Abstract
From a policy and programmatic point of view, this paper reviews the literature on the fertility-related needs of women and men living with HIV and how the entry points represented by family planning, sexually transmitted infection and HIV-related services can ensure access to contraception, abortion and fertility services for women and men living with HIV. Most contraceptive methods are safe and effective for HIV positive women and men. The existing range of contraceptive options should be available to people living with HIV, along with more information about and access to emergency contraception. Potential drug interaction must be considered between hormonal contraception and treatment for tuberculosis and certain antiretroviral drugs. Couples living with HIV who wish to use a permanent contraceptive method should have access to female sterilisation and vasectomy in an informed manner, free of coercion. How to promote condoms and dual protection and how to make them acceptable in long term-relationships remains a challenge. Both surgical and medical abortion are safe for women living with HIV. To reduce risk of vertical transmission of HIV and in cases of infertility, people with HIV should have access to sperm washing and other assisted conception methods, if these are available. Simple and cost-effective procedures to reduce risk of vertical transmission should be part of counselling for women and men living with HIV who intend to have children. Support for the reproductive rights of people with HIV is a priority. More operations research on best practices is needed.
Résumé
A partir du point de vue des politiques et des programmes, cet article fait une revue des publications sur les besoins liés à la fécondité des femmes et des hommes vivant avec le VIH et comment les points d'entrée que sont les services de planification familiale, de traitement des IST et du VIH peuvent garantir l'accès aux services de contraception, d'avortement et de procréation aux femmes et aux hommes vivant avec le VIH. La plupart des méthodes contraceptives sont sûres et efficaces pour les femmes séropositives. Toutes les options contraceptives devraient être disponibles pour les personnes séropositives, avec davantage d'informations sur la contraception d'urgence et un accès à cette intervention. Il faut envisager l'interaction potentielle des médicaments entre la contraception hormonale et le traitement de la tuberculose ou certains antirétroviraux. Les couples vivant avec le VIH qui souhaitent utiliser une méthode permanente de contraception doivent avoir accès à la stérilisation féminine et la vasectomie, en connaissance de cause et sans coercition. Il demeure difficile de promouvoir le préservatif et la protection double, et de les faire accepter dans des relations à long terme. L'avortement chirurgical et médicamenteux est sûr pour les femmes séropositives. Pour réduire le risque de transmission verticale du VIH et dans des cas de stérilité, les personnes séropositives doivent avoir accès au lavage du sperme et autres méthodes de procréation assistée, si elles sont disponibles. Des procédures simples et rentables doivent être présentées dans les conseils aux femmes et hommes vivant avec le VIH qui souhaitent avoir des enfants. Le soutien des droits génésiques des personnes séropositives est une priorité. Il faut davantage de recherches opérationnelles sur les meilleures pratiques.
Resumen
Desde el punto de vista de políticas y programas, este artículo revisa el material publicado sobre las necesidades relacionadas con la fertilidad de las personas que viven con VIH y la forma en que los puntos de entrada representados por los servicios relacionados con la planificación familiar, las infecciones de transmisión sexual y el VIH pueden garantizarles acceso a los servicios de anticoncepción, aborto y fertilidad. La mayoría de los métodos anticonceptivos son seguros y eficaces para las mujeres seropositivas. Las parejas que viven con VIH deben tener acceso a la gama de opciones anticonceptivas, así como a más información sobre la anticoncepción de emergencia y acceso a ésta. Se debe tener en cuenta una posible interacción de medicamentos entre la anticoncepción hormonal y el tratamiento de la tuberculosis y determinados fármacos antirretrovirales. Las parejas que viven con VIH y desean utilizar un anticonceptivo permanente deben tener acceso a la esterilización femenina y la vasectomía de manera informada, libre de coerción. Continúa siendo un reto determinar la mejor forma de promover los condones y la doble protección, así como lograr que sean aceptados en relaciones de largo plazo. El aborto quirúrgico y el aborto con medicamentos son seguros para las mujeres que viven con VIH. A fin de disminuir el riesgo de transmisión vertical del VIH y en casos de infertilidad, las personas con VIH deben tener acceso al lavado de espermatozoides y a otros métodos asistidos de concepción, si estos están disponibles. Los procedimientos sencillos y costo-eficaces deben ser parte de la consejería brindada a las personas que viven con VIH y piensan tener hijos. Es una prioridad apoyar los derechos reproductivos de las personas con VIH. Aún se deben realizar más investigaciones operativas sobre las mejores prácticas.
HIV positive women and men should be empowered to take informed choices relating to their reproductive lives, free of coercion. Their specific health condition and their socio-economic situation may render them vulnerable in this regard, however, which makes support for their reproductive rights a priority.Citation1Citation2 This is the framework within which the sexual and reproductive health of people living with HIV will be dealt in this paper.
There has been encouraging progress in providing antiretroviral treatment for people living with HIV and AIDS. However, the continuum of care that would integrate primary and secondary prevention is still far from being implemented everywhere, and access to HIV treatment is still limited. In addition, people living with HIV have diverse reproductive health needs, and unmet need for family planning services has often been greatest in countries with high HIV prevalence.Citation3 These needs might be better met if reproductive health services were provided jointly with HIV-related services. To date, however, in most settings HIV and family planning services have been offered separately.Citation4Citation5 From a policy and programmatic point of view, this paper reviews the literature on the fertility-related needs of women and men living with HIV and how the entry points represented by family planning, sexually transmitted infection (STI) and HIV-related services can ensure access to contraception, abortion and fertility services for women and men living with HIV. As many people living with HIV are still unaware of their status,Citation6Citation7 it is important to look at how reproductive health services can be provided both inside and outside HIV-related services.
Fertility-related needs of women and men living with HIV
As more than 80% of all women living with HIV and their partners are in their reproductive years,Citation8 many will continue to want children after learning their positive status, whether to start a family or to have more children. Others may wish to regulate their fertility, so that they can decide whether to try for a pregnancy and when.Citation9 Fertility-related needs of women and men living with HIV and of discordant couples may differ substantially from those who are HIV negative.Citation9,10 HIV infection may affect sexuality because of fear of infecting the sexual partner(s), feelings of guilt and shame aggravated by stigma related to HIV, or emotional or psychological distress, reducing desire for or interest in sexual relations. With the increasing availability of antiretroviral treatment and improvement in health status, there may be a renewed interest in sexual relations and the desire to have children for women and men living with HIV.Citation11
When it comes to family planning choices, when only one partner is HIV positive, the potential risk of transmitting HIV to the uninfected partner as well as the possibility of infection with other STIs should be taken into account. When both partners are living with HIV, possible re-infection with HIV has to be considered,Citation12 although there is still uncertainty regarding the risk and consequences of re-infection.Citation13Citation14 These issues may be perceived differently depending on factors such as living in a resource-poor country with limited access to both antiretroviral therapy and STI diagnosis and treatment and the level of condom use.Citation15
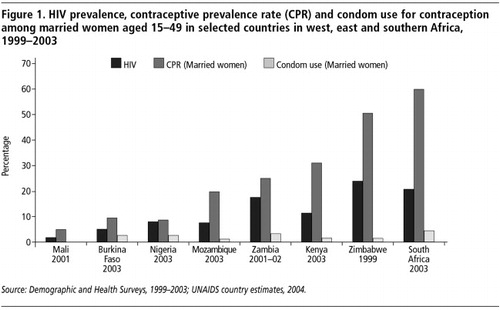
Regarding demand for contraception, some studies have pointed out that in the absence of HIV-related symptoms, the impact of having HIV on people's decisions regarding childbearing and contraceptive use is generally weak.Citation16 A study evaluating prevention of mother-to-child transmission (PMTCT) sites in Kenya and Zambia has shown that HIV positive women had similar contraceptive use rates to HIV-negative women, while in Rwanda the demand for contraception was higher among HIV positive women.Citation17Citation18 A much higher percentage of HIV positive women were using contraception in the Dominican Republic and Thailand than in African sites.Citation17 Overall accessibility of contraceptives and prevalence of contraceptive and condom use are likely to shape patterns of use among women living with HIV. This has implications for national programmes. In countries with high HIV prevalence and relatively high contraceptive prevalence rates, such as Zimbabwe or South Africa, higher contraceptive use among women living with HIV is also more likely though greater condom promotion and use will be needed. In countries such as Mali, with very low contraceptive prevalence rates, overall strengthening of family planning and condom promotion will be necessary ().
