Abstract
Sexual health is defined in terms of well-being, but is challenged by the social, cultural and economic realities faced by women and men with HIV. A sexual rights approach puts women and men with HIV in charge of their sexual health. Accurate, accessible information to make informed choices and safe, pleasurable sexual relationships possible is best delivered through peer education and health professionals trained in empathetic approaches to sensitive issues. Young people with HIV especially need appropriate sex education and support for dealing with sexuality and self-identity with HIV. Women and men with HIV need condoms, appropriate services for sexually transmitted infections, sexual dysfunction and management of cervical and anogenital cancers. Interventions based on positive prevention, that combine protection of personal health with avoiding HIV/STI transmission to partners, are recommended. HIV counselling following a positive test has increased condom use and decreased coercive sex and outside sexual contacts among discordant couples. HIV treatment and care have reduced stigma and increased uptake of HIV testing and disclosure of positive status to partners. High adherence to antiretroviral therapy and safer sexual behaviour must go hand-in-hand. Sexual health services have worked with peer educators and volunteer groups to reach those at higher risk, such as sex workers. Technological advances in diagnosis of STIs, microbicide development and screening and vaccination for human papillomavirus must be available in developing countries and for those with the highest need globally.
Résumé
La santé génésique, définie en termes de bien-être, est menacée par les réalités sociales, culturelles et économiques des femmes et des hommes séropositifs. Il faut donner aux femmes et aux hommes séropositifs la maîtrise de leur santé génésique. Les pairs et les personnels sanitaires formés à des approches empathiques sont les mieux à même de transmettre des informations exactes pour permettre des choix éclairés et des relations sexuelles sûres et agréables. Les jeunes séropositifs ont spécialement besoin d'éducation sexuelle et de soutien pour vivre leur sexualité et leur identité par rapport au VIH. Les femmes et les hommes séropositifs doivent disposer de préservatifs, de services adaptés de prise en charge des IST, des dysfonctionnements sexuels et des cancers de la sphère anale et génitale. On recommande des interventions fondées sur la prévention positive, qui protègent la santé personnelle tout en évitant la contamination des partenaires. Le conseil après un test positif au VIH a augmenté l'utilisation du préservatif, et a diminué les rapports sexuels forcés et les contacts sexuels extérieurs chez les couples sérodiscordants. Le traitement du VIH a atténué la stigmatisation, et encouragé le dépistage et la révélation de la séropositivité aux partenaires. L'observance du traitement antirétroviral doit aller de pair avec un comportement sexuel plus sûr. Les services de santé génésique ont collaboré avec les éducateurs pairs et les groupes de bénévoles pour atteindre les populations les plus exposées, comme les professionnel(le)s du sexe. Les progrès technologiques dans le diagnostic des IST, la mise au point de microbicides et le dépistage et la vaccination contre le papillomavirus doivent être disponibles dans les pays en développement et pour ceux qui en ont le plus besoin.
Resumen
La salud sexual, definida en términos de bienestar, se ve afectada por las realidades sociales, culturales y económicas que afrontan las personas con VIH. Un enfoque en los derechos sexuales pone a dichas personas en control de su salud sexual. La mejor forma de suministrar información exacta y accesible para propiciar una toma de decisiones informadas y relaciones sexuales seguras y placenteras es mediante la educación por pares y profesionales de la salud capacitados en tratar los asuntos delicados con empatía. En particular, la juventud con VIH necesita una educación sexual y apoyo adecuados para lidiar con la sexualidad y autoidentidad con el VIH. Las personas con VIH necesitan condones, servicios adecuados para las infecciones de transmisión sexual, la disfunción sexual y el manejo del cáncer cervical y anogenital. Se recomiendan intervenciones basadas en la prevención positiva, que combinen la protección de la salud personal con evitar la transmisión de ITS/VIH a las parejas. Gracias a la consejería sobre el VIH después de una prueba positiva, ha aumentado el uso de condones y disminuido el sexo forzado y los contactos sexuales exteriores entre parejas discordantes. El tratamiento y la atención del VIH han reducido el estigma y aumentado la aceptación de las pruebas de VIH y la divulgación del estado seropositivo a las parejas. La terapia antirretroviral y el comportamiento sexual más seguro deben ir de la mano. Los servicios de salud sexual han trabajado con educadores de pares y grupos voluntarios para alcanzar a aquellas personas que corren un riesgo más alto, como las trabajadoras sexuales. Los avances tecnológicos en el diagnóstico de ITS, desarrollo de microbicidas y la detección sistemática y vacunación del virus del papiloma humano deben estar a la disposición de los países en desarrollo y las personas más necesitadas mundialmente.
“ Sexual health is a state of physical, emotional, mental and social well-being in relation to sexuality; it is not merely the absence of disease, dysfunction or infirmity. Sexual health requires a positive and respectful approach to sexuality and sexual relationships, as well as the possibility of having pleasurable and safe sexual experiences, free of coercion, discrimination and violence.
Sexual rights embrace human rights that are already recognized in national laws, international human rights documents and other consensus statements. They include the right of all persons, free of coercion, discrimination and violence to the highest attainable standard of sexual health, and to access to sexual and reproductive health care services.”Citation1 Footnote*
Biology, history, politics, religion and law interact to regulate sexual expression in ways that may promote or undermine health, and in many countries these may target or affect people living with HIV in particular ways. Poverty, attitudes towards sexuality and gender power relations, and tensions between individual rights to privacy and self-determination and the rights of partners, families and communities as regards the practice of safer sex also influence sexual health.
The sexual rights of people with HIV are often not recognised or respected. Poor communication by and with health care providers on sexual issues mean that informed choices may be limited and services not offered. Certain religious leaders and faith-based organisations emphasise or promote only sexual abstinence for young and unmarried people in spite of evidence that many are having unsafe sex and may have HIV, and need information and the means to protect themselves and their partners from sexually transmitted infections (STIs) and women partners unwanted pregnancy. In many settings, people with HIV are expected not to have sexual lives, and their sexual health needs and rights may not even be considered. People living with HIV may be among the least able to access health services, yet are among those at highest risk for sexual health problems. They need information on how to look after their health in ways that put them in charge of looking after themselves and able to protect their partners and families.Citation2
Programmes to improve sexual health for women, men and young people with HIV have to take into account a person's actual sexual relationship(s) in the context of their lives and socio-economic situation, and their need for information. The concept of “positive prevention” endorses the right of HIV positive people to have a healthy sexual life, access strategies to support and protect their sexual health, prevent and treat STIs and maintain good health with antiretroviral treatment and other health care. Positive prevention is also about positive people acknowledging they have a crucial role in controlling the HIV epidemic and avoiding transmitting HIV to others, while also having rights to health and safer sex of their own.Citation3Citation4 Positive prevention requires a supportive, non-discriminatory environment for people to learn their HIV status, disclose it to partners, access non-judgemental treatment and care, and receive respect from their partners, family, community and peers.
To be able to enjoy safer sexual lives, people with HIV have requested sexual health education; help to gain skills to negotiate safe sex; long-term supportive counselling that addresses the risk of HIV/STI transmission to regular and casual partners (both in sero-discordant and concordant relationships); access to condoms and lubricants and information on how to use them; guidance on other safer sex practices; information on re-infection with HIV; and regular health check-ups to treat STIs and opportunistic infections, cervical and ano-genital cancer screening, and counselling and treatment for sexual dysfunction.Citation2
Based on the literature, this paper examines the sexual health needs of adolescents, young people, women and men living with HIV and how these can best be met through health policies, programmes and services.Citation5
Sexual health and sexuality education for HIV positive adolescents and young people
The impact of HIV therapies is particularly noteworthy among HIV-positive youth who have been infected perinatally or through blood products. Significant numbers of youth now treated in adolescent HIV clinics in the USA, for example, have “graduated” into these programmes from paediatric HIV clinics. Such longevity was unthinkable a decade ago, when most HIV positive children died before their tenth birthday. Further, people diagnosed during adolescence now survive well into their 20s, with many maturing into their 30s.Citation6
It is critical to understand the developmental stages and changes of adolescence in developing outreach and care strategies. Relevant changes among younger teens include physiological growth and maturation, intense sexual feelings, movement away from dependence on parents to peers, and understanding of cause and effect. Girls start their menstrual periods and boys' sex organs mature, and as they get older, youth increase their ability to take responsibility for their own actions but also have periods of self-consciousness and self-criticism, bouts of low self-esteem, mood swings and an increased desire for independence. Being HIV positive complicates being young and confronting sexuality for the first time.Citation6
HIV positive young people are a diverse group, differing in age, gender, sexual orientation, race and ethnicity, educational attainment, economic circumstances and cognitive abilities. They experience differing rates of mental illness, chemical dependency, social isolation and lack of economic opportunity. HIV positive youth are more likely to be female, men who have sex with men, from racial and ethnic minority populations, and from economically deprived groups than their HIV negative counterparts. High-risk sexual behavior is the dominant mode of HIV transmission among youth. HIV positive young men are much more likely to have acquired the virus through same-sex contact, including unprotected anal intercourse, and in some cultures also sexual contact with older women. HIV positive young women are more likely to have been infected through heterosexual activity, such as unprotected vaginal and anal intercourse, often with (young) men older than themselves. High-risk sexual behaviour is common among youth, primarily associated with a culturally prevalent expectation of sexual interaction among this age group.Citation6 Yet the adult and parent world often wish to deny and ignore why young people become HIV positive.
“… young people are, at times, abandoned by their parents, society and the church to learn by themselves the life skills which sexual relationships require… to wither and die through ignorance, the absence of open, honest and compassionate sharing of vital information, and our embarrassed silence and resistance to reality.” (Njongonkulu Ndungane, Archbishop of Cape Town)Citation7
Knowledge is critical for adolescents and young people to protect their health. Paucity of sexual health education and services tailored to adolescents and youth at risk, many of whom are out of school and unemployed, contributes to high rates of STIs, HIV and unintended pregnancy. Young people seek and welcome this information, as a recent cross-sectional survey of internet use among 500 school-going adolescents aged 12–18 years in Mbarara, Uganda, shows. The majority of youth in this rural area of Uganda expressed the need for such information. Some 35% (173) had used the internet at home to find information about HIV and AIDS, and 20% (102) had looked for sexual health information. If internet access were free, 66% (330) reported that they would search for information about HIV/AIDS prevention online.Citation8 Youth from homes with less education had less access to the internet and therefore to information. Yet young people did not appear to be encouraged to access this information while at school; going online at school was inversely related to looking for HIV/AIDS information via technology.
Research shows that school-based sexuality education programmes for youth:
| • | reduce stigma and discrimination as well as STIs, HIV and unintended pregnancy;Citation9 | ||||
| • | do not encourage early sexual activity in adolescents or increase the number of their sexual partners;Citation10Citation11 and | ||||
| • | can increase knowledge and reduce risk behaviour.Citation12Citation13 | ||||
The literature is replete with descriptions of prevention interventions aimed at increasing knowledge and understanding of sexuality and sex-related issues for adolescents and young people – involving schools, peer counselling, drama and the internet. All of them assume that the adolescents and young people being targeted are HIV negative, however, and there are few evaluations of interventions targeting HIV positive young people. Yet 25% of all new HIV infections globally are in adolescents and young people, especially in high prevalence settings, and children who have had HIV since infancy need information and support as they become adolescents and young adults.
An HIV positive youth at the International AIDS Conference in Toronto in August 2006 pointed out that the difference between HIV prevention for HIV negative youth and AIDS prevention for HIV positive youth is often not addressed, and there is almost no one teaching positive adolescents about sexuality with HIV (Marge Berer, Editor, RHM, Personal communication, April 2007). Adolescents need preparation emotionally and practically for taking antiretroviral drugs. As regards relationships, there are special disclosure issues – even if adolescents have never had intercourse and may not be ready for it, should they tell a new partner they are positive before or after the first kiss? Thus, there are sexual and reproductive health issues relevant to young HIV positive adolescents that need to be mapped with them and appropriate programmes developed.
Young African women with HIV recently prioritised non-judgmental, skills-based training on relationships, sexuality and sexual identity, communication and assertiveness training, negotiation skills for safer sex, and information on the safety of different sexual practices.Citation7 In spite of national commitments to support adolescent sexual health and end the HIV epidemic, these needs are still not being met in most countries of the world today.
