Abstract
This paper describes the maternity monitoring system in Botswana, developed in 1998, and the main methods used: maternal death and morbidity reviews at service delivery level, analysis by the National Maternal Mortality Audit Committee of data from the reviews as reported on two forms, perinatal reviews and surveys using process indicators. We carried out a study of these findings to examine whether the system was working well. Surveys using process indicators in 2001 and 2006 were analysed. Other data examined were from 2004–2006 and early 2007. The Maternal Death Notification Form was found to be comprehensive but not all health facilities were submitting them and some gave incomplete information. In 2001, 70% of pregnant women attended antenatal care but access to emergency obstetric care was uneven. In 2006, 28 facilities with maternity services surveyed were providing 24-hour delivery care, but laboratory, theatre and blood supplies were more limited, and only 50% of doctors and 67% of midwives had life-saving skills. Antibiotics were widely available, but there were shortages of magnesium sulphate, diazepam, oxytocics and manual vacuum aspiration kits. Recommendations for improvements have been made, training for skilled attendants is ongoing and a medical school has just opened at the University of Botswana.
Résumé
Le Botswana a instauré un système de surveillance de la maternité en 1998. Il utilise les analyses de la mortalité et de la morbidité maternelles au niveau de la prestation des services, l’étude par le Comité national de contrôle de la mortalité maternelle des données des analyses, telles que notifiées dans deux formulaires, les enquêtes périnatales à l’aide d’indicateurs de processus. On a étudié ces conclusions pour déterminer si le système fonctionne bien et on a analysé des enquêtes utilisant les indicateurs de processus en 2001 et 2006. D’autres données dataient de 2004–2006 et début 2007. Le formulaire de notification des décès maternels est complet, mais n’est pas envoyé par tous les centres de santé et donne parfois des informations fragmentaires. En 2001, 70% des femmes enceintes bénéficiaient de soins prénatals, mais l’accès aux soins obstétricaux d’urgence était inégal. En 2006, 28 maternités visées par l’enquête assuraient des accouchements 24 heures sur 24, mais l’accès aux laboratoires, aux salles d’opération et aux produits sanguins était plus limité, et seulement 50% des médecins et 67% des sages-femmes possédaient des compétences capables de sauver la vie. Les antibiotiques étaient largement disponibles, mais des pénuries de sulfate de magnésium, de diazépam, d’ocytociques et de trousses d’aspiration manuelle se produisaient. Des recommandations ont été formulées pour améliorer les services, la formation des agents qualifiés est en cours et une école de médecine vient d’ouvrir à l’Université du Botswana.
Resumen
En este artículo se describe el sistema de monitoreo de maternidad en Botsuana, creado en 1998, y los principales métodos utilizados: revisiones de morbimortalidad materna en los puntos de entrega de servicios, análisis por el Comité Nacional de Auditoría de Mortalidad Materna de los datos de las revisiones, conforme informados en dos formularios, revisiones y encuestas perinatales utilizando indicadores de proceso. Realizamos un estudio de estos hallazgos para examinar si el sistema funcionaba bien. Se analizaron las encuestas utilizando los indicadores de proceso en 2001 y 2006. Otros datos examinados fueron de 2004–2006 y principios de 2007. Se encontró que el Formulario de Notificación de Muerte Materna era completo, pero no todos los establecimientos de salud lo estaban llenando y algunos daban información incompleta. En 2001, el 70% de las mujeres embarazadas recibieron atención antenatal, pero no todas tenían acceso a los cuidados obstétricos de emergencia. En 2006, se estaba brindando atención a partos las 24 horas, en 28 establecimientos con servicios de maternidad encuestados, pero los suministros de laboratorio, quirófano y sangre estaban más limitados y sólo el 50% de los médicos y el 67% de las parteras contaban con habilidades para salvar vidas. Los antibióticos se conseguían con facilidad, pero había escasez de sulfato de magnesio, diazepán, oxitócicos e instrumental de aspiración manual endouterina. Se han hecho recomendaciones para mejoramientos, se continúa capacitando a parteras calificadas y se acaba de inaugurar la Facultad de Medicina de la Universidad de Botsuana.