Contraceptive options and dual protection
In general, the same contraceptive options are available to couples irrespective of their HIV status. According to WHO's Medical Eligibility Criteria for Contraceptive Use, most contraceptive methods are considered to be safe and effective for HIV positive women, both with asymptomatic HIV and AIDS.Citation19 Although women living with HIV make up 59% of all adults living with HIV in sub-Saharan Africa,Citation7 there is still limited evidence of extent or type of contraceptive used by them. For women who do not feel able to negotiate safer sex, contraceptive methods they can initiate may be preferred.
| • | Hormonal contraception Recent WHO publicationsCitation19Citation20 indicate that there are no restrictions on the use by HIV positive women of hormonal contraception, whether pills, injectables, implants, patches or rings. Women on antiretroviral treatment can use them as well. However, the drug rifampicine, which is used for tuberculosis treatment, may decrease the effectiveness of oral contraceptives,Citation19Citation20 and the limited data available suggest that several antiretroviral drugs may either increase or decrease the bioavailability of steroid hormones in hormonal contraceptives. Therefore, the consistent use of condoms is recommended, not only for preventing HIV transmission, but also for preventing unintended pregnancies. Low-dose oestrogen (≤35 μg) is not recommended for women receiving rifampicine.Citation20 For discordant couples, limited evidence shows no association between combined oral contraceptive use and the risk of female-to-male HIV transmission.Citation20 With regards to the risk of HIV male-to-female transmission, some studies indicate a tendency towards an increased risk among high risk populations of women, such as sex workers.Citation21 Other studies among those using family planning services found no overall increase in risk of HIV acquisition related to the use of hormonal contraception.Citation22Citation23 In one study, among women who were seronegative for herpes simplex virus 2 (HSV-2) at enrolment, both combined oral contraceptives and depot-medroxyprogesterone acetate (depo-provera or DMPA) users had an increased risk of acquiring HIV compared to the non-hormonal group.Citation23 These results, for which solid biological explanations are difficult to find, need to be further explored.Citation24 Data on hormonal contraceptives and progression of HIV disease, while much needed, are still limited. Regarding transmission of other STIs, WHO recommends no restrictions on the use of combined oral contraceptives, progestogen-only pills, combined injectables or DMPA injections among women at high risk of STIs. However, the guidelines emphasise that none of these methods provide protection against STIs. | ||||
| • | Intrauterine device (IUD) IUDs can be used in case of HIV infection, except for women with AIDS and those not on antiretroviral therapy.Citation19Citation20 Limited evidence shows that IUD use by HIV-infected women has not been associated with increased risk of infection-related complications nor with HIV cervical shedding.Citation20 The fact that copper-bearing IUDs may increase menstrual bleeding, and subsequently the risk of anaemia, has to be taken into account in case of HIV positive women. Some authors have raised caution in advising IUD use for women at risk of STIs and pelvic inflammatory disease (PID), such as sex workers or other women in a context of high STI prevalence.Citation25 | ||||
| • | Female and male sterilisation Female sterilisation is often the most commonly used family planning method in developing countries, whereas in developed countries reversible methods are more popular.Citation26 Some studies have shown that HIV positive status influences fertility intentions,Citation27 especially the desire to stop childbearing among those who have completed their families, who therefore may favour the choice of a permanent method.Citation28 Male sterilisation (vasectomy) is also an option but its use among HIV positive men has not been documented. | ||||
| • | Emergency contraception Emergency contraception can help to prevent unintended pregnancies. Immediate accessFootnote* is crucial for method effectiveness. For women living with HIV who suffer from sexual violence, access to emergency contraception may be vital.Citation29 Concerns have been raised that some women could use emergency contraception in place of regular contraception. However, while access to information improves knowledge of this method, it does not increase its use.Citation30 In general, women living with HIV and discordant couples still seem to have far too little knowledge of emergency contraception. For example, in South Africa, where contraceptive prevalence is quite high compared to many other African countries, qualitative studies conducted among HIV and PMTCT clinic attendees showed that women and men living with HIV had little knowledge of emergency contraception or how to access it.Citation31Citation32 As with other non-barrier contraception, emergency contraception does not protect against STI or HIV transmission and information on risk reduction needs to be routinely given with it. | ||||
| • | Barrier methods Current data suggest that both male and female condoms are highly effective in protecting against pregnancy (failure rates for typical use are 15% versus 21% and for perfect use 2% versus 5%, respectively).Citation33 A recent study comparing the female and the male condom for their effectiveness in preventing pregnancy showed that the two methods are substantially the same.Citation34 Male condoms, used consistently and correctly, are the most effective means to prevent sexual transmission of HIV.Citation35 Four meta-analyses of condom effectiveness put the range at 69–94%.Citation36 Male condoms also protect against other STIs although the level of protection has not been quantified for specific STIs. Randomised controlled trials provide evidence that female condoms confer as much protection from STIs as male condoms, but there is lack of data regarding protection against HIV.Citation37–40 Recent data from people accessing services for antiretroviral treatment and PMTCT in Ghana, Ethiopia, Kenya, Rwanda and South Africa show that male condoms are the contraceptive method most frequently used by people living with HIV.Citation11,17,18,31,41–42 This differs somewhat from data on contraceptive method mix in general populations. Interventions to promote condom use in sub-Saharan Africa and Asia have generally led to increased condom use, mostly in commercial and casual sex, while levels of condom use are lower as the degree of intimacy and stability of the relationship are greater. However, condoms have rarely been promoted to stable couples either. Using condoms demands communication and negotiation. Recent studies provide a more encouraging picture in terms of women's ability to influence men's sense of sexual risk and condom use. One study has shown that married women play an important role in condom use, which depended on the woman's subjective sense of HIV risk (but not the man's).Citation43 Some authors have concluded that men's resistance to condom use can be overcome more easily than has been presumed.Citation44 This is confirmed by a recent qualitative study in Uganda among married couples who used condoms consistently for gender-specific reasons,Citation45 implying that differentiated strategies targeting men and women when promoting dual protection. However, an encouraging environment and good condom availability are crucial to increasing condom use. To date, few studies have looked at men's actual responses to female condom use.Citation45–47 Qualitative data have shown that women living with HIV in particular can feel more in control when using the female condom compared to the male condom or unprotected sex.Citation48 Women view the female condom as a means of enhancing their safer sex bargaining power within the relationship.Citation49Citation50 Efforts to target men and to empower women need to go hand in hand if persistent obstacles to condom use are to be overcome. | ||||
| • | Dual protection Protection against both unwanted pregnancy and STIs is referred to as “dual protection”.Citation51 Condoms are the mainstay of dual protection, alone or in combination with another method(s). The avoidance of penetrative sex is another means of achieving dual protection. When condoms are used in combination with another method, it can be with a non-barrier contraceptive method, male or female sterilisation, or a second barrier method, with the back-up of emergency contraception and/or induced abortion. Condoms with the back-up of emergency contraception is increasingly being used by young people.Citation52 Using condoms as a stand-alone method for dual protection may be compromised because sexually active people often are unwilling to use condoms all the time, for a variety of reasons, which reduces their protective value. Men's general dislike of condoms and women's need to rely on their male partners are often involved. Thus, much of the effectiveness of dual protection against unwanted pregnancy will be contingent on another contraceptive method being used. Empirical studies have shown, however, that the more effective the other method is for pregnancy prevention, the less likely women and their partners are to combine it with condoms.Citation53 The challenge also remains how to promote condom use, especially in stable, long-term relationships. This is particularly relevant for sero-discordant couples, who are in need of long-term adherence to safer sex. Regarding dual method use for pregnancy and STI/HIV prevention, studies have reported diverse rates ranging from 3–42%,Citation54 but few data are available regarding people living with HIV. Data suggest that dual use is more likely to occur if partners are concerned about unfavourable consequences of sexual activity (i.e. unwanted pregnancy and/or HIV/STI infection). General health behaviour or personality-related factors play a comparatively minor role.Citation55 In addition, dual method use has been correlated with having received HIV education or condom use instructions,Citation56 an elevated STI risk,Citation57Citation58 being in short-term or less committed relationships and making shared decisions about contraceptives.Citation53 Many hopes have been placed on female-controlled methods in the context of dual protection, such as the female condom. Other female-controlled methods are greatly needed for HIV prevention. However, as long as more than one method is needed to achieve dual protection, there will be extra difficulties for users, service providers and policymakers.Citation59 | ||||
| • | Microbicides: under development Microbicides include a range of products currently being developed in the form of gels, films, vaginal rings and sponges which, if found to be safe and effective, will help prevent the sexual transmission of HIV and other STIs. While many potential microbicides are currently being assessed,Citation60 the most optimistic prediction is that it will take at least five years before a safe microbicide becomes available.Citation61 | ||||
| • | Spermicides: not recommended Spermicides were developed long before HIV existed. At the time the idea of microbicides to kill HIV in semen was conceived, there were hopes that spermicides (which were shown to kill HIV in vitro), might be usable or adapted. Unfortunately, randomised controlled studies found evidence that nonoxynol-9 spermicide did not offer protection against STIs or HIV, and with frequent sex may even increase the risk of infection because it affects the vaginal lining in such a way that any HIV that was not killed could enter the system through vaginal tissue.Citation62 Women living with HIV are now advised not to use nonoxynol-9 or other existing spermicides, whether alone or in combination with condoms or other barrier methods, for this reason.Citation19 | ||||
Legal and policy implications
Human rights are the foundation of sexual and reproductive rights. Non-discrimination and equality are of particular importance when dealing with women and men living with HIV. Access to family planning services and the range of contraceptive options must be ensured for women and men living with HIV. Particularly in countries with a low contraceptive prevalence rate this is currently not the case; a study on reproductive rights for women affected by HIV carried out in Argentina, Mexico, Poland, Kenya, Lesotho, South Africa and Swaziland showed that contraceptive options tend to be limited. Health care providers' preferences determined how much and what kind of information women received about contraceptives.Citation63Citation64 In addition, the quality of family planning services is a crucial element for women and men living with HIV. Counselling has to be well conducted, ensure confidentiality and provide age-appropriate and accurate information.Citation65
While sterilisation may be a good option for HIV positive women and men, depending on age as well as personal and social circumstances, the danger of being pressured or coerced into being sterilised must not be underestimated; informed choice must be assured. In some countries, post-partum sterilisation is prohibited by law, except in cases where either future childbearing or another operation would constitute a high risk. In that context, stark differences in medical practice may greatly affect the extent of post-partum sterilisation, as shown in a study in two cities in Brazil, despite the same legal environment.Citation28 Adequate law and policy to guide decisions and implementation of programmes and services with respect to sterilisation are therefore important in order to avoid practices that violate rights.