Instead, national sexual health programmes for young people in a number of African and other countries funded under US PEPFAR money or run by faith-based organisations are promoting sexual abstinence only. A condition for receiving PEPFAR money is that the funds may not be used to physically distribute or provide condoms in school settings or for marketing efforts to promote condoms to youths, nor in any setting to promote condoms as the primary intervention for HIV prevention.Citation14
“It is not possible to promote condoms only for high risk people without stigmatising both the people and condoms, and it also jeopardises promoting condom use for contraception. Everything possible must be done to reduce negative messages about condoms. Everyone involved in HIV/AIDS needs to reflect on their own work in relation to this new climate and ensure that all prevention options are widely available, correct information is given and condoms are available for everyone who needs them.” Citation15
While many young people, both positive and negative, may welcome programmes that support not having sex, abstinence is hard to sustain as a “forever” or long-term option. In the USA, oral gonorrhoea is higher in young people who have been taught only about abstinence.Citation16 Interviews with ten HIV positive young women and men aged 17–24 years in Sweden found that “cultures of silence” surrounding sexuality were critical in making them vulnerable to HIV infection, alongside lack of adult supervision when they were children, naïve views, being in love, alcohol and drugs, a macho ideal and gender differentials as regards sex affecting both consensual and forced sex.Citation17
A rights-based approach in the case of adolescents is based on the recognition of the right of adolescents to full and accurate sexuality information and education as means to ensure that they “have the ability to acquire knowledge and skills to protect themselves and others as they begin to express their sexuality.”Citation18
A growing number of NGO-led projects for young people may serve as models for implementing a rights-based approach for national programmes to adapt and scale up. The Médécins Sans Frontières South Africa Khayelitsha Project has operated a youth-friendly service since 2004 that focuses on health education, testing and counselling, HIV care and follow-up, STI care and family planning. About 1,700 young people aged 12–25 visit monthly. Every young person needing STI treatment is strongly encouraged to learn their HIV status, and 26% of those tested so far have been HIV positive. The majority of young people first come for family planning, which gives an excellent opportunity to discuss condom use and safer sex. Follow-up for HIV positive youth with low CD4 counts has been increased to once monthly to assure continuing sex education and support. This has overwhelmed staff workloads but this problem is being addressed by encouraging more HIV support groups for young people.Citation19
Also in South Africa, the UN Development Programme has initiated three pilot projects that involve HIV positive youth, in the provinces of Limpopo, KwaZuluNatal and Eastern Cape, in partnership with national and provincial departments of health, the Department of Social Development, and UNFIP, UNICEF and UNFPA. These are pilots for a programme by and for HIV positive youth aimed at involving them in NGOs providing community and home-based care and support, promoting behavioural change by involving them in action research on sexual attitudes and behaviours, the acquisition of life skills and the relationship between HIV risk and sexual violence, and involving them in local employment situations to equip them with the skills to enable them to better manage their status, and to enhance their potential for employment.Citation20
Ongoing health maintenance, monitoring of immune function and viral load, providing education about HIV and risk reduction, providing access to treatment, identifying and addressing psychosocial needs and depression, promoting skills to live independently and to make the transition to adulthood, treating STIs, providing contraceptives and condoms, support for childcare, and reinforcing and sustaining safer sex behaviours are all important elements of youth-friendly services for young people with HIV.Citation21
Barriers to health care for HIV-infected young people include lack of financial resources, mistrust of health care professionals, difficulty negotiating the health care system, complicated treatment regimens, lack of providers with expertise in both HIV and adolescent medicine, and concerns about confidentiality and disclosure. Laws and institutional policies governing adolescents' rights to confidentiality and consent may not even exist. Fear and denial may also play a part. Research in the USA has pinpointed the following components of youth-friendly services for HIV-positive youth:
| • | Flexible hours, including weekends and evenings, to lessen conflicts with school or work. | ||||
| • | Walk-in appointments, to encourage use of services. | ||||
| • | Accessibility through convenient locations near public transport, travel vouchers and transportation assistance for rural youth. | ||||
| • | Intensive case management to assist with disclosure and partner notification, and to link youth to mental health care, substance abuse treatment, housing as needed. | ||||
| • | Active involvement of young people in all aspects of programme planning, operations and evaluation. | ||||
| • | Staffing, at least in part, by members of the target population. | ||||
| • | Culturally competent staff who are sensitive to youth culture and to racial and ethnic cultures as well as to issues of gender, sexual orientation and HIV status. | ||||
| • | Services appropriate to those being served, e.g. street outreach for homeless youth and tailored support groups for gay, lesbian, bisexual, transgender and questioning youth, substance users, and adolescent parents. | ||||
| • | Youthful and welcoming décor, materials and atmosphere. | ||||
| • | Informational materials appropriate to the languages and literacy levels of the youth served.Citation21 | ||||
HIV counselling and testing, disclosure of HIV positive status and partner notification
The majority of people with the highest incidence of new HIV infections (adolescents, sex workers, men who have sex with men, and injection drug users) are unaware of their HIV status. They need access to sympathetic HIV counselling and testing services to learn their serostatus and how to maintain their health if they are positive. Over half of new HIV infections in the USA were spread by HIV positive people who were unaware of their status. Once they knew, they reduced their high-risk practices by half.Citation22 In Kenya, Tanzania and Trinidad, after learning their HIV status, discordant couples increased condom use and decreased sexual contacts outside the relationship.Citation23–26 In Rwanda, intensive male-focused counselling and testing dramatically increased condom use and decreased coercive sex at one-year follow-up, compared to those receiving conventional counselling and testing.Citation27 In a Zambia study, condom use increased from less than 3% to more than 80% after counselling and testing, and was sustained over the 12 months of the study, although there was substantial under-reporting of unprotected sex.Citation28
Few HIV care programmes offer sexual and reproductive health services at all, but where they do, providers may not offer sufficient information for considered decision-making.Citation29 When care and treatment for HIV and STIs are combined with education in suitable settings, directly or through referral, the opportunities for reaching people with HIV are increased with greater impact on reducing further transmission. UNAIDS/WHO have demonstrated the potential for increasing
prevention, treatment and care synergies as more people get tested in order to access life-saving antiretroviral treatment, and more people on treatment are brought back to health.Citation30 In Haiti and South Africa, introduction of HIV treatment and care reduced stigma, increased uptake of counselling and testing and disclosure to partners.Citation31Citation32
Fear of the consequences of disclosure of HIV to a partner may hamper communication around sexual issues. Disclosure and attempts by positive women and men to use condoms to protect their partners are often met with anger or disbelief.Citation33 A study among French gay men emphasises the need to encourage communication and HIV disclosure in HIV-discordant gay couples. Where HIV-positive partners had not disclosed their status to their HIV negative or untested regular partners, unprotected sex was more likely. Binge-drinking also made inconsistent condom use more likely in HIV discordant partnerships.Citation34
WHO and UNAIDS have pointed to the fear of disclosing HIV positive status to health care workers in order to receive appropriate and timely care; to families and communities in order to get psychosocial and practical support; and to sexual and drug-injecting partners, to prevent onward transmission of HIV. Several years ago they called for the promotion of “beneficial disclosure” and “ethical partner counselling” as crucial steps to reducing stigma and creating a more open, accepting social environment. Criminalisation of those who have not disclosed their status and may have transmitted HIV is considered as counter-productive. Beneficial disclosure is voluntary, respectful of the autonomy and dignity of people with HIV, maintains confidentiality and emphasises benefits to both partners. This can be achieved through counselling and testing services, workplace policies and community care but only if health workers are trained, supervised and supported in their work as well. Ethical partner counselling involves confidentiality and informed consent for disclosure by the person with HIV, with strong professional efforts to persuade them to notify partners. In recognition of the serious consequences of partners not being informed and thereby putting others at risk of infection, WHO/UNAIDS advise that health care providers may counsel the partners of positive people without their consent after an ethical weighing of possible harm.Citation35 The General Medical Council in Britain similarly permits disclosure by a health professional in order to protect the partner and others from risk of death or serious harm, but not those, including relatives, who are not at risk of infection.Citation36
Non-disclosure of HIV status to sexual partners has been a fraught area for health professionals as they have witnessed partners of positive people becoming infected out of lack of knowledge. Women have acquired HIV through sexual transmission without realising their partners were also having sex with men or injection drug users, thus at higher risk of HIV.Citation37Citation38 Knowledge of partner status may not protect women who do not have the social or economic independence to withdraw from relationships, or the power to refuse unprotected sex. Problems arise where disclosure is accompanied by blame, violence, betrayal and bitterness. “Shared confidentiality”, i.e. revealing sensitive information such as HIV status to defined groups such as family or close community members in order to support the affected person, e.g. with home-based care, has assisted families to come to terms with HIV through an emphasis on mutual benefit and support. Health professionals, peer facilitators and family mediators, such as from faith-based organisations, can assist families to mitigate the impact, especially where benefits accrue with disclosure such as STI and antiretroviral treatment.Citation39Citation40
Sexual transmission of HIV, safer sex and risk reduction
For people with HIV, the importance of safer sex with an HIV negative sexual partner or one with uncertain status (an HIV serodiscordant relationship) is for self-protection from STIs and to protect the partner from becoming HIV infected. Between two people with HIV (an HIV seroconcordant relationship), the aim is to protect each other from STIs and re-infection. In an HIV discordant relationship, making sure the HIV negative partner or partners, whether regular or casual, remain negative is particularly challenging.
The risk of sexual transmission of HIV increases if the HIV positive partner has a high viral load, e.g. during seroconversion in the early stages of HIV infection and during late-stage disease. Between these stages the risk of infection is still present, but can be considerably lower.Citation41 Concurrent STIs facilitate HIV transmission through genital ulcers, inflammation of vaginal and anal tissue and under the foreskin of the penis, and concentration of HIV in STI-related discharge and secretions. Women who have unprotected vaginal sex and both men and women who have unprotected anal penetration are more vulnerable biologically than men who penetrate their partners.Citation42 Adolescent girls are at higher risk in unprotected penetrative vaginal sex because of immaturity of the genital tract. The increased vulnerability of the recipient of semen results from the larger surface area of the vagina or rectum relative to the penis and the longer period during which semen remains in contact with tissue. Rough, forced sex can cause abrasions and bleeding, enhancing transmission of HIV and hepatitis B.
The ability to practise safer sex depends on confidence, communication and trust in the partner and the relationship. These characteristics may or may not be present; indeed, sex may take place with little or no communication whatsoever and/or may be coerced. Health care workers, counsellors and educators need training and possibly sexuality education themselves in order to address sexual issues with HIV positive people professionally, in a sex-positive way and without judgment. Discussing sex is taboo in many cultures, making the delivery of education to health workers and the discussion of safer sex by them with people living with and at risk of HIV very difficult.
Safer sex promotion can only be effective if it considers people's real-world sexual desires and activities.Citation43 Case histories of how people in diverse HIV serodiscordant relationships have become infected (e.g. both among male factory workers in Zimbabwe and gay men in the USA) indicate areas for intervention such as improving perceptions of risk, addressing the link between low self-esteem, loss of control and unsafe sex, and teaching ways to show love and intimacy that incorporate condom use and other safer sex practices.Citation39Citation40 The risk discourses of HIV researchers and educators may be different from those in the narratives of HIV positive people in their own seroconversion. A case-series study of seroconversion in Australia, in which men who had seroconverted were asked to give an account of the occasion on which they believed they were infected found that the reasons they gave for their HIV infection varied depending on the context. Within regular relationships, breakdown of negotiated safety, love and intimacy, and fatalism were among the explanations given. In casual sexual encounters seroconversion was more likely to be explained in terms of pleasure, lack of control and related to particular sexual settings. The ways in which men understood their HIV infection were informed both by the risk discourse of HIV researchers and also by the discourses of love, pleasure and control.Citation44
Certain health educators, governments and faith-based organisations have been inclined to give simple “do” or “don't do” messages, including “ABC”, but the reality is more complex. Decisions based on safer sex information require some understanding of biological principles of disease transmission, while many cultures operate with different belief systems of health and disease. Behavioural factors include sex between older, more sexually experienced men and younger women (and vice versa), having more than one partner, having multiple partners (as with selling sex), and frequent partner change. Loss of self-control leading to unsafe sex may occur under the influence of alcohol or drug use. Sex workers often do not use condoms with lovers in order to differentiate them from commercial clients.Citation45Citation46 Where sex between men or with transgender people is criminalised or stigmatised, which is still the case in most developing countries, the need to hide these relationships from neighbours and family may lead to quick, unprotected sex in places like secluded cruising areas, which mitigates hugely against developing steady partnerships.Citation47 Safer sex is far more complicated to promote and practise in all these situations.
