methods were considered to be appropriate for adolescent girls and why? Which methods were actually available, which were (not) offered, (not) recommended and why (not)? What were the contextual factors that impinged on patterns of contraceptive use, including sexual circumstances and attitudes towards pregnancy? Questions were tailored for each individual interview.
Of the 35 girls who were interviewed individually, 25 had used contraception at some time. Twenty-two had used injectable contraceptives (mostly Nur-Isterate), and three oral contraceptives (two of them because of experiences with side-effects of Nur-Isterate). Of the 35, 14 had already had a child, of whom six had never used contraception. Two informants were not yet sexually active. None were married, which reflects the fact that teenage marriage is very unusual; in fact only 1.2% of South African girls aged 15—19 years are married.Citation5
Findings
Pressure to prevent, pressure to conceive
In negotiating their sexuality and contraceptive use, girls reported experiencing pressure and coercion from several sources. They were not able to take decisions on contraceptive use and pregnancy prevention as autonomous individuals. This was clearly a highly contested domain in which a range of players held strong views and sought to impose them, often forcefully, on the girls. Nurses often tried to force the girls to use injectables, which they perceived as the most reliable form of contraception. The nurses described the girls as “stubborn” as they did not heed admonitions to abstain from sex. Some mothers also reportedly tried to impose contraception on their daughters, taking them to clinics for contraception as soon as they started menstruating. These pressures were accepted or resisted, depending on whether the adolescents felt their own needs and concerns were being addressed or not. However, many adolescent girls voluntarily initiated contraceptive use, in some cases before first sex, often as a result of peer pressure to use contraception, and in some instances encouraged by male sexual partners.
On the other hand, there was often pressure to get pregnant at an early age. Many girls described the importance of proving fertility – described as having a “strong snake in the womb” – in order to attain status and acceptance as a woman, a view reportedly held by significant others in their lives. In some families, encouragement to have a child very young was overt, sometimes motivated by grandmothers who wanted a baby to keep them company. This likely reflects a historical institutionalisation,Citation2Citation13Citation15Citation16 if not explicit public acceptance, of pre-marital pregnancy and the routine arrangement of childcare within the extended family.
At the same time, fears that contraception could cause infertility were widespread. Preachers at local African churches reportedly preached that contraceptive use “punctures and spoils the eggs”. Some nurses also seemed to give information that supported this view. One nurse explained:
“We tell them: ‘You might get pregnant, you might not get pregnant’ [after injectable contraceptive use], and say that ‘Sometimes it may be because of the development of your reproductive system, sometimes because you used the injection’.”
Several adolescent mothers described how their own mothers had not allowed them to use contraception in case it caused permanent infertility, and had actively encouraged them to get pregnant. They often complained that contraception made them sick, and of “waist pains” after sex, weight loss, diminished sexual feeling because of vaginal wetness and fears of being condemned (i.e. made infertile).
Young women's sexual partners reportedly also often wanted to prove their fertility by fathering a child, and pregnancy was associated with proving love and commitment. Rather than directly raising this issue, some male partners were reported by girls to use manipulative tactics to try to get them to stop contraceptive use. Some boyfriends reportedly demanded that contraception be stopped, at times threatening to use, or using, physical violence to enforce this, or tearing up the clinic card and throwing away the pills. As a result of this coercion, some girls became pregnant, while others used contraception secretly.
Traditional contraceptives practices and medically inaccurate ideas about conception
When mothers and nurses tried to force girls to use contraception, their high expectations of obedience and respect often resulted in them paying little attention to the girls' need for information and to take their concerns seriously. The girls interviewed said they had been provided with at most very little and vague information about menstruation, or sexual matters, by mothers, other relatives, or teachers. Some adolescents described friends as important sources of information about contraceptive methods, and reported occasionally visiting the clinic in small groups and giving each other advice. However, lack of access to medical information on the reproductive system provided space for medically inaccurate notions about the conditions necessary for conception. These led some girls to think they were not at risk of pregnancy, for example, that the blood of each sexual partner had to “get used to” that of the other through a series of sexual encounters, before conception could occur. There was a related belief that if a woman has multiple partners and alternates them regularly, conception cannot take place because “the blood is different” each time.