There are still barriers to access to emergency contraception and over-the-counter sale without prescription exists only in about 40 countries, including Jamaica, Argentina, Israel, Australia, New Zealand, China, South Africa and other parts of Africa and Europe, and three of the provinces of Canada.Citation66 In some cases, there is even active opposition to making it more widely available (for instance, in Argentina and Poland), while in other places bureaucratic and financial factors impede increased availability.Citation63 Numerous studies have demonstrated that providers lack knowledge and have misconceptions about emergency contraception. Even providers who know about the method often do not offer it to women who would benefit from it.Citation67
Current supply of both male and female condoms is highly inadequate.Citation68 In particular, the supply of female condoms, though they are more than ten years on the market and despite the clear need for women-initiated methods, is significantly below levels that would have an impact on the HIV epidemic.Citation69 Large-scale production, distribution and promotion programmes, including cost reduction, are greatly needed.
With respect to dual protection, many international organisations in the field of sexual and reproductive health have issued policy statements supporting its use.Citation51,70,71 From a public health perspective the practice of dual protection is essential to the attainment of sexual and reproductive health. However, policies that have focused on condom use have largely ignored contraceptive issues and vice versa. Most policies have been targeting men by promoting condom use with casual partners believed to be at higher HIV/STI risk, and not with regular partners. How to make dual protection socially and culturally acceptable in long term-relationships has been treated as an untouchable agenda to date.Citation59 Because condoms are not considered the most effective means of fertility control, the family planning field has been reluctant to recommend condoms alone for dual protection. A mind-shift among family planning managers and service providers is necessary in order to give more room to the promotion and use of condoms. Access to emergency contraception and abortion when legal are also crucial when policies fail to promote and provide contraception and as a back-up in case of contraceptive failure. If dual protection is promoted, all means of increasing safer sex must be taken into account and included in public health campaigns.
Service delivery implications
Regarding IUDs, risk assessment for STIs should be performed before advising IUD use for HIV-positive women or women at risk for STIs and pelvic inflammatory disease. Testing for cervical infections before inserting an IUD for an HIV-positive woman has been recommended.Citation25 However, in low-resource settings this may not be feasible. In the absence of screening tests for cervical infections, presumptive treatment before insertion could be a pragmatic approach, bearing in mind that a copper IUD is effective for up to ten years. Further research is needed regarding IUD use among women living with HIV.
Sterilisation is still rarely used in sub-Saharan Africa. This is not only a culturally specific choice but also due to lack of access to good quality, affordable services.Citation72 In sub-Saharan Africa and other places with low contraceptive prevalence, access to sterilisation as well as reversible contraception should be improved to respond to unmet need among HIV-positive women and men and others of reproductive age.
Emergency contraception is still not well known and has not been sufficiently promoted in most countries. An assessment carried out in six countries among women living with HIV showed that they had limited knowledge about this method.Citation63 Many providers and women, particularly young women, often lack information about how it works, how to use it and where to get it. Information on emergency contraception in family planning training sessions should be enhanced and social marketing of emergency contraception should be encouraged.
All women and couples living with HIV or at risk of HIV infection should know about and have access to the means of dual protection. Family planning counselling protocols should include an individual/couple risk assessment to inform choice of method in relation to effectiveness for both pregnancy prevention and prevention of HIV/STI. HIV treatment centres should also include or refer for contraceptive counselling on a routine basis. Health care providers are in a key position for conveying messages about dual protection. Service providers' own biases towards dual protection and condom use alone have been identified as an important barrier to promoting dual protection effectively.Citation52Citation54 Lessons learned from two studies in Zimbabwe were that many of the mechanical obstacles to using female condoms can be overcome by sympathetic and knowledgeable support from health workers.Citation73 Negotiation and communication skills with partners are also crucial for effective dual protection and gender-specific strategies need to be adopted to promote these.Citation74
Providing dual protection on a routine basis may be more costly when two methods are provided, and access to a variety of methods will be needed. This may be an issue everywhere, but especially in developing countries.
Protection of fertility may be another issue of consideration for many women and couples. Untreated STIs may lead to secondary infertility, and condoms help to prevent secondary infertility, a concept referred to as “triple prevention” and this may be a promising way to promote condoms, particularly in cultures where discussing fertility is socially more acceptable than HIV/STI prevention.Citation75
More research is needed regarding access to and use of contraceptive methods among HIV positive women and men, in order for services to be better able to tailor service delivery to them.Citation76
Termination of pregnancy
Induced abortion for women living with HIV has been overlooked in research. WHO estimates that about 49 million abortions take place every year (out of about 220 millions estimated pregnancies), of which an estimated 19 million are unsafe. Ninety-five per cent of unsafe abortions occur in developing countries, an estimated 4.2 million in Africa alone.Citation77 The decision to have an abortion is a highly complex issue for many women living with HIV. Too many women still learn late in pregnancy about their HIV status, implying that they not only have to cope with the HIV diagnosis but also leaving no time to consider whether to continue or terminate the pregnancy. Sometimes studies do not even distinguish between induced and spontaneous abortion in their analysis of pregnancy outcomes.Citation78 Data are incomplete, not least because abortion is still legally restricted and stigmatised in so many countries.
An HIV diagnosis can have a significant impact on a woman's decision whether to carry a pregnancy to term.Citation79 Several studies have tried to assess the rate of induced abortion among pregnant women living with HIV in industrialised countries: a French cohort study among HIV positive women reported rates of pregnancy termination of 63% between 1985 and 1997.Citation80 The availability of antiretroviral drugs may have altered this picture. A European study revealed that the number of induced abortions increased from 42% to 53% in women after HIV diagnosis; however, since 1995 the proportion of births increased significantly, whereas that of induced abortions decreased compared with earlier years.Citation81 A more recent European multi-centre study found that 22% of HIV positive pregnant women had terminated a pregnancy since their HIV diagnosis, and 29% of them reported more than one termination.Citation82 The illegality of abortion does not stop women seeking abortion even in unsafe conditions. In a study carried out in Côte d'Ivoire, a third of pregnant HIV positive women terminated a pregnancy in spite of legal restrictions.Citation83
More research among HIV positive women in developing countries is needed on the complications of unsafe abortion and whether increased access to antiretrovirals is altering decisions about pregnancy termination.
Legal and policy implications
Most policy guidance documents still omit explicit statements about abortion, due to powerful opposition to abortion.Citation78 The World Health Organization as well as advocacy organisations have affirmed the right of women living with HIV to make an informed choice whether to continue or terminate a pregnancy and to have access to safe abortion where it is not against the law and to post-abortion care for complications of unsafe abortion where it is.Citation84Citation85 The Barcelona Bill of Rights, a tool for advocacy, action and monitoring progress regarding HIV positive women's rights, which was developed with strong input from women living with HIV, includes the right to safe pregnancy and legal abortion.Citation86 Preventing HIV infection yet doing nothing to prevent a woman from dying from unsafe abortion can be questioned both ethically and from a human rights point of view.
Another area of concern, however, as has happened with sterilisation, are reports of pressure or coercion to have an abortion among women living with HIV, for instance among sex workers.Citation78Citation87 This too is a violation of their rights. Service providers must not exert any pressure on women living with HIV with respect to decision-making about pregnancy termination.
Service delivery implications
Both surgical and medical methods of abortion are safe if provided according to international standards. For pregnancies up to 12 weeks gestation, vacuum aspiration should be the preferred method over dilatation and curettage (D&C).Citation19 No studies to date have investigated the complication rates of induced abortion or the specific effects, if any, of unsafe abortion on women living with HIV.Citation78 However, women with HIV may experience more complications than their HIV negative peers, due to the risk of infection, sepsis and haemorrhage. HIV positive women are also at higher risk from anaemia, especially with malaria and with certain antiretrovirals, and may be less able to resist infections.Citation88 HIV positive women may also be at higher risk of pelvic or vaginal infections from retained products of conception, which can occur with medical as well as surgical abortion. The small proportion of women who develop heavy bleeding with either method need to be treated promptly to avoid serious consequences.Citation76Citation89
Research is needed on interactions between medical abortion drugs and antiretroviral therapies, as evidence is scarce. Improvements in provider–patient relations should contribute to a better understanding of and response to factors that can affect health care needs of women living with HIV,Citation90 as well as to adequate post-abortion family planning counselling.
