The Safe Motherhood Initiative was launched in 1987, so this year sees in its 20th anniversary. Global campaigns to mobilise resources and turn attention to the burden of death and illness faced by women during pregnancy, especially in developing countries, have been repeatedly renewed over the last two decades. Some of the most recent calls for action include the launch of the Lancet Maternal Survival seriesCitation1 and the Women Deliver conference in October 2007.Citation2 There are only eight years to go before 2015, a landmark date for the Millennium Development Goals, one of which is a reduction of 75% in maternal mortality from current levels. The hard facts available to us do not show cause for optimism in reaching this target. There is no evidence of reduction in maternal mortality globally; indeed, mortality in some countries like Malawi has increased.Citation3 In rural sub-Saharan Africa, delivery care with health professionals has stagnated at 30%, while small improvements from 40% to 50% between 1992 and 2000 were found in 40 collated national surveys.Citation4 Even in settings with some improvements in coverage, quality, appropriateness and effectiveness of the care being provided remains a concern.
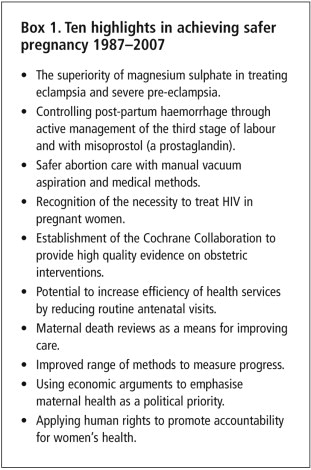
Is it naïve to suggest that there is anything to celebrate in progress toward safer pregnancy? Have the efforts and investments in maternal health in the last 20 years been totally wasted? Perhaps we should not be too pessimistic. After all, an anniversary is a time for reflection – to acknowledge the needs, failures and mistakes – but also to celebrate achievements. So, in salutation, here, in no particular order, are some major advances in the last two decades of the safe motherhood initiative (Box 1).
Conclusive evidence is available of the superiority of magnesium sulphate over other anticonvulsant drugs in treating eclampsia and pre-eclampsia.Citation5 We now know that magnesium sulphate should be used in first and in recurrent eclamptic seizures and in pre-eclampsia when there is a risk of eclampsia occurring. This evidence changed practice especially quickly in Britain where magnesium sulphate was not previously used. Despite advice that magnesium sulphate can be safely administered by trained medical, midwifery or nursing personnel, the drug has so far not been as widely adopted in developing countries where the incidence of eclampsia is highest.
Post-partum haemorrhage, diagnosed as when blood loss is 500ml or more, is one of the commonest causes of maternal death. Active management of the third stage of labour, when used routinely in third stage management of vaginal deliveries, effectively reduces blood loss and controls post-partum haemorrhage.Citation6 Routine active management is an established protocol, but erratically practiced in many developing country settings. Recently, misoprostol (a prostaglandin), which can be administered orally or sub-lingually, has gained recognition for use when injectable uterotonics are not available.Citation7 Its utility in controlling haemorrhage in situations with limited access to professional health care is not yet widely accepted.
Safe abortion care has benefited from the development of new techniques.Citation8 Vacuum aspiration is now recognised as a safe and effective surgical method for abortion and its complications up to 15 weeks of pregnancy. Efforts to boost its use in developing countries are increasing. Medical abortion using mifepristone in combination with misoprostol has also revolutionised the safety of first trimester abortions.
HIV is a major cause of maternal mortality in high prevalence areas. Recognition of this situation has led to development of better antiretroviral drug regimes for treating pregnant women with HIV – both for the woman’s own health as well as to prevent transmission of HIV to the child.Citation9 Good research evidence is available on treatment regimes but uptake of evidence is still lacking in many developing countries.
The Cochrane Collaboration has been a breakthrough for safe motherhood and health care in its own right.Citation10 The initiative has played a central role in improving clinical knowledge, some examples of which are discussed above. Given current views that safe motherhood initiatives are the “poor cousin” of successful global programmes like childhood immunisation, it is worth noting that quality data on pregnancy care from well-conducted studies was one of the foundations upon which the Collaboration was built, changing the image of obstetrics as “the least scientific medical speciality” in the 1980s and 1990s.
The knowledge that the number of routine antenatal visits can be reduced without jeopardising maternal safety provides an avenue toward more efficient health service provision.Citation11 The paradox of this evidence is that despite continuing increase in the uptake of antenatal care worldwide, concerns regarding quality, late pregnancy booking and single contact remain, especially for the most disadvantaged women. The HIV pandemic has further emphasised the need for access to antenatal care by pregnant women.
Maternal death reviews and confidential enquiries have been used for over half a century in some countries, but safe motherhood efforts have enabled implementation in many developing countries.Citation12 Nevertheless, the quality of the review process and the extent of learning that leads to changes in practice require further improvement.