Knowledge was widespread about local traditional and religious methods of contraception, such as tying a rope containing traditional medicines around the waist, mixing a cloth covered in the woman's menstrual blood with medicines from a traditional healer and burying it, and drinking tea or concoctions prayed over by religious leaders. Another method mentioned by some young women was “prevention by menstruation”, which they explained consisted of abstaining from sex in the second half of the cycle (before and during menstruation), which they perceived as the time of greatest risk of conception. The girls we interviewed said they did not use these methods themselves, but believed they were effective, explaining that pregnancy would only occur if the traditional medicine had lost its strength. In recent, unpublished research from another part of South Africa we have found such methods quite commonly used by adolescents and the widespread belief that conception is most likely to occur during menstruation.
Nurses told us that some adolescents took contraceptive pills only when their sexual partner came to visit them, or only on half the required days, to reduce the chances of gaining weight. If pills were missed, nurses said they were sometimes taken all at once, which is in keeping with practices documented in other parts of the country of taking a whole packet of pills to induce abortion.Citation17 Most adolescents we discussed the pill with were under the impression, reinforced by nurses, that forgetting to take one pill would result in pregnancy.
At the time of the research, most informants had little experience of using condoms and were concerned that they could be left inside the vagina or womb, and would then have to be removed by a doctor in hospital. This idea has also been found by the authors amongst adolescents in another part of the country.
Blood blockages: absence of menstruation and injectable contraception
Most of the girls using injectable contraceptives reported having experienced menstrual irregularities, which often resulted in them stopping contraceptive use, as the nurses did not usually allow them to change methods. Changing methods was reserved for cases where the nurses perceived there was a medical problem, a “real” problem. Prolonged absence of menstruation meant that girls did not know whether or not they were pregnant. Menstruation was also widely seen as cleansing the womb of accumulated “dirt”.Citation18 One informant explained irregular menstruation as follows:
“A woman has two tubes which they say release the menstruation, but sometimes only one tube releases it [the blood], and if this is the case it can't release it every month.”
The majority of informants described this state of “blockage” as a dangerous condition, identified by “dark clots” or by “waist pains”, and construed it either as an indication, or cause of, illness. Some said that not menstruating was itself the sickness, and explained that it meant the injectable was “not good for the blood”. Remaining in such a blocked state was perceived to cause a multitude of other symptoms, including abdominal discomfort, bodily swelling, headaches (the blood was “blocked in the head”), tiredness, sores on the body, infections, weight gain and skin changes, in particular a bluish tinge which demonstrated that the blood had withdrawn somewhere. Bodily swelling was interpreted by one teenager to be caused by blood that would “normally stay in the abdomen to make a baby” descending to the legs or other parts of the body. Blood blocked somewhere in the body might eventually “come out too fast”, with adverse effects. Two stories were narrated of cases where women were said to have literally collapsed and bled to death because the blood had come out too fast.
Infertility was related to these blood blockages. One explanation was that blood accumulated in the abdomen and caused the womb “to get tired”, potentially preventing pregnancy, sometimes permanently. Another girl explained the process as follows:
“If you're not on the injection, the blood stays somewhere next to the womb, and if you don't conceive that month, the blood can get out; but if you use Nur-Isterate, this blood doesn't pass easily to the place next to the womb, and it means your body will never be as it was before, and this blood prevents you from ever falling pregnant.”
The majority of girls thought of this infertility as a temporary state, and explained that after two or three years the injection could be “still in your body” or, alternatively, that it would take the same length of time to conceive after stopping the injection as the time spent on it.
Anxiety about missing menstrual periods led to erratic patterns of contraceptive use, which the girls justified as needing to “wait for the blood to come out”. One girl had adopted a pattern whereby she used the injection for three months at a time, and then had a three-month break so that she would menstruate. Menstruating excessively was another reported side effect of injectable contraception, leading to a concern expressed by one informant that her blood would eventually be “finished”.
Stigmatising adolescent sex
As regards management of contraceptive side effects, there was a substantial mismatch between the needs and expectations of adolescent contraceptive users, and the concerns and practices of nurses. Nurses generally felt very uncomfortable giving contraception to adolescent girls, particularly younger ones, whom they invariably thought of as “children”. They perceived that sex was starting at a younger and younger age, and that the easy availability of contraception encouraged this. They expressed concern about the consequences of early pregnancy, especially girls dropping out of school early, and deepening poverty in families.
“It worries me a lot to see such small children getting involved at an early age exposing themselves to diseases, it touches me a lot.”