Infertility and assisted conception
Infertility among women and men living with HIV
Infertility affects 8–12% of the world's population,Citation91 with male and female factors accounting for 40% each, and the remaining 20% either shared or unexplained factors.Citation92 Secondary infertility is often linked to a history of certain STIs and iatrogenic infection related to poorly performed medical procedures, including unsafe abortion and delivery practices; these are all preventable conditions. Addressing the global epidemic of STIs is particularly important because of its relationship to HIV.
Studies have reported that the fertility of HIV positive women is lower than that of HIV-uninfected women in all but the youngest age group.Citation93 Determinants of lower fertility may be biological, demographic or behavioural. They include co-infection with other STIs, in particular syphilis, which puts women at higher risk of fetal loss and stillbirth.Citation94Citation95 Syphilis may cause secondary infertility or explain existing sub-fertility,Citation96 amenorrhoea and anovulation. Longer birth intervalCitation97, widowhood and divorce not followed by remarriage are other factors that may contribute to decreased fertility.Citation98 In addition, reduced sexual activity will reduce the opportunity to get pregnant. Decreasing CD4 cell count was found to decrease the incidence of pregnancy and live births in 473 women with HIV in Côte d'Ivoire followed in a seven-year study.Citation99 Finally, there is evidence that men with more advanced HIV disease have abnormal semenCitation19Citation93 and a decrease in semen volume and progressive motility has been seen in men receiving antiretroviral therapy.Citation100
Assisted conception
Giving birth and having children play a significant role for the social and the personal identity of women and men in most if not all cultures. As access to antiretroviral treatment increases, and mother-to-child-transmission rates decrease, having children can become a realistic option for many more HIV positive women and men. Because people on antiretroviral treatment recover their health, their sexual activity may also increase. Assisted reproduction techniques for couples living with HIV are often successfulCitation101,102 and can help in preventing HIV transmission in discordant couples.
Legal and policy implications
Benefits of the use of assisted reproductive technology by women and men living with HIV are two-fold: avoidance of infection of an uninfected partner, and welfare and health of the intended child. Although this was not the case in the first decade of the epidemic, most ethical committees now recommend that HIV discordant couples should have access to assisted reproductive technology,Citation103 as in most cases the decision not to treat would cause harm by increasing the risk of HIV transmission.Citation104 To date, these recommendations refer to serodiscordant couples only. The rights of HIV positive concordant couples still need to be asserted and attained.
Service delivery implications
For treatment of infertility in low-resource settings, simple investigations can be undertaken such as STI diagnosis, checking hormonal changes and pinpointing ovulation by the temperature method during the cycle. Sperm motility tests are also simple. In case of more complex infertility problems and/or in order to prevent HIV transmission within discordant couples and re-infection in concordant couples, the following techniques have been recommended:
| • | When only the woman has HIV, insemination with the partner's semen eliminates the risk of infecting him. Insemination can be carried out at home after collecting the sperm and then inserted into the vagina or by a health care provider into the cervix to conceive. In pregnancy, antiretroviral treatment needs to be initiated, for the woman depending on her individual condition, and for PMTCT.Citation105 | ||||
| • | When only the male partner has HIV, there is no risk-free way to ensure safe conception. Ways to reduce the risk of transmission include lowering the seminal plasma viral load to undetectable levels with antiretroviral treatment, timing conception at the fertile time of the menstrual cycle to limit unprotected exposure, and post-exposure prophylaxis for the woman following unprotected intercourse.Citation19 Insemination by donor sperm is also possible. Various assisted conception techniques have been used to reduce or eliminate infectious elements present in semen so that isolated spermatozoa can safely be used to start a pregnancy. Several European centres and a few US groups offer sperm washing to HIV seropositive men and their HIV negative partners, followed either by intrauterine insemination or intracytoplasmic injection of sperm (ICSI) into oocytes with in vitro fertilisation. From 1987 to 2005, more than 3,600 published attempts had been reported. A more recent report of 741 discordant couples in Italy had a 70% pregnancy rate and no infected infants. Although the data remain observational, sperm washing techniques appear to be relatively safe and effective, offering HIV serodiscordant couples an opportunity to have children where available.Citation106,107 | ||||
| • | HIV positive concordant couples intending to become pregnant should apply the method of timing conception at the fertile time of the menstrual cycle to limit exposure.Citation19 Adequate treatment for prevention of vertical transmission has to be undertaken. Sperm washing should reduce the possibility of transmission of virus mutations to the partner through unprotected sexual intercourse or donor semen can be used. | ||||
| • | Adoption, if socially and culturally acceptable. | ||||
Because of the cost and resource implications, the more sophisticated methods of assisted conception have only been accessible in industrialised countries so far,Citation78 and experience in resource-constrained settings remains very limited. Thus, there are huge gaps between choices for couples in developing and developed countries. However, with increasing access to treatment options, people living with HIV should be informed about existing options. The existence of simple procedures, as described above, should be part of counselling women and men living with HIV who intend to have children. It has been recommended that couples who present with a request for assisted conception should undergo a baseline evaluation and receive pre-conception counselling. This can help the woman to modify or initiate antiretroviral treatment to reduce both embryo-fetal toxicity and risk of vertical transmission.Citation108 Pre-conception counselling should also include a fertility assessment of the male partner (sperm analysis) prior to deciding which procedures to use.Citation109
Fertility regulation services as an entry point for women and men living with HIV
Available data show that access to family planning services for women and men living with HIV currently does not match the existing need in many settings worldwide. Usually HIV/AIDS services and fertility regulation services have been offered separately, with little or no integration.Citation5,110
In family planning services, training in giving information and services tailored to the specific needs of HIV positive women and men regarding contraception, fertility and sexuality would help health care providers to feel confident about providing services. However, it is not always easy for people to disclose their HIV status outside HIV care settings. So far, there is still limited information on how well the contraceptive and other sexual and reproductive health needs of women and men living with HIV are addressed in regular family planning services.
Dual protection messages should be provided to everyone seeking family planning and condoms. A review of experiences on integration of STI/HIV prevention and dual protection messages in family planning and maternal and child health clinics carried out in the late 1990s showed mixed results.Citation111 Providers' attitude and skills had improved and user satisfaction had increased. However, although STI prevention messages were often included in family planning services, risk assessment was seldom made and any impact on condom use, dual protection and changing risk behaviour was not clear. As mentioned earlier, absence of promotion of dual protection is due to the overwhelming emphasis still placed on non-barrier methods for pregnancy prevention by family planning services. Data on condom use as a (primary) contraceptive method among married women in general confirms this and shows extremely low absolute percentages ranging from less than 1% to 5% in most sub-Saharan African countries (). A major concern is that in many countries with a very high HIV prevalence, such as Zimbabwe or South Africa, condom use as a proportion of all family planning methods has not changed much in the last decade. For example, in Zimbabwe, with an HIV prevalence of 25% and modern contraceptive prevalence of 50% among married women in 1999, condom use was only 1.8%. However, as a recent study has shown, the trends in contraceptive uptake and condom use among single and married young women show distinct patterns in sub-Saharan Africa. A large median increase of 1.4 percentage points per year in condom use by single young women for pregnancy prevention was found in 18 countries from Demographic and Health Survey data from 1993 to 2001.Citation112 Condom promotion in Africa can therefore be considered a success for single women. Its promotion for pregnancy prevention offers even greater potential than for STI/HIV prevention, as pregnancy prevention is the main or partial motive of most single women who use condoms. The needs of the married and cohabiting population have been neglected by researchers and programme staff alike, despite the fact that more than half of HIV infections in the severe epidemics of Southern and East Africa are occurring in this group. And barriers to condom adoption by married couples may not be as severe as is often assumed.Citation112
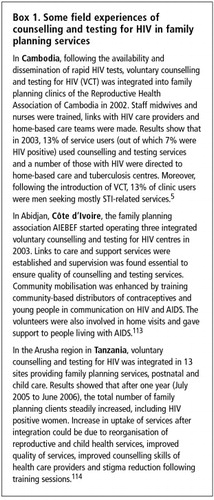
Counselling and testing for HIV in family planning services
Only a small proportion of women and men globally are aware of their HIV status, for instance one in four in developed countries such as Canada and one in three in less developed countries such as Brazil. Potentially, individuals who are unaware of their HIV-infected status may account for up to 70% of all new sexually transmitted HIV infections.Citation6Citation7 While this shows the overall importance of counselling and testing in settings where HIV treatment is available, there is still limited documented experience on its integration in family planning settings. Some field experiences are described in Box 1.