Statistics on maternal mortality in Botswana are not considered reliable.Citation1 In the 1990s, figures ranged from 200 per 100,000 live births in hospital records for 1990–92,Citation2 to an estimated 481 in the WHO/UNICEF/UNFPA report of 1995Citation3 and 200–250 in the Global Maternal Mortality Fact Book in 1999.Citation4 More recently, according to routine facility-based records in 2004, the figure ranged from 175 in 2004 to 154 in 2005 and 165 in 2006.Citation5–7 Data on maternal morbidity in Botswana are also limited. A 2004 unpublished government report, using data collected through the confidential Maternal Death Notification Form (MH2000 Review 2006) revealed that of 36,304 deliveries, there were 7,073 women who experienced maternal complications or morbidity.Citation5
According to the Botswana Multiple Indicator Survey for the year 2000, the proportion of women aged 15–49 years attended at least once during pregnancy by skilled personnel (a trained midwife, medical officer, neonatal nurse or obstetrician–gynaecologist) was 97%,Citation8 an increase of 3% over the 1996 figures,Citation1 while the proportion of births attended by a skilled attendant was 95%. The modern contraceptive prevalence rate was 44% in 2000,Citation8 and the 2001 Population and Housing Census reported a total fertility rate of 3.27.Citation9
Botswana is a landlocked, semi-arid country in southern Africa with an estimated population of 1.7 million.Citation9 Just over half the women are of reproductive age. The South Eastern and Eastern regions of the country contain 88% of the population, while the western desert region has a very low population. Most of the hospitals were initially built on the eastern side of the country. Botswana is served by two major road networks, in the southern and northern parts of the country.Citation10 Tarred roads are found in most districts, connecting major villages, which makes transportation and referral of maternity patients more efficient.
Monitoring progress in reducing maternal mortality is vital. This paper describes the maternity monitoring system in Botswana and the main methods used: maternal death and morbidity reviews at facility level, analysis by the National Maternal Mortality Audit Committee of data from the reviews reported on two forms, perinatal reviews and the WHO process indicators. We carried out a study of the evidence from this monitoring system to examine whether the system was working as well as it should and make recommendations for improvements. Data from two analyses of process indicators in 2001 and 2006 were studied. All other data studied were from 2004–2006 and early 2007. Data were also obtained from Botswana’s Safe Motherhood Programme reports and annual National Maternal Mortality Audit Committee reports. In some cases, personal communication with key informants was used to verify data.
Botswana’s health care system
The Government health care system is the responsibility of two ministries. The Ministry of Health, established in 1975, is responsible for the formulation of national health policies, the education and training of all health personnel and the employment of primary, district and referral hospital staff. The Ministry of Local Government is responsible for the management of clinics, health posts and mobile stops. Coordination between the two ministries is ensured through the joint Primary Health Care Coordinating Committee, in operation since 1976.Citation10
There are 24 health districts, based on a primary health care model. Services are decentralised and delivered through several levels of facilities, from mobile stops to health posts and clinics, up to primary, district and large national referral hospitals. The referral system provides increasingly sophisticated services at successive levels. Clinics provide maternity services and are normally staffed by registered nurses and midwives. These include antenatal care, treatment of problems in pregnancy such as anaemia, and normal deliveries. Primary hospitals are staffed by nurse–midwives and medical officers, and provide a wider range of services, including most deliveries. Primary hospitals are supposed to provide basic essential obstetric care but are not equipped for surgery or managing complications of delivery such as obstructed labour. District and referral hospitals are the next levels of health facilities, equipped to carry out caesarean sections and blood transfusion. All hospitals are open 24 hours a day; clinics are open from 7:30am–4:30pm. However, there is always a staff member on call at clinics to attend to emergencies. The security guard at the clinic is responsible for alerting staff on call about the existence of any emergency.
According to National Development Plan 9 (2004–2009), there are 810 mobile stops, 341 health posts, 261 clinics, 14 district hospitals, 17 primary hospitals and 3 national referral hospitals.Citation10 It is government policy that every settlement with a population of 500 or more has a health facility, while all administrative districts have either a primary or district hospital. Sexual and reproductive health services such as antenatal care, delivery and post-natal care, family planning, post-abortion care, infertility services and sexually transmitted infection (STI) services are provided free at all government clinics, clinics with maternity care and hospitals. Where there are no clinics, health workers have to ensure that such services are scheduled and offered through outreach services (mobile stops). In addition to Government health institutions, the country also has two private hospitals, several private clinics and three mining hospitals where maternity services are provided.