As a result of these concerns, nurses said they often tried to influence the adolescents not to have sex when they came for contraception. As one explained: “You start by giving them lectures about the dangers of early sex before they can convince you to give them what they want.” Another said nurses would tell adolescents that contraceptive use did not mean that they must go “running around” with many partners, but that they should “stick to normal morals”. Nurses perceived as problematic adolescents' purported attitude that sex was a “game”, describing this as symptomatic of ignorance and a lack of concern about the consequences.
The adolescents confirmed what the nurses said, explaining that the nurses would not provide contraception until they had asked “funny questions” about whether they had boyfriends, why they had sex so young, whether they had told their mothers and why they wore mini-skirts, had lectured them on being too young for sex and told them to stop going around with men. Those who refused to answer these questions were scolded, and made to feel ashamed and afraid. The girls unanimously reported that they could not stand up to the nurses, who were older and expected to be respected, and because they needed their services.
“We just feel ashamed but we don't challenge them. Sometimes you may challenge them and find that you use words which may hurt them, then next time you go there, you find they refuse to help you.”
Asked whether the comments and lectures on the dangers of early sex would prevent girls from attending clinic one nurse said: “They enjoy it, they're not afraid, as long as you are not harsh with them.” Others admitted that even if their “lectures” were a barrier to access, they still felt obliged to provide them.
Stigmatising adolescent sex was a barrier to accessing contraceptive services, but most nurses did not identify their actions as contributing to the reinforcement of this stigma. We were told that a reluctance to accept the tainted identity of girls who are not virgins was a barrier to service use. Contraception could not be accessed without accepting that it was needed, and seeking contraception amounted to a form of public admission of sexual activity. As one nurse put it: “It's her secret, and it's a scandal for nurses to know.” A perception that youth sexuality was stigmatised was reinforced, both by the action of the nurses as well as by older women in clinic waiting rooms, who were said to pass remarks.
Scolding nurses and adolescent retaliation: dynamics of power in rural contraceptive services
Experiences of “harassment” by nurses emerged as a strong theme in the narratives of adolescent informants, even in interviews held in side rooms in clinics, which potentially could have inhibited frank discussion of these concerns. Nurses were commonly described by adolescents as rude, short-tempered and arrogant.
Legally, parental permission is not needed for minors to be given contraception, but some nurses felt uncomfortable with this, and also feared repercussions from irate parents. This was especially a problem in settings like that of our study, where communities are small and churches that oppose contraceptive use influential. Staff therefore did not always follow official policy, although they indicated that they would generally provide a method to an adolescent whose mother disagreed or did not know. However asking for parental permission was potentially a barrier to access and certainly occurred, e.g. one girl we interviewed had been told to come back with her mother.
Adolescents spoke of being scolded by nurses for many things, including if they had got previous doses of contraception from a (private) general practitioner, or had used a fixed clinic when their home was serviced by a mobile clinic, or for not arriving at the clinic early in the morning (despite the fact that, for most, visiting the clinic was only feasible after school hours). Clinic cards also constituted an important area of struggle. Most nurses complained that some girls tampered with their clinic cards and, in particular, changed the dates and forged the nurses' signatures if they were late for their return date, to avoid scolding. One nurse called this “not knowing that they are cheating themselves”. Another nurse explained that some girls used “forgery” as a strategy for resisting mothers who forced them to use contraceptives against their will. Nurses described this as truanting and even criminal behaviour, which made them feel fed up and offended, and they told the girls so. Some of the adolescents told us that if they were late for the return date because they were busy, forgot or were away, or if they had lost or damaged their clinic card, sometimes they would stop contraception for a while rather than face scolding from staff. They might also, one of the nurses mentioned, share oral contraceptives with friends rather than come to the clinic themselves.
Although termination of pregnancy has been legal in South Africa since February 1997 (before this research was conducted) and emergency contraception was supposed to be available in clinics, nurses were adamant that they should not be “tricked” into providing emergency contraception as an abortifacient. This is in keeping with the widespread resistance of nurses to having any involvement in abortion, or even providing information about it.Citation17 Nurses also reported that some girls would request the injectable or less commonly “the red pills” ( emergency contraception) if they suspected they were pregnant, believing that these would make them abort. Although it was not medically necessary, clinics had a rule that a woman could only be given the injection when menstruating, so that nurses could be sure they were not pregnant. Nurses reported that adolescents would borrow the soiled sanitary towels of friends, or put beetroot juice or blood from a pricked finger onto a pad, to try and convince the nurses that they were actually menstruating. They explained that they could often detect such cases from the adolescent's behaviour: “These ones will be aggressive, she just forces you to inject her, or she may cry.”