These experiences show that integration of counselling and testing for HIV into family planning services can increase access to family planning provision tailored to the needs of women and men living with HIV and possibly to dual protection.Citation115 In low HIV prevalence settings, family planning services should offer those at risk an HIV test, e.g. sex workers or people with a history of STI. In high prevalence settings, all family planning service users should be offered an HIV test. Unwanted pregnancy and induced abortion are signs of the occurrence of unprotected sex and providers in comprehensive or post-abortion care services could offer HIV testing at their sites or suggest that women consider being tested elsewhere.
HIV services as an entry point for family planning
Integration also works in the other direction, confronting similar issues, e.g. by adding family planning counselling to HIV clinical services.
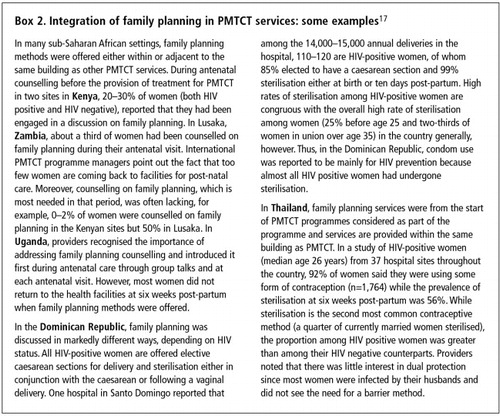
Family planning in PMTCT services
Recently, there has been a call for links between family planning and PMTCT programmes to ensure that women living with HIV have easy access to a range of contraceptive methods to prevent unintended pregnancies.Citation2,116 Family planning for HIV positive women who want to space or limit births is also an important and effective component of preventing mother-to-child transmission of HIV.Citation117,118 An analysis of family planning content in HIV/AIDS, counselling and testing and PMTCT policies in different countries has identified a number of gaps. Among others, a need for stronger links between HIV and maternal and child health and family planning departments and programmes was identified. Broader participation in policy development and review processes of people living with HIV and their networks and advocacy organisations was also called for. Operational challenges in terms of human resources, investment in training and organisation of services were also found.Citation119 PMTCT services and their increased funding represent an opportunity to initiate or strengthen the family planning component of maternity care for women living with HIV as well as for all pregnanct women.Citation33,120 A review of PMTCT services found that family planning provision is usually part of PMTCT training, but content varies between countries, and is often not considered a priority (Box 2).Citation17
Although antenatal coverage can be moderate to high in developing countries, including in sub-Saharan Africa, follow-up after delivery is always lower. The post-partum period is indeed important for women living with HIV due to advice not to breastfeed or to reduce duration of breastfeeding, which can put women at higher risk of getting pregnant again. Consequently, follow-up of women after delivery needs to be enhanced and adequate strategies such as home visits, involvement of partners and community support need to be put in place. Condom promotion needs particularly to be reinforced during pregnancy and the post-partum period, especially among HIV negative women with an HIV positive partner.Citation121
Family planning in HIV testing and counselling services
HIV testing and counselling services represent a unique opportunity to reach a lot of people with HIV who may need contraception and condoms and may not be attending family planning services. Moreover, family planning services attract women while counselling and testing services draw couples and men as well as individual women.
A recent analysis of international policy guidelines on counselling and testing for HIV showed that all policies but one explicitly addressed family planning. However, the focus in six of the nine national policies and guidelines reviewed was primarily on the provision of family planning information and referral for family planning services.Citation119 The potential for family planning service provision and coverage in testing and counselling sites exists, and the extent could vary according to site and context. However, concerns of potential negative effects on testing and counselling services from adding family planning and the question of whether it could effectively increase contraceptive uptake were raised.
To try to answer some of these questions, Family Health International conducted operations research in Kenya. First, an assessment of integration of family planning in 20 HIV voluntary counselling and testing (VCT) centresCitation122 was conducted in 2002 and showed that integration was acceptable and feasible but only a small number of centres were ready to implement it. 84% of providers counselled that condoms prevent HIV transmission but only 58% mentioned that condoms prevent pregnancy. Other contraceptive methods were mentioned by only 25% of providers. Referral for family planning was very low. Although the majority of providers came from clinical backgrounds, only 37% of VCT counsellors had participated in family planning in-service training prior to becoming counsellors. Most clients thought that addressing family planning in VCT services was a good idea. Of those using modern contraception, 42% were using condoms while only 2% were using condoms plus another contraceptive.Citation122
The baseline assessment findings resulted in a national integration strategy (adapted to each level of care), training curriculum, sensitisation workshops and training of local trainers and VCT providers. Then, the results of a subsequent study conducted in 2004 and 2005 in 14 of the same VCT sites, before and after the integration of family planning, confirmed that the intervention was feasible and acceptable.Citation123 Training improved providers' knowledge and attitudes toward family planning and the likelihood of VCT clients receiving family planning messages, especially related to condoms. There was little effect on uptake of methods other than condoms, which did increase. VCT quality was not affected. The study showed that VCT clinics represent a valid place to counsel about dual protection, and if not provide family planning methods other than condoms, at least refer people to family planning services. Referral mechanisms need to be in place to do this effectively, however, and whether integration has resulted in substantial contraceptive uptake in such sites remains unclear.Citation123
Another field experience of integrating family planning into VCT centres comes from Haiti, where a VCT centre was established in 1985 by GHESKIO, an NGO working with the Haitian Ministry of Health to provide free HIV services in Port-au-Prince. After having gradually integrated other services, such as HIV and STI care, family planning services were included in 1993. Evaluation of the project from 1985 to 2000 showed that demand for services increased 60-fold in 1999. In 1999, 19% of some 6,700 VCT clients began using contraceptives and then returned to the centre for at least three family planning visits. 70% of these new contraceptive users chose condoms alone and the remaining 30% chose another method (combined or not with condoms for dual protection).Citation5 In Uganda, family planning services were introduced into VCT services in one AIDS Information Centre in 1993 in Kampala, then in other VCT sites in the country from 1995. At the beginning, workload and time constraints were mentioned as major problems, but these were reduced with adequate training and also through the support of health volunteers who assisted counsellors.Citation5
Family planning in STI clinics and HIV treatment and care services
Implementing special STI services for populations at risk, such as sex workers, was recognised early on as an important strategy for STI/HIV control. Although a substantial proportion of sex workers may be HIV positive in many settings, they still have limited access to HIV testing and counselling and HIV treatment and care services.Citation6 In addition, comprehensive reproductive health services, including family planning for women sex workers, have been little addressed to date. Studies in Cambodia and Côte d'Ivoire showed a very low contraceptive prevalence (apart from condoms) among women sex workers and high abortion rates.Citation124,125 Access to comprehensive reproductive health care for women sex workers should be considered when dealing with the rights of women living with HIV.
In STI (or genitourinary) clinics, which are currently mainly used by men in developing countries, HIV prevention and promotion of safer sex are included in the package of information provided. However, data on need for contraception and provision of contraceptive information and methods is often scarce. A recent study in a genitourinary clinic in the UK reported that unmet contraceptive needs were low since most patients were already using a reliable method correctly.Citation126 In Bogota, Colombia, services offered at an STI clinic for men included urological procedures and in-patient surgery, general medicine, family planning (including vasectomy and condoms), infertility testing and treatment (including HIV testing), sex therapy, sperm counts and hormone, urine and blood testing. Men visiting the clinic for any one of these services could also receive counselling about reproductive health and family planning. Sex therapy consultations were particularly popular, provided by experts. These consultations introduced men to the clinic and allowed other health issues to be addressed.Citation127 Whether clinics catering primarily for men represent an opportunity to increase awareness and provide contraception services for people living with HIV remains to be determined through operations research.
To date, HIV care services in low-resource settings have been struggling to increase the number of women and men who have access to antiretroviral treatment and proper follow-up. In Haiti, antiretroviral treatment was successfully provided in the context of a comprehensive programme of HIV care, tuberculosis and STI prevention and treatment, together with women's health.Citation128 It was reported that integrated HIV prevention and care strengthened primary health care, and in particular regarding women's health, increased attendance for antenatal care. However, available quantitative evidence is limited, including in terms of the impact of integrated care on family planning.Citation129
In HIV care centres, there is an increased awareness of the importance of links between sexual and reproductive health and HIV, and on including attention to these in HIV care services. The MTCT-Plus initiative (i.e. expansion of regular PMTCT programmes to including comprehensive clinical services for HIV positive women and their families during pregnancy and post-partum) was designed to include sexual and reproductive health services in HIV care and treatment programmes.Citation130,131In South Africa, health care providers in HIV care settings identified the need for additional training, including in family planning.Citation132 Some HIV programmes refer women to family planning services but do not really ensure there is follow-up.