Not having sex at all is of course the safest path but of no help for those who wish to have sex or are forced to do so. Based on biological principles of disease transmission, safe(r) sex refers to sexual activities that avoid or reduce exchange of body fluids (semen, blood, vaginal fluids), avoid genital-to-genital contact and reduce risk of STI and HIV transmission, including re-infection. The most effective forms of safe(r) sex are:
| • | Non-penetrative sex (no penetration of the vagina, anus or mouth by the penis) including masturbation, mutual masturbation, kissing, sex-talking, massage and other forms of touching and stimulation. | ||||
| • | Mutual monogamy or polygamy between partners with no pre-existing infection. Protection depends on each partner being faithful, and no partner having a relationship outside the couple or circle. | ||||
| • | Use of male or female condoms alone, including for vaginal and anal sex and non-lubricated male condoms for oral sex. | ||||
There are also risk reduction approaches that are somewhat safe or safer than others rather than “absolutely safe”, and their efficacy and acceptability will vary considerably. Evidence shows that consistent and correct condom use is the most effective risk-reduction strategy. Other risk reduction strategies, with differing and in some cases uncertain degrees of efficacy include withdrawal, oral sex, male circumcision for HIV negative men, maintaining a low viral load through antiretroviral therapyCitation48Citation49 and sero-sorting (people with HIV seeking relationships with positive partners).
Withdrawal (coitus interruptus) has been used for centuries as a risk reduction method for preventing pregnancy. Since the early days of the HIV epidemic it has also been used by gay men (or the variation of temporary and partial penetration without a condom), e.g. in Australia,Citation50 for risk reduction. Withdrawal does not protect against other STIs, and its efficacy for HIV risk reduction has never been studied.
Oral sex is an exciting alternative to penetrative sex for many people. It is difficult to study HIV transmission through oral sex because most people engage in other sexual activities as well, though most STIs other than HIV (e.g. syphilis, herpes and gonorrhoea) are transmissible orally. The current consensus is that unprotected oral sex is an effective risk reduction strategy compared to unprotected anal or vaginal penetration. The UK's Public Health Laboratory Service estimates that 1–3% of HIV cases may be due to oral sex. One American study on the risks of HIV transmission from oral sex reported that of 122 gay men with HIV, 8% reported oral sex as their only risk activity. However, some of the men in this study who initially said oral sex was their only risk activity subsequently admitted having unprotected anal sex. A recent study did not find any cases of oral transmission of HIV over a ten-year period in over 100 couples where one partner was HIV positive and the other HIV negative.Citation51 Over 19,000 instances of unprotected oral sex did not lead to a single case of HIV transmission amongst a cohort of 135 HIV-negative individuals (110 women and 25 men) in a sexual relationship with a person with HIV, in a study in Spain conducted between 1990 and 2000.Citation52 Oral sex on a woman is considered even lower risk than on a man, and avoiding menstrual blood is sometimes suggested.Citation51 Minimising risk can be achieved by use of condoms or other latex or polyurethane barriers over the vulva or anus, avoiding oral sex when the positive partner is likely to have higher viral loads and may be more infectious, when there is inflammation caused by common throat infections, allergies or STIs such as gonorrhoea, or bleeding gums or sores in the mouth or throat of the recipient, and avoiding ejaculation into the recipient's mouth if the giver is HIV positive.Citation53
A 2005 study demonstrated the ability of HIV antiretroviral therapy to reduce heterosexual transmission of HIV in discordant couples by 80%Citation48 but the investigators and others have cautioned that even a small increase in sexual risk-taking could cancel this out. Moreover, while mathematical modelling has also shown that reduced viral load may reduce risk in individual cases, in settings such as Uganda, with limited access to antiretroviral therapy, and because only people with advanced disease receive therapy, it is unlikely to have an impact on the epidemic at population level.Citation49
The cervix is the primary site of infection for gonorrhoea, chlamydia and human papillomavirus and has more HIV receptors than the vagina.Citation54 Cervical barriers such as the diaphragm and cervical cap have been in use for decades for contraception. The diaphragm has been shown to decrease rates of gonorrhoea, chlamydia and pelvic inflammatory disease and results are pending of a clinical trial of the All-Flex diaphragm to prevent HIV transmission.Citation55Citation56 Newer barrier devices are also now available.
Anal sex practices are rarely addressed in sex education on the assumption that they do not happen, or at least not with women, and sex between men and transgender people may not be discussed at all. Yet a review of studies in the USA in 1999 on heterosexual anal intercourse showed in absolute numbers that approximately seven times more women than homosexual men had experienced unprotected anal intercourse.Citation57
Anal transmission of HIV from an HIV positive man to a receptive partner, male or female, is the highest risk mode of HIV transmission, after blood-to-blood transmission. In a number of countries adolescents have reported having anal sex to avoid pregnancy or to preserve virginity.Citation41 In South Africa, 42.8% of a sample of women sex workers had anal sex with their clients. HIV prevalence in this group was 61.3% compared to 42.7% in those who did not engage in anal sex, controlling for age, number of clients per week and duration of sex work.Citation58 Unprotected receptive anal intercourse is ten times more risky than unprotected vaginal intercourse for acquiring HIV because anal mucosa is more delicate and easily damaged during penetration.Citation59 Tearing of rectal tissue, haemorrhoids, proctitis and other anal lesions have been experienced by some men who have sex with men and also increase risk.Citation60
Vaginal douching may remove natural fluids and bacteria such as lactobacilli which maintain the natural environment and pH of the vagina. Natural vaginal lubrication during sexual arousal facilitates penetration, with or without condoms. Negative associations of natural vaginal wetness with promiscuity in some cultures should be addressed. Water-based lubricants and saliva make vaginal and anal sex safer and are especially needed by sex workers and others for repeated acts of intercourse. They can also make sex more pleasurable. Water-based lubricants should be used with condoms, especially for anal sex, to prevent damage to anal tissue and condom breakage.Citation61 Health workers and women need information on the dangers of inserting substances into the vagina to make it tight, dry or “hot” with astringents, detergents, bleach, chillies, bark and other substances.Citation62
Recent results from three randomised trials in Africa show partial protection (50–60% reduction in risk) from female-to-male vaginal transmission of HIV for HIV negative men who undergo male circumcision.Citation63–65 Consideration of male circumcision is particularly appropriate for women with HIV and their male partners who are untested or negative. No protective effect of male circumcision for women has been shown, and recruitment for the one trial looking at this issue was stopped early because of higher HIV incidence among the female partners of circumcised men compared to the uncircumcised control group.Citation66 Messages and counselling should stress that resumption of sexual relations before complete wound healing may increase the risk of acquisition of HIV infection among recently circumcised HIV negative men and may increase the risk of HIV transmission to female partners of recently circumcised HIV positive men.Citation66Citation67
A partially effective intervention that protects men but not women could result in increased HIV transmission if circumcised men do not maintain or initiate use of condoms or if they have more partners. WHO/UNAIDS advise that “any decisions about male circumcision must take into account cultural factors, risk of complications, potential to undermine existing protective behaviours and prevention strategies and health system constraints”.Citation67
Based on the currently available evidence, male circumcision is not recommended for HIV positive men as an intervention to reduce HIV transmission to women; nor is there information on the safety of male circumcision for HIV positive men, especially those with advanced immune suppression. Research has not yet been done on whether there is any protective benefit of male circumcision for sex between men when one is HIV positive, nor in heterosexual anal sex.Citation67
Condom use
UNAIDS, WHO and UNFPA emphasise that condoms are central to all STI and HIV control strategies.Citation68 The common notion among family planning providers that condoms are only for disease prevention because they are less effective than other contraceptive methods fails to take into account the potential for increasing the number of protected sex acts when their contraceptive potential is also stressed. Due to successful social marketing efforts, condom promotion in Africa has been a success for single women, including for pregnancy prevention, which the main or partial motive of most single women who use condoms even if the risk of HIV/STIs is high. The needs of the married and cohabiting population have been neglected by researchers and programme staff alike, despite the fact that more than half of HIV infections in the severe epidemics of southern and East Africa are occurring in this group. Yet the barriers to condom adoption by married couples may not be as severe as is often assumed.Citation69
Misleading and factually incorrect statements about condom effectiveness are increasingly found in health education materials supported by faith-based organisations opposed to sex outside marriage and to contraception.Citation7 Christian conservatives in the USA want condom labels to warn of the risk of infections rather than their high effectiveness on preventing infection if used consistently and correctly, and state-funded abstinence-only programmes only allow mention of condoms in the context of their failure rate.Citation70 Deliberate misinformation seriously undermines prevention efforts, sows confusion and threatens condom availability and use – which in turn promotes HIV transmission.
Male latex condoms are 80–95% effective in preventing HIV and most STIs when used consistently and correctly.Citation71–73 Condoms are impermeable to infectious agents in genital secretions.Citation58,72,74,75 They reduce the risk of transmission of human papillomavirus (HPV) and therefore of cervical and ano-genital dysplasia and cancer.Citation70,76,77 They also reduce the risk of transmission of herpes simplex virus-2, although some transmission can still occur through non-penetrative sex and through skin not covered by a condom.
Using a lubricant with male condoms is important for post-menopausal women, who have less natural vaginal lubrication, and for women sex workers and others who are having multiple and/or rapid intercourse with one or more persons, which can cause discomfort and even pain with condoms alone, because the vagina may not produce adequate natural lubrication. Lack of stimulation and psychological depression can contribute to vaginal dryness as well. This sometimes leads to condom breakage and an increase in vaginal tearing, thereby increasing the risk of STI/HIV transmission.Citation61 Anal sex should always be protected by condoms and a water-based lubricant should always be used to prevent friction, as the anal passage does not have its own natural lubrication like the vagina does, and condom breakage.Citation78
Female condoms come with lubrication. Female condoms used consistently and correctly are estimated to be 94–97% effective against STIs. While they have not specifically been studied for HIV prevention, effectiveness is assumed to be comparable.Citation68 Despite limited access and high cost, female condoms are becoming more popular with some women, who are able to negotiate their use with some men.Citation43 Newer versions of female condoms have been developed, including a more affordable nitrile version by the Female Health Company,Citation79 and PATH are also testing a new model of female condom.Citation80 More investment is needed for mass production, support for advocacy groups who can advise on use, and training for health workers to promote them.
There is anecdotal evidence from many countries that men who have sex with men successfully use female condoms anally for protection. In a 1998 survey of more than 2,200 HIV positive men in the USA, a majority said they were very likely or somewhat likely to use the Reality female condom for future receptive and insertive anal intercourse. 54% of those surveyed actually preferred using the Reality condom to the male condom. A redesigned product may be preferable for anal intercourseCitation81 but none has emerged in the decade since.
Difficulties using condoms, which occur mostly for new users, should be acknowledged and practical suggestions given on how to overcome them.Citation82 Men may lose their erection when putting a condom on, especially when they first start using condoms, and may not persist with them for this reason (Juliet Richters, National Centre in HIV Social Research, Sydney, Australia. Personal communication, October 2006). It is worth suggesting that men practise on their own before trying them with their partners, and the same could be said for female condoms, but trying with a partner and making it a joint learning adventure may help to sustain use by introducing them as part of sexual intimacy from the start.