Whilst many of the girls felt powerless to respond to nurses in the clinic, some seem to have retaliated when they met the nurses in the community. Nurses complained of this.
“They [the girls] are cooperative in the clinic but outside they'll start pointing at you, saying ‘There's that woman who was asking all those questions.’ You try to ignore them, but then the others will say ‘Hey! she can't ask all those questions’, and then you feel small because you are outside the clinic.”
Most importantly, however, the combined effects of nurses' attempts to stigmatise teenage sexuality, their scolding and harsh treatment of adolescent girls, and their unwillingness to acknowledge adolescents' experiences as contraceptive users, undermined the effective use of contraception by the girls.
Discussion
Adolescent pregnancy remains an important problem in South Africa. Although rates are declining,Citation5 they are still very high and most teenagers still report that their pregnancies are, at least at some level, unwanted. Most of the girls interviewed in this study were using contraception, but had not done so continuously in the past, and several had become pregnant as a result. In some cases, a problematic experience at the clinic had led to an immediate decision never to return. Other barriers assumed lesser or greater importance, depending on the circumstances. Problems such as contraceptive side effects might be tolerated for a while but later contraceptive use might be stopped, even if temporarily. Similarly, nurses' scolding was sometimes managed by girls through attending clinic in groups, while it might be an absolute barrier for other girls who came alone, or who were perhaps younger or more vulnerable.
Caution is needed with regard to generalising our findings. We do not know whether the same sorts of attitudes and experiences prevail amongst adolescent girls and family planning nurses in Limpopo Province today. However, our research in the rural Eastern Cape over the last three years has found very similar ideas about conception among girls, widespread use of “traditional” contraceptives, irregular patterns of modern contraceptive use and reports of scolding nurses.Citation19 Thus, we have reason to believe that our findings remain pertinent, and that interventions are still needed.
Our study identified pressure on adolescent girls to conceive as one of the factors underlying the high adolescent pregnancy rate. Although there is a dominant discourse in the health sector about the problem of adolescent pregnancy, our research suggests that some of the influential figures in adolescents' lives see adolescent pregnancy as desirable. However, this observation is in conflict with other research, that most teenage mothers did not want their pregnancy at the time.Citation5 This points to the shifting nature of “wantedness” of adolescent pregnancies, which was remarked upon by Jewkes et al.Citation2 It seems unlikely that there will be a more unified view of the undesirability of teenage pregnancy in communities until more widespread further education and employment opportunities for youth engender a convergence of ideas about the social and other costs of teenage pregnancy. Meanwhile, a proportion of adolescent pregnancies are not likely to be preventable, even with improved health services.
One of the barriers to effective contraceptive use was limited and inaccurate knowledge of reproductive anatomy and physiology. This has been found in much previous research,Citation4Citation14 and reflects a lack of general knowledge and a failure of tuition in schools. There have been recent efforts to improve this area of the curriculum and teaching in South Africa, but there is considerable evidence that it remains unsatisfactory and is often provided only after adolescents have become sexually active.Citation20 Our findings reinforce the need to provide information to teenagers before sexual activity commences, which is usually from age 14.Citation3Citation14Citation21 We would also suggest that there is a need to actively refute common erroneous local beliefs.
There is good evidence that high quality care in contraception services results in continued use of contraception.Citation22Citation23 Women who are given more information and better counselling on side effects are less likely to discontinue use.Citation24Citation25Citation26 Young women need better information on contraception, whether provided as part of reproductive and sexual health education in schools, through other media or by health facilities. This should address common concerns about contraceptive side effects and how these can be managed without jeopardising contraceptive effectiveness. Our findings also suggest that nursing staff in contraceptive services may have gaps in their education and knowledge of contraceptive use and management of side effects. In particular, in a context of injectable contraceptive use, the difference between infertility and contraception-induced delay in return to fertility needs to be better understood and communicated. In this setting, the most common cause of infertility is sexually transmitted infections, and their prevention also needs to be communicated effectively.