To date, published experiences and data on provision of contraception services within HIV care clinics or through referral to family planning services are limited. Yet this remains one of the most promising options for providing family planning for HIV positive women and men and deserves particular attention. In Mombasa, Kenya, a recent study showed that 43% of antiretroviral patients had been counselled on family planning methods and that among those currently using a contraceptive method, 37% were provided at the antiretroviral treatment clinic, 33% by a chemist/shop and only 28% at a health centre. Less than 20% of those seeing a family planning provider had disclosed their HIV status at a non-antiretroviral treatment clinic site.Citation42
While there is a need to address fertility control issues at all levels of service delivery for women and couples living with HIV, it may at the same time overburden specialised HIV services, particularly in low-resource settings. Closer links between specialised HIV care and community-based services, which may be better placed to provide family planning, could be beneficial in this respect. The move to bring HIV treatment to primary health care level may be expected to result in more adequate provision of family planning and other fertility-related services.
Conclusion
In conclusion, further research is needed on all types of hormonal contraception in women living with HIV in terms of side effects, disease progression and interaction with antiretroviral therapy (safety, efficacy and pharmacokinetics). Research studies should also address the issue of condom use among married and cohabiting women and men. Documentation of ongoing experiences and operations research on provision of contraception, abortion, sexual health, infertility and assisted conception care and services for women and men living with HIV is also greatly needed. With effective treatment just becoming available in large parts of the world, the gap in quality of care between resource-rich and resource-poor settings may grow even further as different settings will have different capacities to meet these needs. Availability of contraceptive services, better access to assisted conception services and termination of unwanted pregnancy, carried out with respect for the reproductive rights of all individuals, constitutes a great challenge for HIV care and family planning services alike if services are to meet the fertility-related needs of men, women and couples living with HIV.
Notes
* Recommended in most clinical protocols within 72 hours after unprotected sexual intercourse, and the sooner the better.
References
- United Nations, Programme of Action of the UN International Conference on Population and Development. 1994, UN. New York.
- UNFPA. Glion Call to Action on Family Planning and HIV/AIDS in Women and Children. 3–5 May 2004..
- N Walker, JM Garcia-Calleja, L Heaton. Epidemiological analysis of the quality of HIV sero-surveillance in the world: how well do we track the epidemic?. AIDS; 15(12), 2001:1545-1554.
- M Berer. Integration of sexual and reproductive health services: a health sector priority. Reproductive Health Matters; 11(21), 2003:6-15.
- Family Health International. Integration of services. Network; 23(3), 2004 At: <http://www.fhi.org/NR/Shared/enFHI. >.
- USAID, UNAIDS, WHO, UNICEF, Policy Project, Coverage of selected services for HIV/AIDS prevention, care and support in low and middle income countries in 2003. 2004, Policy Project. Washington DC.
- UNAIDS, AIDS Epidemic Update. Special report on HIV/AIDSDecember 2006, UNAIDS. Geneva.
- K Siegel, EW Schrimshaw. Reasons and justifications for considering pregnancy among women living with HIV/AIDS. Psychology of Women Quarterly; 25(2), 2001:112-123.
- HIV positive women have different needs Network; 20(4), 2001.
- Guttmacher Institute and the Joint United Nations Programme on HIV/AIDS (UNAIDS). Meeting the Sexual and Reproductive Health Needs of People Living with HIV. 2006. Series 2006 no.6..
- Degu G, Yimer G, Berhane Y, et al. Reproductive Health Needs of PLWHA on ART. Linking Reproductive Health, Family Planning, and HIV/AIDS in Africa. Conference Proceedings. Addis Ababa, 9–10 October 2006. At: <www.jhsph.edu/gatesinstitute/CR/FP-HIV-Presentations>..
- GS Gottlieb, DC Nickle, MA Jensen. Dual HIV-1 infection associated with rapid disease progression. Lancet; 363(9409), 2004:619-622.
- DM Smith, DD Richman, SJ Little. HIV superinfection. Journal of Infectious Diseases; 192(3), 2005:438-444.
- JL Marcus, MA McConnell, RM Grant. HIV superinfection vs. dual infection: what clinicians and patients should know. Medscape HIV/AIDS; 11(1), 2005 At: <www.medscape.com/viewarticle/504811. >.
- HS Mitchell, E Stephens. Contraception choice for HIV positive women. Sexually Transmitted Infections; 80(3), 2004:167-173.
- JL Chen, KA Phillips, DE Kanouse. Fertility desires and intentions of HIV positive men and women. Family Planning Perspectives; 332000:144-165.
- N Rutenberg, C Baek Review of field experiences: integration of family planning and PMTCT services. 2004, Population Council. New York. At: <http://www.popcouncil.org/pdfs/horizons/fpandpmtctrprt.pdf.2004. >. 2004.
- Ministry of Health, Rwanda, Evaluation of access to and utilization of prevention of mother-to-child transmission (PMTCT) services in RwandaJanuary 2007, TRAC, ICAP, EGPAF. Kigali.
- World Health Organization, Medical Eligibility Criteria for Contraceptive Use3rd ed.2004, WHO. Geneva.
- World Health Organization, Sexual and Reproductive health of Women with HIV. Guidelines on care, treatment and support for women living with HIV and their children in resource-constrained settings. 2006, WHO. Geneva.
- CC Wang, J Kreiss, M Reilly. Risk of HIV infection in oral contraceptive pill users: a meta-analysis. Journal of AIDS; 211999:51-58.
- World Health Organization, International Planned Parenthood Federation, Family Health International. Final Statement. Hormonal Contraception and HIV: Science and Policy. Africa Regional Meeting, Nairobi, 19–21 September 2005..
- CS Morrison, BA Richardson, F Mmiro. Hormonal contraception and the risk of HIV acquisition. AIDS; 21(1), 2007:85-95.
- M Bulterys, D Smith, A Chao. Hormonal contraception and incident HIV-1 infection: new insight and continuing challenges. AIDS; 21(1), 2007:97-99.
- R Steen, K Shapiro. Intrauterine contraceptive devices and risk of pelvic inflammatory disease: standard of care in high STI prevalence settings. Reproductive Health Matters; 12(23), 2004:136-143.
- United Nations Department of Economics and Social Affairs, Population Division, World Contraceptive Use. 2003, UN. New York. At: <www.unpopulation.org. >.
- V Paiva, EV Filipe, N Santos. The right to love: the desire for parenthood among men living with HIV. Reproductive Health Matters; 11(22), 2003:91-100.
- K Hopkins, BR Maria, KD Riva. The impact of health care providers on female sterilization among HIV-positive women in Brazil. Social Science and Medicine; 61(3), 2005:541-554.
- LW Karanja. Domestic violence and HIV infection in Uganda. Human Rights Dialogue; 2(10), 2003 At: <www.carnegiecouncil.org. >.
- A Graham, L Moore, D Sharp. Improving teenagers' knowledge of emergency contraception: cluster randomised, controlled trial of a teacher led intervention. British Medical Journal; 324(7347), 2002:1179.
- Cooper D, Myer L, Zweigenthal V, et al. Addressing reproductive intentions and reproductive health care needs among among HIV positive women and men in Cape Town, South Africa. Linking Reproductive Health, Family Planning, and HIV/AIDS in Africa. Conference Proceedings. Addis Ababa, 9-10 October 2006. At: <www.jhsph.edu/gatesinstitute/CR/FP-HIV-Presentations>..
- D Cooper, H Bracken, L Myer Reproductive intentions and choices among HIV-infected individuals in Cape Town, South Africa: lessons for reproductive policy and services provision from a qualitative study. Policy Brief. 2005, University of Cape Town, Population Council. Cape Town.
- RA Hatcher, J Trussell, F Stewart Contraceptive Technology18th revised ed.2004, Ardent Media. New York.
- T Hatzell Hoke, B Deperthes. Effectiveness of female condoms in the prevention of pregnancy and sexually transmitted diseases. PATH Global Consultation on the Female Condom. Baltimore, 26–29 September 2005. At: <www.path.org/projects/womans_condom_gcfc2005.php. >.
- S Weller, K Davis. Condom effectiveness in reducing heterosexual HIV transmission. Cochrane Database of Systematic Reviews; 12002:CD003255.
- UNAIDS, Making condoms work for HIV prevention. UNAIDS Best Practice Collection. 2004, UNAIDS. Geneva.
- WL Drew, M Blair, RC Miner. Evaluation of the virus permeability of a new condom for women. Sexually Transmitted Diseases; 17(2), 1990:110-112.
- PP French, M Latka, EL Gollub. Use-effectiveness of the female versus male condom in preventing sexually transmitted disease in women. Sexually Transmitted Diseases; 30(5), 2003:433-439.
- TR Moench, T Chipato, NS Padian. Preventing disease by protecting the cervix: the unexplored promise of internal vaginal barrier devices. AIDS; 15(13), 2001:1595-1602.
- AM Minnis, NS Padian. Effectiveness of female controlled barrier methods in preventing sexually transmitted infections and HIV: current evidence and future research directions. Sexually Transmitted Infections; 81(3), 2005:193-200.