Today, there are more and better methods to measure reduction of maternal mortality available. More than 40 tools for assessing, monitoring and measuring maternal health are currently listed in the Compendium of Maternal and Newborn Health Tools.Citation13 Although not an advance that saves lives directly, progress would be difficult to demonstrate without improvements in methods of measurement. Despite the availability of these tools, capacity-building for measurement and monitoring globally is still required.
Using economic reasoning is a relatively new approach to increasing global attention to and investment in safe motherhood. Demonstrating the link between maternal ill-health and poverty is a powerful political tool which speaks to the priorities of sectors beyond health. This movement has led to the generation of improved knowledge on the effects of maternal death on poverty and development.Citation14
Applying human rights as a basis to argue the case for women’s health is an approach taken up by a number of global organisations.Citation15 Used in a supportive way, rights-based principles can provide an environment within which governments and civil society can influence policies to reduce gender and social inequities which add momentum to other means of reducing maternal mortality.
The successes listed are a mix of two sorts – one is evidence of life-saving interventions and the other, strategic approaches pertinent to public health and political concerns. We need progress in both these areas. There is a strong argument for celebrating and communicating these advances. Even if it is clear that there is no case for resting on our laurels, it would seem undermining to disregard or underplay the determined efforts of so many people in the last 20 years. If we do not acknowledge that there have been at least some steps forward, then we run the risk of losing potential future support by conveying only our failures. We also risk the ability to attract a new generation of scientists, advocates, practitioners and investors into an area of public health which will otherwise become known only for its disappointments.
For the future, there is much to do. We need to focus on seeking evidence that is directly relevant to policy and practice. It is not enough to generate good evidence without ensuring optimal access for all pregnant women. The evidence must tell us not only what is happening, but why, and how more progress can be made.
As the safe motherhood initiative approaches its “coming of age” at 20, these are my choices for ten achievements in safe motherhood – what are yours?
Acknowledgements
The author’s work is part of an international research programme, Immpact (see <www.immpact-international.org>) which is funded by the Bill & Melinda Gates Foundation, the UK Department for International Development and USAID. The funders have no responsibility for the information provided or views expressed in this paper. The views expressed herein are solely those of the author.
References
- R Horton. Healthy motherhood: an urgent call to action. Lancet. 368(9542): 2006; 1129.
- Women Deliver Conference London 18–20 October 2007. At: <www.womendeliver.org>. Accessed 14 June 2007
- World Health Organization. World Health Report 2005: Make Every Mother and Child Count. 2005; WHO: Geneva.
- M Koblinsky, Z Matthews, J Hussein. Going to scale with professional skilled care. Lancet. 368(9544): 2006; 1377–1386.
- Magpie Trial Collaborative Group. Do women with pre-eclampsia, and their babies, benefit from magnesium sulphate? The Magpie Trial: a randomised placebo-controlled trial. Lancet. 359(9321): 2002; 1877–1890.
- Prendiville WJ, Elbourne D, McDonald S. Active versus expectant management in the third stage of labour. Cochrane Database of Systematic Reviews 2000; Issue 3. Art. No. CD000007.
- Gülmezoglu AM, Forna F, Villar J, et al. Prostaglandins for preventing postpartum haemorrhage. Cochrane Database of Systematic Reviews 2007; Issue 3. Art. No. CD000494.pub3.
- K Rogo. Improving technologies to reduce abortion-related morbidity and mortality. International Journal of Gynecology and Obstetrics. 85(S1): 2005; S73–S82.
- J McIntyre. Preventing mother to child transmission of HIV: successes and challenges. BJOG: An International Journal of Obstetrics and Gynaecology. 112: 2005; 1196–1203.
- Cochrane Collaboration. At: <www.cochrane.org>. Accessed 15 June 2007
- G Carroli, J Villar, G Piaggio. WHO systematic review of randomised controlled trials of routine antenatal care. Lancet. 357(9268): 2001; 1546.
- World Health Organization. Beyond the Numbers: Reviewing maternal deaths and complications to make pregnancy safer. 2004; WHO: Geneva. At: <www.who.int/reproductive-health/publications/btn/text.pdf>. Accessed 27 July 2007
- Compendium of Maternal and Newborn Health Tools. At: <www.cpc.unc.edu/measure/publications/html/ms-02-09.html>. Accessed 27 July 2007
- P Jha, A Mills. Improving health outcomes of the poor: The Report of Working Group 5 of the Commission on Macroeconomics and Health. 2002; World Health Organization: Geneva.
- K Hawkins, K Newman, D Thomas. Developing a human rights-based approach to reducing maternal mortality: Desk review. 2005; DFID Health Resource Centre: London. At: <www.dfid.gov.uk/pubs/files/maternal-desk.pdf>. Accessed 27 July 2007