Focus on pleasure
“There is growing evidence that promoting pleasure in male and female condom use, alongside safer sex messaging, can increase the consistent use of condoms and the practise of safer sex. This is the ‘power of pleasure’.” Citation78
The emphasis in HIV programmes on disease and disease prevention, sexual violence, infidelity and difficulties in promoting condoms can be overwhelming. Being labelled as “infected” injures a person's sense of identity, often making them feel they have no right to a fulfilling relationship or to being “normal”. Most HIV positive women and men are healthy, and those on antiretroviral treatment have in large numbers got their health back. Most are or will be having active sexual lives, just as young people with HIV want to explore relationships as much as their negative peers. Promotion of safer sex can be done in a sex-positive way, rather than trying to frighten people. Emphasis on sex as pleasurable, condoms and lubricants as erotic and non-penetrative sex as exciting should be used more often to encourage safer sex. The Pleasure Project has mapped programmes, literature, research and training using pleasure as a primary motivational force, particularly in resource-poor settings.Citation61Citation78
Many gay men's organisations in the US, UK, Canada, Australia and other developed countries have taken a pleasure approach to HIV prevention and teach men how to make condoms feel better and integrate them into sex play. The Australian Federation of AIDS Organisations, for example, created Sex in Queer Places, an interactive video game that follows a fictional gay man through a variety of sexual encounters (e.g. sauna, dance party) and lets the viewer make a set of sexual and drug-use choices. With each choice a dialogue box pops up with health promotion and harm minimisation information.
An electronic booklet that takes a sex-positive approach to issues about sex for HIV-positive men is also included (<www.afao.org.au>). Often, the target audience have their own innovative ideas for eroticising condoms and increasing their use.Citation78
Pleasure and sexiness are often culturally specific, so it is vital to tailor pleasure-focused HIV prevention to the needs and desires of target communities. For example, in Mumbai, India, the Sambhavana Trust reported that some of the hijra (transsexual) community were inserting the female condom anally before sex and explaining to their penetrative partner that they were using the female condom as proof of their femininity.Citation78
Safer sex in HIV serodiscordant and seroconcordant relationships
HIV negative partners of people with HIV are at high risk for HIV infection but they are often not the focus of prevention programmes, especially married couples, and condoms are rarely promoted to them. In a French study of 575 sexually active HIV positive women of reproductive age who knew the serologic status of their steady partners, consistent condom use was six times higher in serodiscordant couples than in seroconcordant couples (odds ratio=6.1, 95% CI=0.1-0.2, p<0.001).Citation83 High levels of consistent condom use (73%) were reported in a 2003 Swiss study of HIV serodiscordant couples and in the Swiss HIV Cohort Study, the level was 88%.Citation84 On the other hand, among 145 HIV serodiscordant couples in the USA, 45% reported having had unprotected vaginal or anal sex in the six months prior to the study. Unsafe sex was associated with lower educational level, unemployment, African-American ethnicity, practice of anal sex by the couple and injection drug use. Consistency of condom use did not depend on the sex of the HIV positive partner or duration of the sexual relationship. The findings suggest that many HIV serodiscordant heterosexual couples remain at high risk of HIV transmission and may benefit not only from safer sex interventions but also from interventions aimed at improving their social and economic conditions.Citation85
In areas of high HIV prevalence in sub-Saharan Africa, e.g. Zimbabwe, 5–10% of women become HIV infected during pregnancy and breastfeeding.Citation86Citation87 Where a male partner's HIV positive status is known, condom use during pregnancy and breastfeeding can be introduced to prevent HIV infection of the woman if she is negative but also parent-to-child transmission to the unborn baby which is a much greater risk when the mother is infected while pregnant. Encouraging men to share this responsibility may normalise condom use in marriage so that discordant couples continue to use them after the perinatal period. During breastfeeding, additionally, condom use is a safe means of preventing another pregnancy.
In a study among homosexual men with a regular partner in France, 285 reported a serodiscordant partner and 193 a seroconcordant partner. Unprotected sex was reported by a higher number of those in seroconcordant (46.7%) than serodiscordant couples (15.6%). In both kinds of partnerships, unprotected sex was significantly more frequent when episodes of unprotected sex with casual partners were reported. In seroconcordant couples, those who had more than four casual partners were also more likely to practise unprotected sex with their regular partner. Among sero-nonconcordant couples, binge drinking and absence of disclosure of HIV-positive status to the partner were also independently associated with unprotected sex. Absence of disclosure of HIV positive status to the partner was also independently associated with unprotected sex. The relationship between unprotected sex with both casual and regular partners thus appeared to be related to the underlying psychosocial and interactional factors that may influence sexual behaviours of people living with HIV in regular relationships, independently of the status of the partner.Citation88
Re-infection in HIV concordant couples
The question of whether people with HIV can re-infect each other and whether such re-infection causes progression to AIDs more quickly has been around since the beginning of the epidemic. Conventional advice given to HIV positive concordant couples emphasises consistent condom use for all sexual intercourse for the rest of their lives because of the dangers of re-infection.Citation89 However, information about re-infection between seroconcordant partners is still extremely limited, making the evidence for this advice uncertain. The main concerns are that dual infection (with two or more viral strains, in the case of multiple positive partners) may lead to more rapid disease progression and that recombinant drug resistant viruses may occur. Re-infection means: i) co-infection with another strain of HIV at the same time or within a month of the initial HIV infection, or ii) super-infection with a second HIV strain some time after the initial infection has become established. Only 16 cases of re-infection have been reported in the literature since the first case in 2002,Citation90Citation91 and as detecting re-infection is technically difficult, the frequency is quite possibly under-estimated. Studies of super-infection have recently begun. At the International AIDS Conference in 2006 Dr Julie Overbaugh reported in a plenary presentation on eight potential cases of super-infection among a cohort of HIV positive women in Mombasa, Kenya, that had occurred after an antibody response had had time to develop (2–5 years).Citation92
Many women and men with HIV are seeking relationships with positive partners (called “sero-sorting”) in an attempt to avoid HIV transmission to negative partners and having always to use condoms. Given the difficulty of sustaining consistent lifelong condom use, this is a rational response. Condom use between HIV concordant partners may need re-thinking, especially for those who have no STIs, are reliably monogamous and if heterosexual and not wanting a child, using other contraception.Citation93 In the CAPRISA Project in South Africa, they have stopped counselling such concordant couples to use condoms (Personal communication, Salim Abdool Karim, CAPRISA Project KwaZuluNatal, South Africa, March 2006). The greater challenge is how to increase safer sex between partners who are not concordant or monogamous.
Antiretroviral therapy and safer sex
Reports of increasing unprotected intercourse associated with poor adherence to antiretroviral therapy in the USA and Europe have given rise to fears that being on treatment, “safe-sex fatigue” and perceptions of HIV as treatable and chronic will result in increased risk-taking behaviours.Citation94Citation95 However a literature review found that the prevalence of unprotected sexual intercourse was not higher in HIV positive people on antiretroviral therapy than in those who were not, nor in those with undetectable vs. detectable viral load.Citation96 Regardless of HIV serostatus, however, the likelihood of unprotected sex was higher in people who perceived that receiving antiretroviral therapy or having an undetectable viral load was protective against transmitting HIV.
Encouragingly, some studies have found a relationship between high adherence to antiretroviral therapy and safer sex behaviours: in California HIV clinics with diverse populations, use of and adherence to antiretroviral therapy >95% and undetected viral load were significantly associated with a decrease in unprotected vaginal and anal sex.Citation97 In a London outpatient clinic, HIV positive homosexual men on antiretroviral therapy consistently reported lower behavioural and clinical risk factors than men not on treatment.Citation98 A recent study in Uganda found that provision of antiretroviral therapy along with prevention counselling and partner testing and counselling reduced sexual risk behaviour by 70% after six months.Citation99
Antiretroviral “treatment literacy” for both health care providers and people with HIV is essential for treatment to be effective. Treatment literacy education should include messages that include pleasure-based safer sex information and emphasise:
| • | the benefits of treatment adherence (better health, reducing the need to change treatment regimens, preventing development of drug-resistant virus); | ||||
| • | the continuing need for safer sex because although improvements in health (higher CD4 counts and lower or undetectable viral loads) do reduce the risk of sexual transmission of HIV they do not eliminate it; | ||||
| • | antiretroviral therapy is not a “cure” for HIV, and | ||||
| • | there is a continuing risk of other STIs with unprotected sex. | ||||
As access to antiretroviral therapy increases in developing countries, while second and third line drugs remain extremely limited, strategies to support adherence and sustained safer sex are critical to avoid resistant HIV strains emerging.
Regular screening and treatment for STIs
STIs cause considerable morbidity and mortality, and are powerful cofactors that facilitate HIV transmission and acquisition from 10–300 times per sex act, especially with genital ulcer disease.Citation100–102 STI treatment can be carried out in two ways: i) population-level interventions to reduce STI prevalence and lower HIV transmission efficiency, and ii) STI services to address the health needs of individual people, with and without HIV, which are usually based on symptomatic individuals seeking treatment.
Sexual transmission of HIV is most widespread in the same regions as those with poorest STI control, where curable STIs (chancroid, syphilis, gonorrhoea and chlamydia) predominate. An appropriate strategy includes targets to lower curable STI prevalence, minimise complications (which can be more severe in people with HIV), and slow further HIV transmission. Thailand and Cambodia successfully implemented national-level interventions that resulted in large reductions in curable STIs and helped to reverse the growth of their HIV epidemics.Citation103–105 Key elements of success included condom promotion, improved STI services and targeting sex workers and clients with effective preventive and curative services. Similar results have been reported from Senegal, Kenya and elsewhere.Citation106,107 Once basic STI services are strengthened, curable STIs can be rapidly controlled and incurable viral infections (herpes simplex virus-2) and human papillomavirus assume greater importance. Herpes is incurable but suppression with daily acyclovir is currently being studied for its effect on HIV prevention.Citation108 Effective STI control requires interventions that reach sexual networks with the highest rates of sexual partner change.Citation109–111 Successful interventions combining peer outreach and clinical services including STI screening and/or presumptive treatment have reported marked reductions in STI prevalence among sex workers in Africa,Citation112–115 Latin AmericaCitation116 and Asia.Citation117
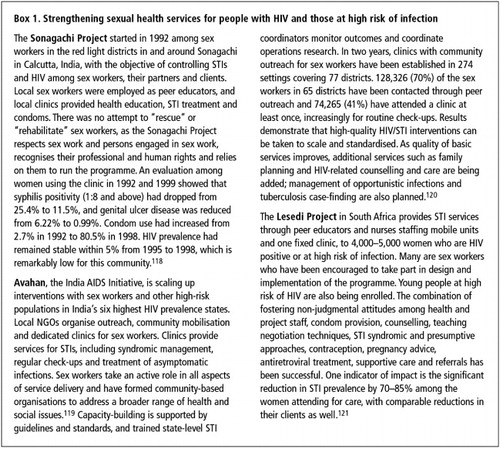
Sex workers have special service needs for STI prevention and detection. Over half of sex workers, many of whom are HIV positive, have curable STIs but are unable to access health services for diagnosis and treatment, and unable to insist on condom use with clients.Citation111 In successful programmes, services are offered at convenient places and times, along with other needed services such as contraception, HIV care and treatment, and support for advocacy to prevent police harassment and ensure that the rights of women are respected by brothel owners (Box 1). Although some programmes were originally intended for female sex workers, male sex workers (who are even more highly stigmatised) have also been attracted to utilise them. Frequent STI exposure is a real and ongoing hazard of sex work that should be addressed through counselling, regular genital examination and six-monthly screening for syphilis. The conditions that frequently lead to sex work, especially poverty and lack of economic alternatives, are aggravated by HIV infection.
Repeated STIs challenge the immune system of HIV positive people, reducing their capacity for staying healthy. People with HIV need to know the risks to their health associated with STIs, be encouraged to seek treatment early for symptoms and advised on increased HIV risk to negative partners. Per sex act, men are twice as likely to infect women with a variety of STIsCitation47 and four times more likely to infect them with HIV as women are to infect them.Citation122 The common sequelae of STIs in women – pelvic inflammatory disease, ectopic pregnancy, congenital infections – and ano-genital cancers and infertility in both women and men may be aggravated by HIV infection.Citation123 Other infections of the reproductive tract, including chronic candida vulvovaginitis and bacterial vaginosis, although not sexually transmitted, are also problems for HIV positive women.