- Adamchak S, Janowitz B, Amenyah R, et al. Family planning use and unmet need among female ART Clients in Ghana. Linking Reproductive Health, Family Planning, and HIV/AIDS in Africa. Conference Proceedings. Addis Ababa, 9–10 October 2006. At: <www.jhsph.edu/gatesinstitute/CR/FP-HIV-Presentations>..
- Sarna A, Luchters S, Shikely K, et al. Fertility preferences and family planning experiences among ART clients in Mombasa, Kenya. Linking Reproductive Health, Family Planning, and HIV/AIDS in Africa. Conference Proceedings. Addis Ababa, 9–10 October 2006. At: <www.jhsph.edu/gatesinstitute/CR/FP-HIV-Presentations>..
- Pullum T, Cleland J, Shah I. Consensus, power and trust in the use of family planning and condoms by couples in Eastern and Southern Africa. Paper presented at IUSSP International Conference, Tours 18–23 July 2005..
- P Maharaj. Obstacles to negotiating dual protection: perspectives of men and women. African Journal of Reproductive Health; 5(3), 2001:150-161.
- NE Williamson, J Liku, K McLoughlin. A qualitative study of condom use among married couples in Kampala, Uganda. Reproductive Health Matters; 14(28), 2006:89-98.
- A Penman-Aguilar, J Hall, L Artz. Presenting the female condom to men: a dyadic analysis of effect of the woman's approach. Journal of Women's Health; 35(1), 2002:37-51.
- R Pool, G Hart, G Green. Men's attitudes to condoms and female-controlled means of protection against HIV and STDs in south-western Uganda. Culture, Health & Sexuality; 2(2), 2000:197-211.
- A Welbourn. Sex, life and the female condom: some views of HIV positive women. Reproductive Health Matters; 14(28), 2006:32-40.
- S Hoffman, J Mantell, T Exner. The future of the female condom. International Family Planning Perspectives; 30(3), 2004:139-145.
- D Meekers, K Richter. Factors associated with use of the female condom in Zimbabwe. International Family Planning Perspectives; 31(1), 2005:30-37.
- World Health Organization. Joint WHO/UNAIDS/UNFPA Policy Statement. Dual protection against unwanted pregnancy and sexually transmitted infections, including HIV. 1 December 2000. At: <www.who.int/reproductive-health/publications/RHR_01_20/annex1.en.html.2000. >.
- M Berer. Dual protection: more needed than practised or understood. Reproductive Health Matters; 14(28), 2006:162-170.
- W CatesJr, MJ Steiner. Dual protection against unintended pregnancy and sexually transmitted infections: what is the best contraceptive approach?. Sexually Transmitted Diseases; 29(3), 2002:168-174.
- JE Mantell, S Hoffman, TM Exner. Family planning providers' perspectives on dual protection. Perspectives on Sexual and Reproductive Health; 35(2), 2003:71-78.
- PJ Poppen, CA Reisen. Women's use of dual methods of sexual self-protection. Journal of Women's Health; 30(2), 1999:53-66.
- L Myer, C Morroni, C Mathews. Dual method use in South Africa. International Family Planning Perspectives; 28(2), 2002:119-121.
- A Bankole, JE Darroch, S Singh. Determinants of trends in condom use in the United States, 1988–1995. Family Planning Perspectives; 31(6), 1999:264-271.
- SM Harvey, JT Henderson, MR Branch. Protecting against both pregnancy and disease: predictors of dual method use among a sample of women. Journal of Women's Health; 39(1), 2004:25-43.
- M Berer. Dual protection: making sex safer for women TKS Ravindran, M Berer, J Cottingham. Beyond Acceptability: Users' Perspectives on Contraception1997, Reproductive Health Matters for World Health Organization. London109-121.
- Rees H, et al. Phase III trial design. Paper presented at Microbicides 2004 Conference, London, 31 March 2004..
- J Balzarini, L Van Damme. Intravaginal and intrarectal microbicides to prevent HIV infection. CMAJ; 172(4), 2005:461-464.
- L Van Damme, G Ramjee, M Alary. Effectiveness of COL-1492, a nonoxynol-9 vaginal gel, on HIV-1 transmission in female sex workers: a randomised controlled trial. Lancet; 360(9338), 2002:971-977.
- Ipas. Reproductive rights for women affected by HIV/AIDS? A project to monitor Millennium Development Goals 5 and 6. 2005. At: <www.ipas.org/english/publications/international_health_policies.asp. >.
- M de Bruyn. Living with HIV: challenges in reproductive health care in South Africa. African Journal of Reproductive Health; 8(1), 2004:92-98.
- International Planned Parenthood Federation, International Community of Women Living with HIV/AIDS, Dreams and Desires. Sexual and Reproductive Health. Experiences of Women Living with HIV. 2005, IPPF, ICW. London.
- AL Clements, AM Daley. Emergency contraception: a primer for pediatric providers. Pediatric Nursing; 32(2), 2006:147-153.
- Family Health International. Revealing the “secrets” of emergency contraception. Network; 21(1), 2001 At: <www.fhi.org/en/RH/Pubs/Network/v21_1/NWvol21. >.
- A Foss, C Watts, P Vickerman Are people using condoms? Current evidence from sub-Saharan Africa and Asia and the implications for microbicides. 2003, International Family Health; HIV Tools Research Group, London School of Hygiene and Tropical Medicine. London. (Unpublished).
- PATH, UNFPA, Female Condom: A Powerful Tool for Protection. 2006, UNFPA/PATH. Seattle.
- International Planned Parenthood Federation, Statement on Dual Protection against Unwanted Pregnancy and Sexually Transmitted Infections, Including HIV. 2000 At: <http://mirror.ippf.org/medical/imap/statements/eng/2000_05a.htm. >.
- Family Health International. Many clients need dual protection. Network; 20(4), 2001 At: <www.fhi.org/NR/Shared/enFHI>.
- N Rutenberg, E Landry. A comparison of sterilization use and demand from the Demographic and Health Surveys. International Family Planning Perspectives; 19(1), 1993:4-13.
- S Ray, C Maposhere. Male and female condom use by sex workers in Zimbabwe: acceptability and obstacles TKS Ravindran, M Berer, J Cottingham. Beyond Acceptability: Users' Perspectives on Contraception1997, Reproductive Health Matters for World Health Organization. London97-108.
- L Goparaju Gender, power, and multi-partner sex: implications for dual method use in Ghana. 2003, Center for Development and Populations Activities. Washington DC. At: <www.dec.org/pdf_docs/PNACT915.pdf>.
- M Brady. Preventing sexually transmitted infections and unintended pregnancy, and safeguarding fertility: triple protection needs of young women. Reproductive Health Matters; 11(22), 2003:134-141.
- J Balkus, R Bosire, G John-Stewart. High uptake of postpartum hormonal contraception among HIV-1 seropositive women in Kenya. Sexually Transmitted Diseases; 34(1), 2007:25-29.
- World Health Organization, Unsafe Abortion: Global and regional estimates of incidence and associated mortality in 20004th ed.2004, WHO. Geneva.
- M de Bruyn HIV/AIDS and reproductive health. Sensitive and neglected issues. A review of the literature. Recommendations for action. 2005, Ipas. Chapel Hill, NC. At: <www.ipas.org>.
- JM Stephenson, A Griffioen Study Group for the Medical Research Council Collaborative Study of Women with HIV The effect of HIV diagnosis on reproductive experience. AIDS; 10(14), 1996:1683-1687.
- A Bongain, A Berrebi, E Marine-Barjoan. Changing trends in pregnancy outcome among HIV-infected women between 1985 and 1997 in two southern French university hospitals. European Journal of Obstetrics & Gynecology and Reproductive Biology; 104(2), 2002:124-128.
- BH van Benthem, I de V, MC Delmas. Pregnancies before and after HIV diagnosis in a European cohort of HIV-infected women. European Study on the Natural History of HIV Infection in Women. AIDS; 14(14), 2000:2171-2178.
- C Nöstlinger, G Bartoli, V Gordillo. Children and adolescents living with HIV positive parents: emotional and behavioural problems. Vulnerable Children and Youth Studies; 1(1), 2006:29-43.
- Desgrées de Loû A, Msellati P, Viho I, et al. Contraceptive use, protected sexual intercourse and incidence of pregnancies among African HIV-infected women. DITRAME ANRS 049 Project, Abidjan 1995–2000. International Journal of STD & AIDS 13(7):462–68..
- World Health Organization, Safe Abortion: Technical and Policy Guidance for Health Systems. 2003, WHO. Geneva.
- M Rabkin, W El-Sadr, E Abrams The Columbia Clinical Manual. 2004, Mailman School of Public Health, Columbia University. New York. At: <www.womenchildrenhiv.org/pdf/p03-pi/pi-72-00.pdf. >.
- Women at Barcelona Mujeres Adelante International Women's AIDS Causus International AIDS Society International Community of Women Living with HIV/AIDS, Barcelona Bill of Rights. 2002 At: <www.archives.healthdev/net/gender-aids/. >.
- Asia-Pacific Network of People Living with HIV/AIDS, AIDS and Discrimination in Asia. 2004 At: <www.gnpplus.net/regions/human_rights_initiative.doc. >.