Dealing effectively with contraceptive side effects is an area of clinical practice which requires good listening and communication skills, but also a particular attitude towards adolescents and the role of nurses. Whilst the rigidity we observed in nurses' responses to side effects may partly indicate a lack of confidence and inadequate training, it also reflects a hierarchical approach to nurse–patient relationships that makes it difficult for nurses to talk with girls on their terms. It may also reflect the use of scare tactics in an attempt to dissuade adolescents from having sex. In the Eastern Cape province, Mathai taped contraceptive user–nurse consultations and showed that very little of the available time was spent discussing how to use methods, known side effects or why symptoms occur.Citation27 Training for contraceptive providers needs to equip them with a more empowering, problem-solving approach, but also needs to address roles and attitudes with respect to their patients. The World Health Organization has developed a tool for family planning providers to address these issues.Citation29 However it will only be effective if providers are orientated attitudinally towards providing information and empowering girls needing contraception. The National Adolescent-Friendly Clinic Initiative in South Africa is an example of a programme that has sought to improve contraceptive services for young women by making them more accessible and acceptable.Citation9 Its effectiveness, however, needs to be established.
The judgmental approach of some health care providers in South Africa has acted as a barrier to the use of a range of facilities.Citation9Citation17Citation28Citation30Citation31 That the nurses in this study thought it was wrong for adolescents to be having sex affected their actions in clinical encounters. Despite believing that adolescent pregnancy was a problem that should be prevented, the nurses did not feel good about providing contraception to girls. Their attempts to discourage youth sex appeared to further stigmatise sexual activity and act as a barrier to contraceptive use. The gap between nurses' personal politics (reflecting wider social norms), and public health imperatives is an important challenge for health services, as it jeopardises the delivery of high quality, effective services. It also raises important questions about professional socialisation, training, supervision and development of nursing staff. Interventions such as the workshop series Health Workers for Change can play an important role in helping staff to address some of these issues.Citation32
This research was conducted before the loveLife campaigns (<http://www.lovelife.org.za>) were initiated in South Africa. One of the aims of loveLife has been to reduce stigma associated with teenage sexuality and establish that since most adolescents are sexually active (almost all by the age of 20), it is important to acknowledge it, to provide accurate information about sex and enable sexual activity to be safe. We do not know what impact such campaigns have had on teenage girls' perceptions of being sexually active. Our findings, however, suggest that a programmatic goal of this nature would be appropriate and could make a positive contribution to improving contraceptive access and use.
Acknowledgements
This research was funded by the Reproductive Health Research Fund of the Health Systems Trust, and would not have been possible without the young women and clinic nurses who participated. Joyce Maepa was interpreter, co-interviewer and translated and transcribed tape interviews. Dr Lloyd Kaseke, the nursing Services Department of Mankweng Hospital and Limpopo Province Department of Health Research Committee, provided access to the site and facilitated the research. We would like to thank Peter Aggleton for his comments on the manuscript.
References
- G Buga, D Amoko, D Ncayiyana. Sexual behaviour, contraceptive practices and reproductive health among school adolescents in rural Transkei. South African Medical Journal. 86: 1996; 523–527.
- R Jewkes, C Vundule, F Maforah. Relationship dynamics and adolescent pregnancy in South Africa. Social Science and Medicine. 52(5): 2001; 733–744.
- C Kaufman, S Clark, N Manzini. Communities, opportunities and adolescents' sexual behaviour in KwaZulu-Natal, South Africa. Studies in Family Planning. 35(4): 2004; 261–274.
- C Varga. Sexual decision-making and negotiation in the midst of AIDS: youth in KwaZulu/Natal, South Africa. Health Transition Review. 7(Suppl. 3): 1997; 45–67.
- Department of Health. South Africa Demographic and Health Survey. 1999; Department of Health: Pretoria.
- Department of Health. National HIV and syphilis antenatal sero-prevalence survey South Africa 2003. 2004; Department of Health: Pretoria.
- O Chimere-Dan. Contraceptive prevalence in South Africa. International Family Planning Perspectives. 22(1): 1996; 4–9.
- S Burgard. Factors associated with contraceptive use in late- or post-apartheid South Africa. Studies in Family Planning. 35(2): 2004; 91–104.
- K Dickson-Tetteh, A Pettifor, W Moleko. Working with public-sector clinics to provide adolescent-friendly services in South Africa. Reproductive Health Matters. 9(17): 2001; 160–169.