Extensive, persistent herpes simplex virus-2 infection is a sign of late-stage AIDS (WHO clinical stage 4).Citation89 Systematic screening for asymptomatic infection (serologic test for syphilis, speculum/bimanual examination with tests for cervical infection, where feasible, and cervical cancer screening) should be an integral part of routine HIV care for women.Citation124 Services providing HIV testing and counselling, antenatal care, prevention of parent-to-child-transmission and treatment for tuberculosis should develop STI screening programmes that include referral or treatment. Syndromic case management is challenging for women because vaginal discharge is over-diagnosed as an STI, resulting in stigma and over-treatment in women who may have endogenous vaginitis.Citation125 Lack of good diagnostic tests for gonorrhoea and chlamydia at point of care and appropriate for resource-poor settings remain a critical unmet need, especially for women..Citation126 Prices of highly effective single dose treatment for gonorrohoea, chlamydia, and genital ulcer disease (azithromycin, ciprofloxacin, cefixime) have dropped in the past decade but these and other appropriate medicines for treating bacterial STIs continue to be available intermittently or not at all in many STI programs in developing countries. Poor drug supply management, weak health infrastructure and lack of political support for STI control contribute to continuing STI epidemics in the same populations where HIV prevalence is highest.
HIV seroconversion is a time of high viral load and infectiousness. A person who acquires an STI may have been simultaneously exposed to HIV. A recent study in Malawi found that 2% of men presenting to clinics with symptomatic STIs and negative for HIV antibodies were found to be in the process of acute HIV seroconversion with significantly higher viral loads than those who tested positive for HIV.Citation127 HIV testing and counselling should routinely be offered as part of STI services; those who test positive should receive intensive prevention counselling and support. People diagnosed with STIs similarly need intensive education that they may be in the window period of HIV infection and need a repeat HIV test in 6–12 weeks, and could pass HIV on to partners if they have unprotected sex. All people at risk of STIs through unsafe sex need to use safer sex methods consistently. This is potentially harder for those whose risk comes from their partner's behaviour rather than their own.
Human papillomavirus, cervical and ano-genital cancers
Cancer of the cervix and ano-genital cancers in women and men are a complication of persistent infection with oncogenic strains of human papillomavirus (HPV). Lower-risk strains of human papillomavirus cause benign genital warts on the lower genitalia and anus in both sexes. They can be severe and persistent in people with HIV, but eventually resolve spontaneously without treatment.
Globally up to 80% of newly sexually active men and women may be exposed to oncogenic strains of HPV, but most develop only transient infection. In a small percentage of women, HPV infection progresses to cervical intraepithelial neoplasia (CIN), a pre-cancerous condition that either regresses or progresses to invasive cancer.Citation128 Anal intraepithelial neoplasia (AIN) caused by HPV occurs with the same frequency in men who have sex with men as cervical cancer does in women and is probably higher among those with HIV.Citation129 A study of over 100 women with CIN and their male sexual partners indicated that consistent condom use can speed up regression of HPV-associated lesions, clearance of HPV in women and regression of flat penile lesions in men, presumably by blocking repeated transmission and re-infection between partners.Citation130,131
Large-scale multi-country, multi-site trials of several HPV vaccines are underway.Citation132 A vaccine that is 90% effective against two oncogenic HPV strains, 16 and 18, causing about 70% of cervical cancer, has been evaluated and approved in the USA and Europe for use in (young) women.Citation133,134 There is currently a lack of knowledge of the prevalence of specific HPV types in women and men with HIV. Between 1996 and 2003 in the USA, of 202 HIV positive women who were receiving routine HIV care, 105 were positive for HPV, of whom 52% were positive for multiple types of HPV. Women in this study were often infected with different strains of the virus from the ones covered by the new vaccine, which were also associated with a high risk of pre-cancerous and cancerous cell changes.Citation135
No data are yet available on the safety and efficacy of HPV vaccines for people with HIV, whether infected perinatally or sexually. Studies have found that women with HIV have a two- to six-fold increased risk of pre-cancerous cervical cell abnormalities,Citation136–138 and can develop invasive cervical cancer up to ten years younger than HIV negative women.Citation138 Progression to high-grade lesions is more rapid, and lesions are more resistant to treatment in the presence of HIV.Citation139–141
In women with HIV, lower genital tract cancers in the vagina and vulva, and cancers of the anus in women who have receptive anal sex are also prevalent. Overall, however, increased rates of invasive cervical cancer have not been associated with the HIV epidemic.Citation142 In 1992 the US Centers for Disease Control classified cervical cancer as an AIDS-defining illness. This is now being questioned since the relationship of cervical cancer to declining immune function, as determined by CD4 cell count and responsiveness to antiretroviral therapy, is unclear.Citation143
In the context of population-based cervical cancer control programmes, WHO recommends that women with HIV be offered cervical screening at the time of HIV diagnosis and thereafter “at the same frequency and with the same screening test as women not infected with HIV”.Citation124 Once screened, a woman with an abnormal test should be followed up and/or treated. HIV positive women with cervical dysplasia also have a higher incidence of other lower genital tract cancers; they, and men with HIV, should be screened on a regular basis by visual inspection of the genitalia for abnormal tissue or lesions, which should be biopsied, followed up and/or treated as well.
Since the HIV epidemic, the incidence of AIN in men who have sex with men is increasing. Screening in HIV positive and HIV negative men who have sex with men for anorectal malignancies or dysplasia is cost-effective if the incidence is sufficiently high. Treatment options range from watchful waiting for asymptomatic grade-1 AIN to excision or radio(chemo)therapy for anorectal carcinoma.Citation144
All available screening methods, cytology, HPV DNA testing and visual inspection, are appropriate for people with HIV. As most HPV infections resolve spontaneously by age 30–35, HPV testing before that time is not useful as a screening test.Citation146 High grade pre-cancerous lesions (CIN 3) require treatment but this is complicated by poor outcomes, especially for women with CD4 counts below 200. However, women with HIV should be offered treatment and followed closely for complications, recurrence or persistence of lesions.Citation145 Low-grade abnormalities (CIN 1 and 2) do not require treatment, but women with HIV need to know they require closer follow-up because of risk of rapid progression.
Evidence on the impact of antiretroviral therapy on HPV disease in people with HIV is mixed.Citation146 Cancer incidence data in North America, Europe and Australia showed no significant change in incidence rates for cervical cancer but the number of cancers was very small.Citation147–149 Regression of cervical lesions as immune function improves has been noted in several studies.Citation150,151 Other studies have showed a dose–response relationship between decreased immune function and increased severity and persistence of CIN.Citation152,153 Early data suggest that most anal high-grade lesions do not regress after an individual begins antiretroviral therapy, but may take several years to show a comparative difference with HIV negative men and women.Citation154 Given these data, it is important that those who are eligible have access to antiretroviral treatment.
Integration of cervical and ano-genital cancer control into sexual health programmes for people with HIV would include giving information on primary HPV prevention as part of sex education to young people with HIV who are not yet sexually active, and for women, alertness to persistent vaginal discharge or spotting unresponsive to treatment (possibly the only symptom of early cervical cancer). It would also include integrating screening into HIV care and sexual and reproductive health programmes where there is access to treatment. Ideally, HIV positive women and men should receive cervical and ano-genital screening and treatment along with contraception and STI services from a combination of enhanced public sector and research-focused clinical services.Citation155 Women and men with HIV have real concerns about the impact of cervical and ano-genital disease on their health, which services should do their best to address. But it is unrealistic to expect complex multi-level services to be set up for them in the absence of national guidelines and services, particularly for cervical cancer prevention for the general population. Screening is not helpful if proper diagnosis, follow-up, treatment and care for abnormalities are unavailable; it is only through well-planned provision of services at the central level that people with HIV will benefit.Citation145
Addressing sexual dysfunction
The sexuality of men and women with HIV is diminished by the fear of infecting others and being infected, as well as guilt, anger and ill-health resulting in negative physical and psychological effects on sexual desire. Men with HIV are not uncommonly concerned about sexual dysfunction, including loss of libido, problems with erections and ejaculation, which may be related to illness or opportunistic infections, certain antiretroviral drugs or other medications. Poor treatment adherence and sexual dysfunction have also been reported.Citation156–158 Men with sexual dysfunction have also commonly reported recreational drug use, co-infection with hepatitis B and C, anxiety and depressive illnesses, peripheral neuropathy and lipodystrophy.Citation159 Health care providers can provide some reassurance that improvement in health will address some sexual dysfunction. Treating STIs, addressing concerns and providing simple behavioural interventions could increase positive men's confidence. Health staff need skills in sympathetic and knowledgeable responses to such problems, in particular to raise these issues in counselling so that men with HIV continue to comply with their treatment.
Retrospective analysis of clinic notes of women with HIV attending an HIV clinic in London that offered a sexual dysfunction service for men with HIV found that about half the clinic's cohort of women patients reported sexual problems, most commonly from contextual causes, or were not satisfied with sex in the preceding 12 months. A survey by letter of HIV clinical centres in the UK found that 60% had rarely or never asked women patients with HIV about sexual functioning.Citation160
Policies, programmes and health services
There are increasing calls for men's sexual health to be better addressed for their own sake as well as that of their partners and families.Citation161,162 Although this may slowly be changing among some men in many cultures, men mostly still hold the power to make decisions about pregnancy, contraception, safer sex and when to have sex and with whom, and their choices may be based on limited knowledge. Peer pressure and cultural norms and expectations, such as pressure to have early sexual experiences, for which they may not be prepared, having multiple partners and even expressing sexual violenceCitation163,164 serve to limit and undermine HIV prevention efforts.
Lack of knowledge of reproductive biology, including the physiology of sexual response, fertility, the menstrual cycle, biological vulnerability to HIV/STIs their effects on pregnancy, contribute to poor attention to sexual health, dissatisfaction with sex and failure to realise reproductive goals.Citation165 Sexual health education is more targeted at women through health talks, posters and leaflets when they attend family planning clinics and antenatal care, or with children for immunisation. Women educate each other through social networking. Men are also interested in receiving scientifically-based information directly from clinics, rather than through their wives or partners.Citation166
Men tend to use services where health education is not the norm, such as STI clinics, workplace clinics, private or informal health services when clinic hours clash with work. They also tend to prefer the private sector, where they are less likely to be “scolded” by staff for having STIs and where they have more privacy. Services for women that include men as partners, such as antenatal care, by their nature exclude young, single men and men who have sex with men, and other marginalised groups, whose concerns are usually hidden because of stigma. Like women, men often feel stigmatised when their only option for care is a designated STI clinic. A study in India, for example, found that men preferred going to a “male clinic” which provided more than STI care.Citation156 Programmes have to fit in with people's working times, discard punitive approaches, ensure confidentiality and use alternative settings, ranging from community-based groups, social and sports facilities to workplaces, drinking spots and bars.Citation167 Peer education and social networking approaches are highly suited to young people, injecting drug users, sex workers and men who have sex with men.Citation168
Developing countries rely on sexual health research and therapeutic interventions often developed in better-resourced environments. As these interventions become more widely available, international and national programmes will need to incorporate them in ways that are responsive to HIV-affected people. Programmes have to become more people-centred, more courageous and flexible, and less punitive and conservative, always focusing on public health interventions with known effectiveness.
Current developments in HPV vaccination and screening could eventually transform cervical and ano-genital cancer prevention, but the relevance to people with HIV needs to be clarified. As regards STIs more generally, in 2006 the World Health Assembly endorsed the Global Strategy for the Prevention and Control of Sexually Transmitted Infections for 2006–2015.Citation169 Although it is cast almost entirely in the mode of prevention of HIV and does not deal with STIs in people living with HIV, it does underline the importance of having quality, up-to-date drugs always available and well-equipped STI services able to carry out both diagnosis and treatment, which are critical for maintaining the health of people living with HIV.