- PM Lichtenberg, L Borgatta A Clinician's Guide to Medical and Surgical Abortion. 1999, Churchill Livingstone. Philadelphia.
- International Consortium for Medical Abortion. Medical Abortion: Information Package, Part 3 for Clinicians. At: <www.medicalabortionconsortium.org. >. (In preparation, April 2007).
- MR Corbett, KL Turner. Essential elements of postabortion care: origins, evolution and future directions. International Family Planning Perspectives; 29(3), 2003:106-111.
- Family Health International. Men contribute to and suffer from infertility. Network; 23(2), 2003 At: <http://FHI.org/NR/Shared/enFHI/PrinterFriendly.asp. >.
- TM Farley, EM Belsey. The prevalence of infertility. African Population Conference; International Union for the Scientific Study of Population; 1(2), 1988:1.15-2.1.30.
- B Zaba, S Gregson. Measuring the impact of HIV on fertility in Africa. AIDS; 12(Suppl.1), 1998:S41-S50.
- RH Gray, MJ Wawer, D Serwadda. Population-based study of fertility in women with HIV-1 infection in Uganda. Lancet; 351(9096), 1998:98-103.
- M Temmerman, FA Plummer, NB Mirza. Infection with HIV as a risk factor for adverse obstetrical outcome. AIDS; 4(11), 1990:1087-1093.
- A Ross, D Morgan, R Lubega. Reduced fertility associated with HIV: the contribution of pre-existing subfertility. AIDS; 13(15), 1999:2133-2141.
- JR Glynn, A Buve, M Caraël. Decreased fertility among HIV-1-infected women attending antenatal clinics in three African cities. Journal of Acquired Immune Deficiency Syndromes; 25(4), 2000:345-352.
- JP Ntozi. Widowhood, remarriage and migration during the HIV/AIDS epidemic in Uganda. Health Transition Review; 7(Suppl), 1997:125-144.
- MA Loko, S Toure, N Dakoury-Dogbo. Decreasing incidence of pregnancy by decreasing CD4 cell count in HIV-infected women in Côte d'Ivoire: a 7-year cohort study. AIDS; 19(4), 2005:443-445.
- L Bujan, M Sergerie, N Moinard. Decreased semen volume and spermatozoa motility in HIV-1 infected patients under antiretroviral treatment. Journal of Andrology2007 Jan 10 [E-pub ahead of print].
- AE Semprini, S Fiore, G Pardi. Reproductive counselling for HIV-discordant couples. Lancet; 349(9062), 1997:1401-1402.
- S Sharma, C Gilling-Smith, AE Semprini. View 1: Assisted conception in couples with HIV infection. Sexually Transmitted Infections; 79(3), 2003:185-188.
- LC Frodsham, JR Smith, C Gilling-Smith. Assessment of welfare of the child in HIV positive couples. Human Reproduction; 19(10), 2004:2420-2423.
- F Shenfield, G Pennings, J Cohen. Taskforce 8: ethics of medically assisted fertility treatment for HIV positive men and women. Human Reproduction; 19(11), 2004:2454-2456.
- International Planned Parenthood Federation. IMAP statement on the management of HIV infection within sexual and reproductive health services. IPPF Medical Bulletin; 392005:1-4 At: <http://new.ippf.org/ContentController.aspx?ID=10747. >.
- MV Sauer. Sperm washing techniques address the fertility needs of HIV-seropositive men: a clinical review. Reproductive Biomedicine Online; 10(1), 2005:135-140.
- V Savasi, E Ferrazzi, C Lanzani. Safety of sperm washing and ART outcome in 741 HIV-1-serodiscordant couples. Human Reproduction; 22(3), 2007:772-777.
- D Hawkins, M Blott, P Clayden. Guidelines for the management of HIV infection in pregnant women and the prevention of mother-to-child transmission of HIV. HIV Medicine; 6(Suppl.2), 2005:107-148 Hawkins D, Blott M, Clayden P.
- U Sonnenberg-Schwan, C Gilling-Smith, M Weigel. HIV and wish for parenthood. HIV Medicine2005 At: <www.hivmedicine.com/textbook/parent.htm>.
- I Askew, M Berer. The contribution of sexual and reproductive health services to the fight against HIV/AIDS: a review. Reproductive Health Matters; 11(22), 2003:51-73.
- KL Dehne, R Snow, KR O'Reilly. Integration of prevention and care of sexually transmitted infections with family planning services: what is the evidence for public health benefits?. Bulletin of the World Health Organization; 78(5), 2000:628-639.
- J Cleland, MM Ali, I Shah. Trends in protective behaviour among single vs. married young women in sub-Saharan Africa: the big picture. Reproductive Health Matters; 14(28), 2006:17-22.
- International Planned Parenthood Federation UNFPA, Integrating HIV voluntary counselling and testing services into reproductive health settings. IPPF, UNFPA. 2004.
- Mphuru L, Perchal P, Barone M, et al. Integration of voluntary counseling and testing for HIV into family planning and reproductive health services in Arusha Region, Tanzania. Linking Reproductive Health, Family Planning, and HIV/AIDS in Africa. Conference Proceedings. Addis Ababa, 9-10 October 2006. At: <www.jhsph.edu/gatesinstitute/CR/FP-HIV-Presentations>..
- M Myaya Integrating HIV Voluntary Counselling and Testing Services into Reproductive Health Settings: Stepwise Guidelines for Programme Planners, Managers, and Service Providers. 2004, IPPF South Asia Regional Office, UNFPA. London.
- WHO, UNFPA, UNAIDS, IPPF, Sexual and Reproductive Health and HIV/AIDS. A Framework For Priority Linkages. 2005, WHO. Geneva.
- MD Sweat. Cost-effectiveness of nevirapine to prevent mother-to-child HIV transmission in eight African countries. AIDS; 18(12), 2004:1661-1671.
- HW Reynolds, B Janowitz, R Homan. The value of contraception to prevent perinatal HIV transmission. Sexually Transmitted Diseases; 332006:350-356.
- M Strachan, A Akua Kwateng, K Hardee. An analysis of family planning contents in HIV/AIDS, VCT, and PMCT policies in 16 countries. Policy Project. Policy Working Paper Series No.9, 2004. At: <www.policyproject.com/BySeries.cfm/WPS. >.
- K Best Family planning and the prevention of mother-to-child transmission of HIV: a review of the literature. 2004, Family Health International. Chapel Hill NC.
- RH Gray, X Li, G Kigozi. Increased risk of incident HIV during pregnancy in Rakai, Uganda: a prospective study. Lancet; 366(9492), 2005:1182-1188.
- HW Reynolds, J Liku, BN Maggwa VCT & FP Study Integration Team Assessment of voluntary counselling and testing centers in Kenya. Potential demand, acceptability, readiness, and feasibility of integrating family planning into VCT. 2003, Family Health International. Chapel Hill NC.
- HW Reynolds, J Liku, A Beaston-Blaakman Integrating family planning into voluntary counseling and testing centers in Kenya. Operations research results. 2006, Family Health International. Chapel Hill NC. At: <www.fhi.org/en/RH/Pubs/booksReports/FPVCTKenya.htm. >.
- T Delvaux, F Crabbé, S Seng. The need for family planning and safe abortion services among women sex workers seeking STI care in Cambodia. Reproductive Health Matters; 1(21), 2003:88-95.
- B Vuylsteke, PD Ghys, G Mah-bi. Where do sex workers go for health care? A community based study in Abidjan, Côte d'Ivoire. Sexually Transmitted Infections; 77(5), 2001:351-352.
- F Mahar, J Sherrard. Is genitourinary medicine meeting the contraception needs of clinic attendees?. International Journal of STD and AIDS; 16(8), 2005:543-545.
- Family Health International. Men and reproductive health. Network; 181998:29-30 See also: Rogow D. Man/Hombre/Homme: Meeting Male Reproductive Health Care Needs in Latin America. Quality/Calidad/Qualité No. 2. New York: Population Council, 1990.
- SP Koenig, F Leandre, PE Farmer. Scaling-up HIV treatment programmes in resource-limited settings: the rural Haiti experience. AIDS; 18(Suppl.3), 2004:S21-S25.
- DA Walton, PE Farmer, W Lambert. Integrated HIV prevention and care strengthens primary health care: lessons from rural Haiti. Journal of Public Health Policy; 25(2), 2004:137-158.
- L Myer, C Morroni, WM El-Sadr. Reproductive decisions in HIV-infected individuals. Lancet; 366(9487), 2005:698-700.
- L Myer, M Rabkin, EJ Abrams. Focus on women: linking HIV care and treatment with reproductive health services in the MTCT-Plus Initiative. Reproductive Health Matters; 13(25), 2005:136-146.
- AL Stenson, S Charalambous, T Dwadwa. Evaluation of antiretroviral therapy (ART)-related counselling in a workplace-based ART implementation programme, South Africa. AIDS Care; 17(8), 2005:949-957.