- Z Mfono. Adolescent contraceptive needs in urban South Africa: a case study. International Family Planning Perspectives. 24(4): 1998; 180–183.
- K Wood, F Maforah, R Jewkes. “He forced me to love him”: putting violence on the adolescent sexual health agenda. Social Science and Medicine. 47: 1998; 233–242.
- C Varga. How gender roles influence sexual and reproductive health among South African adolescents. Studies in Family Planning. 34(3): 2003; 160–172.
- E Preston-Whyte. Culture, context and behaviour: anthropological perspectives on fertility in Southern Africa. South African Journal of Demography. 2(1): 1998; 13–23.
- L Richter. A survey of reproductive health issues among urban Black youth in South Africa. 1996; Society for Family Health: Pretoria.
- JC Caldwell, P Caldwell. The South African fertility decline. Population and Development Review. 19(2): 1993; 225–262.
- E Preston-Whyte, M Zondi. African teenage pregnancy: whose problem?. S Burman, E Preston-Whyte. Questionable Issue: Illegitimacy in South Africa. 1992; Oxford University Press: Cape Town, 226–246.
- R Jewkes, T Gumede, M Westaway. Why are women still aborting outside designated facilities in metropolitan South Africa?. British Journal of Obstetrics and Gynaecology. 112(5): 2005; 1236–1242.
- R See Jewkes, K Wood. Problematizing pollution: dirty wombs, ritual pollution and pathological processes. Medical Anthropology. 18: 1999; 163–186.
- R Jewkes, M Nduna, J Levin. A cluster randomised controlled trial to determine the effectiveness of Stepping Stones in preventing HIV infections and promoting safer sexual behaviour amongst youth in the rural Eastern Cape, South Africa: trial design, methods and baseline findings. Tropical Medicine & International Health. 11: 2006; 3–16.
- N Manzini. Sexual initiation and childbearing among adolescents in KwaZulu Natal, South Africa. Reproductive Health Matters. 9(17): 2001; 44–52.
- C Vundule, NF Maforah, R Jewkes. Risk factors for teenage pregnancy amongst African adolescents in metropolitan Cape Town: a case control study. South African Medical Journal. 91: 2001; 73–80.
- S Rama Rao, M Lacuesta, M Costello. The link between quality of care and contraceptive use. International Family Planning Perspectives. 29(2): 2003; 76–83.
- MA Koenig, MB Hossain, M Whittaker. The influence of quality of care upon contraceptive use in rural Bangladesh. Studies in Family Planning. 28(4): 1997; 278–289.
- N Cotton. Early discontinuation of contraceptive use in Niger and the Gambia. International Family Planning Perspectives. 18(4): 1992; 145–149.
- Z-W Lei, SC Wu, RJ Garceau. Effect of pretreatment counseling on discontinuation rates in Chinese women given depot-medroxyprogesterone acetate for contraception. Contraception. 53: 1996; 357–361.
- D Patel. The effects of service quality on IUD continuation among women in rural Gujarat. MA Koenig, ME Khan. Improving Quality of Care in India's Family Welfare Programme: The Challenge Ahead. 1999; Population Council: New York, 333–345.
- M Mathai. A study of the knowledge and problem-solving ability of family planning nurses in Mdantsane. Unpublished thesis, Master of Philosophy (Maternal and Child Health). 1997; University of Cape Town.
- Q Abdool-Karim, E Preston-Whyte, S Abdool-Karim. Adolescents seeking condoms at family planning services – Part 1. A user's perspective. South African Medical Journal. 80: 1992; 301–302.
- World Health Organization and John Hopkins Bloomberg School of Public Health Center for Communication Programs, Information and Knowledge for Optimal Health (INFO). Decision making tool for family planning clients and providers. 2005; WHO: Geneva. At: <http://www.who.int/reproductive-health/family_planning/counselling.html. >.
- R Jewkes, N Abrahams, Z Mvo. Why do nurses abuse patients? Reflections from South African obstetric services. Social Science and Medicine. 47: 1998; 1781–1795.
- C Kaufman, T de Wet, J Stadler. Adolescent pregnancy and parenthood in South Africa. Studies in Family Planning. 32(2): 2001; 147–160.
- C Vlassoff, S Fonn. Health Workers for Change as a health system management and development tool. Health Policy and Planning. 16(Suppl. 1): 2001; 47–52.