Cervical barriers and female condoms have been available for many years but are still not widely available because of funding shortages and low political will, despite widespread support and calls for women-initiated methods. Microbicides include a range of topical products (they can be gels, creams, films, or suppositories) that are under development. They are intended to interrupt HIV transmission in both semen and vaginal secretions, and to reduce the risk of some STIs when applied vaginally or rectally prior to sex; some may also prevent pregnancy. Research has been ongoing for a number of years, but there have been setbacks, most recently the discontinuation in early 2007 of the Phase III effectiveness trials of cellulose sulfate because of safety concerns. Several other Phase III trials of vaginal microbicides evaluating the effectiveness of products to prevent vaginal transmission of HIV to women are ongoing or due to start, and advocates have stressed the importance of continuing this research. Further studies will be needed of effectiveness for preventing transmission from HIV positive women to HIV negative male partners and for safety and effectiveness for anal sex. Another promising line of research is chemoprophylaxis which, if successful, would involve an HIV negative person taking an antiretroviral to interrupt HIV transmission during and after sex. None of these potential products is likely to be available in the coming few years.Citation170–172
Interventions that are currently available need more intensive lobbying. National policies that clearly state the scientific and public health rationale for promoting and distributing condoms in HIV/STI programmes need far greater encouragement from international public health, sexual health and HIV/AIDS agencies and donors. Far greater support for condom social marketing efforts is also needed. Promotion of consistent, correct use of male and female condoms for “dual protection” against pregnancy and infection needs also strengthening, particularly among heterosexual couples affected by HIV. Condoms should be universally available, free or at low cost, along with measures to decrease barriers to their use.
People living with HIV need more confidence that their sexual health and rights will be respected. To this end, governments must be encouraged to develop policies, laws and guidelines that protect confidentiality and informed consent as well as stating clearly the limited circumstances in which partner disclosure may take place without consent. Advocacy by civil society organisations to implement policies, strategies and legislation already in place is essential for governments and leaders to show they are accountable for the protection of women and men living with HIV.
Policies developed at national and regional level by governments, local experts and civil society in conjunction with young people, men and women living with HIV have demonstrated effectiveness. Examples are 100% condom and STI policies in southeast Asia;Citation103 treatment literacy and advocacy in South Africa, Brazil and many developed countries; integration of cervical cancer screening into sexual and reproductive health services in Zimbabwe; sex worker peer education in India, Nigeria, Kenya, Thailand, Mexico and Dominican Republic. Evidence shows that coordinated approaches linking strategies for antiretroviral adherence to support for practising safer sex and reducing risky sexual behaviours, and programmes that address the broader sexual health concerns of HIV positive
men and women can all help to sustain health gains for people living with HIV.
Conclusion
In many ways the challenges faced by people living with HIV in achieving sexual health are the same as for everyone living in resource-poor settings, and depend on good health services and systems. The added vulnerability of women and men with HIV because of stigma, social vulnerability and illness needs to be addressed in ways that are supportive and enabling rather than discriminatory. This paper argues for the need for appropriate health services and targeted education, advocacy for the development of enabling policies and support for positive prevention for people with HIV. Investment is needed in training health workers to provide services within a professional ethos of respect and dignity, taking into account the diversity of sexual relationships and partnerships, and people's different needs at different stages in their lives, starting in adolescence. Involvement of people with HIV as active partners in development of policy, programmes and services will encourage ownership, enhancing quality of care within both resource-rich and resource-poor environments. At the same time, advocacy and activism will remain essential to guarantee that new technologies and therapies are accessible for HIV positive people in developing countries, especially those countries with a high prevalence of HIV.
Notes
* These definitions were elaborated in a WHO-convened international technical consultation on sexual health in January 2002, and subsequently revised by a group of experts from different parts of the world. They are not official WHO definitions, and should not be used or quoted as such.
References
- Report of a Technical Consultation on Sexual Health. 28-31 January 2002. 2006, WHO. Geneva. At: <www.who.int/reproductive-health/gender/sexual_health.html#3. >. Accessed 17 March 2007.
- International Community of Women Living With HIV/AIDS Gender Aids Forum ICW Durban. Confronting marginalization together in the context of HIV/AIDS. At: <www.icw.org/node/46. >. Accessed 7 December 2006.
- International HIV/AIDS Alliance. Positive Prevention: prevention strategies for people with HIV/AIDS. Emerging Practice Series. Draft background paper, July 2003. At: <www.aidsalliance.org/sw9438.asp. >.
- R Bunnell, J Mermin, KM De Cock. HIV prevention for a threatened continent: implementing positive prevention in Africa. JAMA; 296(7), 2006:855-858.
- Global consultation on the rights of people with HIV to sexual and reproductive health, Addis Ababa, 27–30 March 2006. At: <www2.who.int/reproductive-health/hiv/final_global_consultation.pdf. >. Accessed 15 March 2007.
- Positive Outcomes, Finding HIV positive youth and bringing them into care. 2005, AIDS Alliance for Children, Youth and Families. Washington DC. At: <http://aids-alliance.intrasmart.com/isdoclibrary/files/951839/957442/20053261598389/Finding%20HIV-Positive%20Youth.pdf. >.
- M Garvey. Dying to learn: young people HIV and the churches. Christian Aid, October 2003. At: <www.christian-aid.org.uk/indepth/310learn/dyingtolearn.pdf. >.
- ML Ybarra, J Kiwanuka, N Emenyonu. Internet use among Ugandan adolescents: implications for HIV intervention [abstract]. PloS Medicine; 3(11), 2006:e433.
- International Community of Women Living With HIV/AIDS. HIV Positive Women in Thailand: Their Voices and Choices. A Study Conducted by and for HIV Positive Women. At: <www.icw.org/files/Voices_and_Choices_Thailand.pdf. >. Accessed 30 November 2005.
- Kirby D. Emerging answers: research findings on programmes to reduce teen pregnancy. Washington DC: National Campaign to Prevent Teen Pregnancy, 2001. p. 5, 88–91..
- J Manlove, A Romano Papillio, E Ikramullah Not yet: programmes to delay first sex among teens. 2004, National Campaign to Prevent Teen Pregnancy. Washington DC.
- M Gallant, E Maticka-Tyndale. School-based HIV prevention programmes for African youth. Review. Social Science and Medicine; 58(7), 2004:1337-1351.
- R Magnani, K Macintyre, AM Karim. The impact of life skills education on adolescent sexual risk behaviours in KwaZulu-Natal, South Africa. Journal of Adolescent Health; 36(4), 2005:289-304.
- US Government Accountability Office, Report to Congressional Committees. Global Health: Spending Requirement Presents Challenges for Allocating Prevention Funding under the President's Emergency Plan for AIDS Relief. GAO-06-395April 2006, US GAO. Washington DC.
- G Gordon, V Mwale. Preventing HIV with young people: a case study from Zambia. Reproductive Health Matters; 14(28), 2006:68-79.
- P Bearman, H Bruckner. After the promise: the STD consequences of adolescent virginity pledges, 2004. At: <www.yale.edu/socdept/CIQLE/cira.ppt. >.
- Eyes Wide Shut – sexuality and risk in HIV-positive youth in Sweden: a qualitative study Scandanavian Journal of Public Health; 35(1), 2007:55-61.
- United Nations. General Comment No.3 (2003). HIV/AIDS and the rights of the child. Thirty-second session 13–31 January 2003. CRC/GC/2003/3. 17 March 2003. Quoted in Bosmans et al..
- Médécins sans Frontières South Africa Internal newsletter. February–June 2005. At: <www.doctorswithoutborders.org/news/southafrica.cfm. >.
- UN Development Programme. Training HIV/AIDS positive youth to enhance their potential for employment. (no date). At: <www.undp.org.za/projects/training_hiv.html. >.
- J Augustine Serving HIV-positive youthNovember 2002, Advocates for Youth. Washington DC. At: <www.advocatesforyouth.org/PUBLICATIONS/iag/hivpositive.pdf. >.
- TR Frieden, M Das-Douglas, SE Kellerman, KJ Henning. Applying public health principles to the HIV epidemic. New England Journal Medicine; 353(22), 2005:2397-2402.
- Voluntary HIV-1 Counseling and Testing Efficacy Study Group. Efficacy of voluntary HIV-1 counselling and testing in individuals and couples in Kenya, Tanzania, and Trinidad: a randomised trial. Lancet; 356(9224), 2000:103-112.
- LS Weinhardt, MP Carey, BT Johnson. Effects of HIV counselling and testing on sexual risk behaviour: a meta-analytic review of published research 1985–1997. American Journal of Public Health; 891999:1397-1405.
- LS Weinhardt, JA Kelly, MJ Brondino. HIV transmission risk behaviour among men and women living with HIV in four cities in the United States. Journal of Acquired Immune Deficiency Syndrome; 362004:1057-1066.
- BT Johnson, MP Carey, SR Chaudoir. Sexual risk reduction for persons living with HIV; research synthesis of randomized controlled trials, 1993–2004. Journal of Acquired Immune Deficiency Syndrome; 412006:642-649.
- DL Roth, KE Stewart, OJ Clay. Sexual practices of HIV discordant and concordant couples in Rwanda: effects of a testing and counselling programme for men. International Journal STD & AIDS; 12(3), 2001:181-188.
- S Allen, J Meinzen-Derr, M Kautzman. Sexual behaviour of HIV discordant couples after HIV counselling and testing. AIDS; 172003:733-740.
- N Santos, E Ventura-Filipe, V Paiva. HIV positive women, reproduction and sexuality in São Paulo, Brazil. Reproductive Health Matters; 6(12), 1998:31-40.
- UNAIDS, Intensifying HIV Prevention. UNAIDS Policy Position PaperAugust 2005, UNAIDS. Geneva.
- A Castro, P Farmer. Understanding and addressing AIDS-related stigma: from anthropological theory to clinical practice in Haiti. American Journal of Public Health; 952005:53-59.
- NC Levy, RA Miksad, OT Fein. From treatment to prevention: the interplay between HIV/AIDS treatment availability and HIV/AIDS prevention programming in Khayelitsha, South Africa. Journal of Urban Health; 82(3), 2005:498-509.
- R Feldman, J Manchester, C Maposhere Positive Women: Voices and Choices: A Zimbabwe Report. 2002, SAfAIDS. Harare.
- AD Bouhnik, M Preau, MA Schilts and The VESPA Study Group Unprotected sex in regular partnerships among homosexual men living with HIV: a comparison between sero-nonconcordant and seroconcordant couples (ANRS-EN12-VESPA Study). AIDS; 21(Suppl.1), 2007:S43-S48.
- UNAIDS/WHO, Opening Up the HIV/AIDS Epidemic. Guidance on encouraging beneficial disclosure, ethical partner counselling and appropriate use of HIV case-reporting. UNAIDS Best Practice CollectionNovember 2000, UNAIDS/WHO. Geneva.
- General Medical Council UK. Serious Communicable Diseases 1997. At: <www.gmc-uk.org/guidance. >.
- European Collaborative Study. The mother-to-child HIV transmission epidemic in Europe: evolving in the East and established in the West. AIDS; 202006:1419-1427.
- UNAIDS, WHO, AIDS Epidemic UpdateDecember 2005, UNAIDS. Geneva.
- S Ray, A Latif, R Machekano. Sexual behaviour and risk assessment of HIV seroconvertors among urban male factory workers in Zimbabwe. Social Science and Medicine; 47(10), 1998:1431-1443.
- EJ Bernard. BHIVA: Recent gay seroconverters explain why they became HIV-infected. Aidsmap News. 6 April 2006. At: <www.aidsmap.com. >.
- TC Quinn, MJ Wawer, N Sewankambo. Viral load and heterosexual transmission of human immunodeficiency virus type 1. New England Journal of Medicine; 342(13), 2000:921-929.
- RB Jones, JN Wasserheit. Introduction to the biology and natural history of sexually transmitted diseases JN Wasserheit. Research Issues in Human Behaviour and Sexually Transmitted Diseases in the AIDS Era1991, American Society for Microbiology. Washington DC.
- J Berger. Resexualizing the epidemic: desire, risk and HIV prevention. Development Update; 5(3), 2004 At: <www.sarpn.org.za/documents/d0001195/2-Resexualising the Epidemic-Jonathan_Berger.pdf. >.
- S Kippax, S Slavin, J Ellard. Seroconversion in context. AIDS Care; 15(6), 2003:839-852.
- S Ray, J van de Wijgert, P Mason. Constraints faced by sex workers in use of female and male condoms for safer sex in urban Zimbabwe. Journal of Urban Health: Bulletin of the New York Academy of Medicine; 78(4), 2002:581-592.
- CS Estcourt, C Marks, R Rohrsheim. HIV, sexually transmitted infections, and risk behaviours in male commercial sex workers in Sydney. Sexually Transmitted Infections; 76(4), 2000:294-298.
- S Jolly. Vulnerability, risk and sexual rights. Think piece for ‘AIDS and Vulnerability’ brainstorming workshop. UNAIDS/IDS, 23–24 June 2005. At: <www.eldis.org/cf/rdr/rdr.cfm?doc=DOC20. >.
- J Castilla, J del Romero, V Hernando. Effectiveness of highly active antiretroviral therapy in reducing heterosexual transmission of HIV. Journal of Acquired Immune Deficiency Syndrome; 402005:96-101.
- RH Gray, X Li, MJ Wawer. Stochastic simulation of the impact of antiretroviral therapy and HIV vaccines on HIV transmission, Rakai, Uganda. AIDS; 172003:1941-1951.
- J Richters, S Knox, J Crawford. Condom use and ‘withdrawal’: exploring gay men's practice of anal intercourse. International Journal of STD & AIDS; 11(2), 2000:96-104.
- Oral sex. Aidsmap. 21 December 2005. At: <http://www.aidsmap.com/en/docs/C858FF44-5E81-4F59-8030-B5A3C7A93654.asp. >.
- J del Romero, B Marincovich, J Castilla. Evaluating the risk of HIV transmission through unprotected orogenital sex. AIDS; 16(9), 2002:1269-1297.
- Fellatio. Aidsmap. 13 July 2004. At: <http://www.aidsmap.com/en/docs/D2C102B1-1CE1-4243-93E1-BA0DFEF60440.asp. >.
- TR Moench, T Chipato, NS Padian. Preventing disease by protecting the cervix: the unexplored promise of internal vaginal barrier devices. AIDS; 52001:1595-1602.
- AM Minnis, NS Padian. Effectiveness of female controlled barrier methods in preventing sexually transmitted infections and HIV: current evidence and future research directions. Sexually Transmitted Infections; 82005:193-200.
- University of California, San Francisco. Clinical Trial: Effectiveness of the Diaphragm for HIV Prevention. At: <www.clinicaltrials.gov/ct/show/NCT00121459. >.
- DT Halperin. Heterosexual anal intercourse: prevalence, cultural factors, and HIV infection and other health risks, Part I. Review. AIDS Patient Care and STDS; 13(12), 1999:717-730.
- SS Karim, G Ramjee. Anal sex and HIV transmission in women. American Journal of Public Health; 88(8), 1998:1265-1266.
- American Foundation for AIDS Research. HIV prevention for men who have sex with men. Issue Brief. June 2006. At: <www.amfar.org/cgi-bin/iowa/programs/publicp/record.html?record=37. >.
- Training manual for men who have sex with men. 2001, NAZ Foundation India Trust. New Delhi.
- A Philpott, W Knerr, V Boydell. Pleasure and prevention: when good sex is safer sex. Reproductive Health Matters; 14(28), 2006:23-31.
- RJ Levin. Wet and dry sex – the impact of cultural influence in modifying vaginal function. Sexual and Relationship Therapy; 20(4), 2005.
- RC Bailey, S Moses, CB Parker. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomized controlled trial. Lancet; 3692007:643-656.
- RH Gray, G Kigozi, D Serwadda. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomized trial. Lancet; 3692005:657-666.
- B Auvert, D Talijaard, E Lagarde. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. PLoS Med; 22005:e298.
- Rakai Health Sciences Program. Study presents new information on male circumcision to prevent spread of HIV in Africa. Press release 6 March 2007..
- New Data on Male Circumcision and HIV Prevention: Policy and Programme Implications. WHO/UNAIDS Technical Consultation Male Circumcision and HIV Prevention: Research Implications for Policy and Programming. Montreux, 6–8 March 2007. Conclusions and Recommendations. At: <http://www.who.int/hiv/mediacentre/MCrecommendations_en.pdf. >. Accessed 27 April 2007.
- UNAIDS, WHO, UNFPA, Position Statement on Condoms and HIV PreventionJuly 2004, WHO. Geneva. At: <http://data.unaids.org/una-docs/condom-policy_jul04_en.pdf. >.
- J Cleland, MM Ali, I Shah. Trends in behaviour among single vs. married young women in sub-Saharan Africa: the big picture. Reproductive Health Matters; 14(28), 2006:7-22.
- M Carter. Condoms reduce women's risk of contracting genital HPV, proves US study. Aidsmap News. 22 June 2006. At: <www.aidsmap.com/en/news. >.
- S Weller, K Davis. Condom effectiveness in reducing heterosexual HIV transmission. Cochrane Database Systematic Review; 22004:CD003255.
- KK Holmes, R Levine, M Weaver. Effectiveness of condoms in preventing sexually transmitted infections. Review. Bulletin of World Health Organization; 82(6), 2004:454-461.
- MJ Steiner, W Cates. Condoms and sexually-transmitted infections. New England Journal of Medicine; 3542006:2642-2643.
- American Foundation for AIDS Research. The effectiveness of condoms in preventing HIV transmission. Issue Brief No.1. January 2005. At: <www.amfar.org/binary-data/AMFAR_PUBLICATION/download_file/34.pdf. >.
- World Health Organization Department of Reproductive Health and Research, The Female Condom FC2. Joint WHO/UNAIDS/UNFPA Statement. 2005.
- RL Winer, JP Hughes, Q Feng. Condom use and the risk of genital human papillomavirus infection in young women. New England Journal of Medicine; 3542006:2645-2654.
- JL Gerberding Report to Congress. Prevention of Genital Human Papillomavirus InfectionJanuary 2004, US Centers for Disease Control and Prevention. Atlanta.
- The Pleasure Project. Global Mapping of Pleasure-Focused Projects. 2005. At: <www.thepleasure-project.org. >.
- The FC2 female condom. At: <www.femalehealth.com. >.
- PS Coffey, M Kilbourne-Brook, G Austin. Short-term acceptability of the PATH Woman's Condom among couples at three sites. Contraception; 732006:588-593.
- Female condom use by men Positively Aware; 9(5), 1998:23.
- J Richters, J Gerofi, B Donovan. Why do condoms break or slip off in use? An exploratory study. International Journal of STD & AIDS; 61995:11-18.
- I Heard, V Potard, D Costagliola. Contraceptive use in HIV positive women. Journal of Acquired Immune Deficiency Syndrome; 36(2), 2004:714-720.
- L Panozzo, M Battegay, A Friedl. High risk behaviour and fertility desires among heterosexual HIV-positive patients with a serodiscordant partner – two challenging issues. Swiss Medical Weekly; 133(7–8), 2003:124-127.
- K Buchacz, A van der Straten, J Saul. Sociodemographic, behavioral, and clinical correlates of inconsistent condom use in HIV-serodiscordant heterosexual couples. Journal of Acquired Immune Deficiency Syndrome; 28(3), 2001:289-297.
- JH Humphrey, JW Hargrove, LC Malaba ZVITAMBO Study Group HIV incidence among post-partum women in Zimbabwe: risk factors and the effect of vitamin A supplementation. AIDS; 20(10), 2006:1437-1446.
- P Van de Perre, A Simonson, P Msellati. Postnatal transmission of human immunodeficiency virus type 1 from mother to infant. New England Journal of Medicine; 325(9), 1991:593-644.
- AD Bouhnik, M Preau, MA Schiltz. Unprotected sex in regular partnerships among homosexual men living with HIV: a comparison between sero-nonconcordant and seroconcordant couples (ANRS-EN12-VESPA Study). AIDS; 21(Suppl.1), 2007:S43-S48.
- World Health Organization, Chronic HIV care with ARV therapy, integrated management of adolescent and adult illness, interim guidelines for first-level facility health workersJanuary 2004, WHO. Geneva.
- DM Smith, DD Richman, SJ Little. HIV superinfection. Journal of Infectious Diseases; 1922005:438-444.
- N Cheonis. Dual HIV infection. TheBody.com Winter 2005–06. At: <www.thebody.com/sfaf/winter06/dual.html. >. Accessed 7 March 2007.
- J Overbaugh. HIV transmission and pathogenesis: a viral perspective. Presentation Monday Plenary 01. International AIDS Conference. Toronto, 14 August 2006. At: <www.aids2006.org/Web/MOPL01.ppt. >.
- GS Gottlieb, DC Nickle, MA Jensen. Dual HIV-1 infection associated with rapid disease progression. Lancet; 363(9409), 2004:619-622.
- SC Kalichman, D Rompa. HIV treatment adherence and unprotected sex practices in people receiving antiretroviral therapy. Sexually Transmitted Infections; 792003:59-61.
- TE Wilson, H Minkoff. Condom use consistency associated with beliefs regarding HIV disease transmission among women receiving HIV antiretroviral therapy. Journal of Acquired Immune Deficiency Syndrome; 272001:289-291.
- N Crepaz, TA Hart, G Marks. Highly active antiretroviral therapy and sexual risk behaviour: a meta-analytic review. JAMA; 292(2), 2004:224-236.
- C Diamond, JL Richardson, J Milam. Use of and adherence to antiretroviral therapy is associated with decreased sexual risk behaviour in HIV clinic patients. Journal of Acquired Immune Deficiency Syndrome; 39(2), 2005:211-218.
- JM Stephenson, J Imrie, MM Davis. Is use of antiretroviral therapy among homosexual men associated with increased risk of transmission of HIV infection?. Sexually Transmitted Infections; 79(1), 2003:7-10.
- R Bunnell, JP Ekwaru, P Solberg. Changes in sexual behaviour and risk of HIV transmission after antiretroviral therapy and prevention interventions in rural Uganda. AIDS; 202006:85-92.
- RJ Hayes, KF Schulz, FA Plummer. The cofactor effect of genital ulcers on the per-exposure risk of HIV transmission in sub-Saharan Africa. Journal of Tropical Medicine & Hygiene; 98(1), 1995:1-8.
- World Health Organization, Global prevalence and incidence of selected curable sexually transmitted infections: overview and estimates. 2001, WHO. Geneva.
- DT Fleming, JN Wasserheit. From epidemiological synergy to public health policy and practice: the contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sexually Transmitted Infections; 75(1), 1999:3-17.
- W Rojanapithayakorn. The 100% Condom Use Programme in Asia. Reproductive Health Matters; 14(28), 2006:41-52.
- DD Celentano, KE Nelson, CM Lyles. Decreasing incidence of HIV and sexually transmitted diseases in young Thai men: evidence for success of the HIV/AIDS control and prevention programme. AIDS; 12(5), 1998:F29-F36.
- Leng HB, Wantha SS, Saidel T. Success of Cambodian HIV prevention efforts confirmed by low prevalence of sexually transmitted infections and declining HIV and risk behaviours. In: Proceedings of the Abstracts of XIV International Conference on AIDS, Barcelona, Spain, 6–10 July 2002..
- N Meda, I Ndoye, S M'Boup. Low and stable HIV infection rates in Senegal: natural course of the epidemic or evidence for success of prevention?. AIDS; 131999:1397-1405.
- Moses S, Ngugi EN, Costigan A, et al. Declining sexually transmitted disease and HIV prevalences among antenatal and family planning clinic attenders in Nairobi, Kenya, from 1992–1999. Abstract ThOrC727. XIII International Conference on AIDS, Durban, 9–15 July 2000..
- HPTN 039: A Phase III, randomized, double-blind, placebo-controlled trial of acyclovir for the reduction of HIV acquisition among high risk HSV-2 seropositive, HIV-seronegative individuals. At: <www.hptn.org/research_studies/hptn039.asp. >. Accessed 7 July 2006.
- RC Brunham, FA Plummer. A general model of sexually transmitted disease epidemiology and its implications for control. Medical Clinics of North America; 74(6), 1990:1339-1352.
- M Over, P Piot. HIV infection and sexually transmitted diseases Disease Control Priorities in Developing Countries. 1993, Oxford University Press. New York.
- R Steen, G Dallabetta. The use of epidemiologic mass treatment and syndrome management for sexually transmitted disease control. Sexually Transmitted Diseases; 26(4 Supp.1), 1999:S12-S22.
- M Laga, M Alary, N Nzila. Condom promotion, sexually transmitted diseases treatment, and declining incidence of HIV-1 infection in female Zairian sex workers. Lancet; 3441994:246-248.
- PD Ghys, MO Diallo, V Ettiegne-Traore. Effect of interventions to control sexually transmitted disease on the incidence of HIV infection in female sex workers. AIDS; 15(11), 2001:1421-1431.
- M Alary, L Mukenge-Tshibaka, F Bernier. Decline in the prevalence of HIV and sexually transmitted diseases among female sex workers in Cotonou, Benin, 1993–1999. AIDS; 16(3), 2002:463-470.
- R Steen, B Vuylsteke, T DeCoito. Evidence of declining STD prevalence in a South African mining community following core-group intervention. Sexually Transmitted Diseases; 27(1), 2000:1-8.
- WC Levine, R Revollo, V Kaune. Decline in sexually transmitted disease prevalence in female Bolivian sex workers: impact of an HIV prevention project. AIDS; 12(14), 1998:1899-1906.
- T Wi, E Ramos, R Steen. STI declines among sex workers and clients following outreach, one-time presumptive treatment and regular screening of sex workers in the Philippines. Sexually Transmitted Infections; 82(5), 2006:386-391.
- S Jana, N Bandyopadhyay, A Saha. Creating an enabling environment: lessons learnt from the Sonagachi Project, India Research for Sex Work 2. 1999 At: <hcc.med.vu.nl/artikelen/jana.htm. >. Accessed 23 March 2007.
- JR Williams, AM Foss, P Vickerman. What is the achievable effectiveness of the India AIDS Initiative intervention among female sex workers under target coverage? Model projections from southern India. Sexually Transmitted Infections; 822006:372-380.
- R Steen, V Mogasale, T Wi. Pursuing scale and quality in STI interventions with sex workers: initial results from Avahan India AIDS Initiative. Journal of Sexually Transmitted Infections; 82(5), 2006:381-385.
- R Steen, S Ralepeli, T DeCoito. Lesedi: services for women at high risk help reduce sexually transmitted infection (STI) prevalence in a South African mining community. FHI/UNAIDS Best Practices in HIV/AIDS Prevention Collection Case Study Four. 2007 At: <www.fhi.org/en/HIVAIDS/pub/guide/bestpractices.htm. >. Accessed 20 March 2007.
- S Aral. Heterosexual TRansmission of HIV: the role of other sexually transmitted infections and behavior in its epidemiology prevention and control. Annual Review of Public Health; 141993:451-467.
- MS Cohen. HIV and sexually transmitted diseases: lethal synergy. Topics in HIV Medicine; 122004:104-107.
- WHO, UNFPA, Sexual and Reproductive Health of Women with HIV. Guidelines on care, treatment and support for women living with HIV/AIDS and their children in resource-constrained settings. 2006, WHO. Geneva.
- WHO Guidelines for the Management of Sexually Transmitted InfectionsRevised edition2003, WHO. Geneva. At: <www.who.int/reproductive-health/publications/rhr_01_10_mngt_stis/index.html. >.
- D Mabey, RW Peeling, A Ustianowski. Diagnostics for the developing world. Nature Reviews Microbiology; 2(3), 2004:231-240.
- CD Pilcher, MA Price, IF Hoffman. Frequent detection of acute primary HIV infection in men in Malawi. AIDS; 182004:517-524.
- World Health Organization International Agency for Research on Cancer, IARC Handbooks of Cancer Prevention. Vol.10: Cervix Cancer Screening. 2005, IARC Press. Lyon.
- Kreuter A, Reimann G, Esser S, et al. [Screening and therapy of anal intraepithelial neoplasia (AIN) and anal carcinoma in patients with HIV-infection]. Deutsche Medizinische Wochenschrift 2003;128:38,1957–62..
- MS Bleeker, CJ Hogewoning, FJ Voorhorst. Condom use promotes regression of human papillavirus-associated penile lesions in male sex partners of women with cervical intraepithelial neoplasia. International Journal of Cancer; 107(5), 2003:804-810.
- CJ Hogewoning, MS Bleeker, AJ Vanden Brule. Condom use promotes regression of cervical intraepithelial neoplasia and clearance of human papillomavirus: a randomised clinical trial. International Journal of Cancer; 107(5), 2003:811-816.
- CM Lowndes, ON Gill. Cervical cancer, human papillomavirus, and vaccination. BMJ; 331(7522), 2005:915-916.
- DM Harper, EL Franco, C Wheeler. Efficacy of a bivalent L1 virus-like particle vaccine in prevention of infection with human papillomavirus types 16 and 18 in young women: a randomised controlled trial. Lancet; 364(9447), 2004:1757-1765.
- LA Koutsky, KA Ault, CM Wheeler. A controlled trial of a human papillomavirus type 16 vaccine. New England Journal of Medicine; 347(21), 2002:1645-1651.
- M Carter. HIV-positive women often infected with multiple high-risk HPV strains not covered by vaccine. Aidsmap News27 July 2006 At: <www.aidsmap.com/en/news/A8AD650BD88D-42CC-AE47-DE40BBC6E48F.asp. >.
- TV Ellerbrock, MA Chiasson, TJ Bush. Incidence of cervical squamous intraepithelial lesions in HIV-infected women. Journal of American Medical Association; 283(8), 2000:1031-1037.
- XW Sun, TV Ellerbrock, O Lungu. Human papillomavirus infection in human immunodeficiency virus-seropositive women. Obstetrics & Gynaecology; 851995:680-686.
- TJ Wright, S Subbarao, TV Ellerbrock. Human immunodeficiency virus 1 expression in the female genital tract in association with cervical inflammation and ulceration. American Journal of Obstetrics & Gynecology; 184(3), 2001:279-285.
- J Melnikow, J Nuovo, AR Willan. Natural history of cervical squamous intraepithelial lesions: a meta-analysis. Obstetrics & Gynecology; 92(4 Part 2), 1998:727-735.
- AG Ostor. Natural history of cervical intraepithelial neoplasia: a critical review. International Journal of Gynaecological Pathology; 12(2), 1993:186-192.
- P Lomalisa, T Smith, F Guidozzi. Human immunodeficiency virus infection and invasive cervical cancer in South Africa. Gynecologic Oncology; 77(3), 2000:460-463.
- ZM Chirenje. HIV and cancer of the cervix. Best Practice & Research. Review. Clinical Obstetrics & Gynaecology; 19(2), 2005:269-276.
- M Bower, D Mazhar, J Stebbing. Should cervical cancer be an acquired immunodeficiency syndrome-defining cancer?. Journal of Clinical Oncology; 24(16), 2006:2417-2419.
- EM van der Snoek, ME van der Ende, WR Schouten. [Anorectal malignancies and dysplasia in HIV-positive men who have sex with men]. Nederlands Tijdschrift voor Geneeskunde; 149(36), 2005:1989-1993.
- WHO, Comprehensive Cervical Cancer Control: A Guide to Essential Practice. 2006, WHO. Geneva.
- I Heard, JM Palefsky, MD Kazatchkine. The impact of HIV antiviral therapy on human papillomavirus (HPV) infections and HPV-related diseases. Antiviral Therapy; 9(1), 2004:13-22.
- International Collaboration on HIV and Cancer. Highly active antiretroviral therapy and incidence of cancer in human immunodeficiency virus-infected adults. Journal of National Cancer Institute; 922000:1823-1830.
- M Frisch, RJ Biggar, JJ Goedert. Human papillomavirus-associated cancers in patients with human immunodeficiency virus infection and acquired immunodeficiency syndrome. Journal of National Cancer Institute; 922000:1500-1510.
- EA Engels, JJ Goedert. Human immunodeficiency virus/acquired immunodeficiency syndrome and cancer: past, present, and future. Journal of National Cancer Institute; 97(6), 2005:407-409.
- I Heard, JM Tassie, MD Kazatchkine. Highly active antiretroviral therapy enhances regression of cervical intraepithelial neoplasia in HIV-seropositive women. AIDS; 16(13), 2002:1799-1802.
- H Minkoff, L Ahdieh, LS Massad. The effect of highly active antiretroviral therapy on cervical cytologic changes associated with oncogenic HPV among HIV-infected women. AIDS; 15(16), 2001:2157-2164.
- I Heard, JM Tassie, V Schmitz. Increased risk of cervical disease among human immunodeficiency virus-infected women with severe immunosuppression and high human papillomavirus load (1). Obstetrics & Gynaecology; 96(3), 2000:403-409.
- JK Kreiss, NB Kiviat, FA Plummer. Human immunodeficiency virus, human papillomavirus, and cervical intraepithelial neoplasia in Nairobi prostitutes. Sexually Transmitted Diseases; 19(1), 1992:54-59.
- C Piketty, MD Kazatchkine. Human papillomavirus-related cervical and anal disease in HIV-infected individuals in the era of highly active antiretroviral therapy. Current HIV/AIDS Reports; 32005:140-145.
- K Shapiro, K West, L Heise Standard of care in international phase III microbicide efficacy trials. Draft report for Global Campaign for MicrobicidesMarch 2007 (Unpublished).
- S Hawkes, M Collumbien. The sexual health of men in India and Bangladesh; what are men's concerns? Programming for male involvement in reproductive health Report of the meeting of WHO Regional Advisers in Reproductive HealthSeptember 2001, PAHO. Washington DC. At: <whqlibdoc.who.int/hq/2002/WHO_FCH_RHR_02.3.pdf. >.
- MP Trotta, A Ammassari, A Cozzi-Lepri. Adherence to highly active antiretroviral therapy is better in patients receiving non-nucleoside reverse transcriptase inhibitor-containing regimens than in those receiving protease inhibitor-containing regimens. AIDS; 172003:1099-1102.
- MJ Miguez-Burbano, L Espinoza, JE Lewis. HIV treatment adherence and sexual functioning. AIDS and Behaviour2007 Feb 13 [E-pub ahead of print].
- D Richardson, H Lamba, D Goldmeier. Factors associated with sexual dysfunction in men with HIV infection. International Journal of STD & AIDS; 17(11), 2006:764-767.
- C Bell, D Richardson, M Wall. HIV-associated female sexual dysfunction: clinical experience and literature review. International Journal of STD & AIDS; 17(10), 2006:706-709.
- M Collumbien, S Hawkes. Missing men's messages: does the reproductive health approach respond to men's sexual health needs?. Culture, Health and Sexuality; 22000:135-150.
- AVSC International International Planned Parenthood Federation Western Hemisphere Region, Literature review for the symposium on male participation in sexual and reproductive health: new paradigms. 1999, IPPF WHR. New York.
- I Szasz. Masculine identity and the meanings of sexuality: a review of research in Mexico. Reproductive Health Matters; 6(12), 1998:97-104.
- E Weiss, G Rao Gupta Bridging the Gap: Addressing Gender and Sexuality in HIV Prevention. 1998, International Centre for Research on Women. Washington DC.
- Action Research in Community Health and Development. Perceptions of male members about reproductive health matters: preliminary evidence from a tribal area of Gujarat Men as Supportive Partners in Reproductive Health. Moving from Rhetoric to Reality. 2000, Population Council. New York.
- S Ray, N Gumbo, M Mbizvo. Local voices: what some Harare men say about preparation for sex. Reproductive Health Matters; 4(7), 1996:34-45.
- B Robey, M Drennan. Male participation in reproductive health. Network; 18(3), 1998:11-15.
- YA Amirkhanian, JA Kelly, E Kabakchieva. A randomized social network HIV prevention trial with young men who have sex with men in Russia and Bulgaria. AIDS; 19(16), 2005:1897-1905.
- Prevention and control of sexually transmitted infections: draft global strategy. World Health Organization, 59th World Health Assembly, Provisional agenda item 11.618 May 2006 At: <www.who.int/gb/ebwha/pdf_files/WHA59/A59_11-en.pdf. >.
- Leading advocates express support for microbicide research, despite disappointing clinical trial results Global Campaign for Microbicides/African Microbicides Advocacy Group/AIDS Vaccine Advocacy Coalition Joint Statement31 January 2007 At: <www.global-campaign.org/clientfiles/civil_soc_press_release%209.doc. >.
- TAC comment on the termination of Ushercell microbicide trial Treatment Action Campaign Electronic Newsletter7 February 2007 At: <www.tac.org.za/nl20070207.html. >.
- HIV positive women and microbicides Global Campaign for MicrobicidesApril 2006 At: <www.global-campaign.org/clientfiles/FS7-PositiveWomen-March07.pdf. >.