All referral, district and primary hospitals as well as clinics in Botswana have telephones. This makes it easy for health practitioners to communicate with each other about issues related to maternity care. Unfortunately, some of the health posts do not have telephones, but have to rely on institutional two-way Radio Call Services, popularly known as roger–roger. Communications between health posts and other health facilities may be hindered as the roger–roger system uses solar power and is dependent on weather conditions. This may adversely affect the speed with which staff from facilities can communicate with Central Medical Store (CMS) personnel for procurement of essential obstetric drugs and equipment.
Maternity monitoring system in Botswana
The Safe Motherhood Conference of 1987 in Nairobi recommended that countries adopt strategies to reduce maternal mortality by at least 50% by the year 2000. The Botswana government accepted these recommendations and launched its national Safe Motherhood Initiative in 1990.Citation11 The current objective of the programme is to reduce the maternal mortality ratio to 150 by 2011. Botswana has also endorsed the Millennium Development Goal of reducing the 1990 maternal mortality ratio by 75% by the year 2015.Citation1 In order to measure the impact of Safe Motherhood programme interventions, a system of continuous evaluation and assessment of progress in relation to maternity care was developed. Thus, a national maternal morbidity and mortality monitoring system, with two main monitoring levels, was developed in 1998. The system is designed to provide an opportunity for all those involved in the health system to participate.Citation11
The two levels are internal (institutional) and external (non-institutional). The internal level involves monitoring committees at health facilities with in-patient maternity care. These are found at clinics with maternity services, primary, district and referral hospitals. The composition of the committee at each level includes representation from the obstetrics and gynaecology team plus the officer in-charge of the facility. The committee meets if and when morbidity and/or a maternal death have occurred within the institution. Staff at each level are required to consider and discuss each case, examine the circumstances leading up to it and make relevant conclusions and recommendations on each individual case.Citation11 All the information obtained from each case is eventually compiled and the report is forwarded to the Ministry of Health Safe Motherhood Programme office. The main objectives of the internal monitoring committees include improvement of services at the facility, provision of information and education to facility staff and the community, improvement of the referral system and provision of in-service training.
The external monitoring system is based at national level. It is composed of obstetrician–gynaecologists from various health regions, midwives and regional senior matrons from the southern and northern parts of Botswana, a general medical officer, representatives from WHO and UNFPA, and the Safe Motherhood Programme Coordinator, who serves as secretary to the committee. This committee is referred to as the National Maternal Mortality Audit Committee, and it meets on quarterly basis. Its primary role is to assist the Ministry of Health to assess all maternal deaths reported at national level and advise the Ministry accordingly. The Committee is also responsible for conducting confidential enquiries and developing a reporting system on maternal deaths. The Committee reviews national obstetric emergency guidelines with a view to improving service delivery. Within the Committee, there are assessors who prepare a summary of each case from the maternal death notification form (MH2000) and the case notes from facilities and then submit the report to the National Maternal Morbidity and Mortality Audit Committee. The Committee then reviews all maternal death summary reports and makes recommendations to the Ministry of Health.
Data collection
At health facility level, the information on maternal morbidity and mortality is collected through the confidential Maternal Death Notification Form (MH2000), developed by government. The form is anonymous in respect of the health personnel involved in the management of the case in question.Citation12 It does include the name of the facility and district where the death occurred. It further captures demographic details of the deceased, including name, summary of antenatal care provided, care during labour, delivery and pueperium as well as neonatal information. The form has a section that asks whether family members contributed to any of the problems encountered by the pregnant woman. It also seeks to find out if there were any logistical or health personnel-related problems that contributed to the morbidity or mortality. The form includes post-mortem results and an assessment as to whether or not the death was avoidable. Ultimately, the form has to bear the signature of the medical officer who compiled the data.
Immediately after a woman dies in a health facility, the head of the facility should notify the Ministry of Health by telephone. The confidential maternal death notification form should be completed in duplicate by either the midwife or the medical officer within seven days of the death and submitted to the Sexual and Reproductive Health Unit, with copies of the antenatal card, case records and all investigation results.
The other form used is a one-page maternal and perinatal monitoring tool (MH3123), filled out by facilities on a monthly basis to summarise and report on the maternity services. The form was developed due to the concern that the maternal death notification form was not being completed adequately and the frequency of reporting to the national level was not regular. In addition, unless a maternal death occurred, vital information on maternal morbidity experienced by women was not being reported as a death has to occur for the MH2000 form to be filled in.Citation5
The maternal and perinatal monitoring form captures the total number of deliveries and categorises them as follows: spontaneous vertex deliveries, caesarean section, breech, vacuum extraction and forceps. The form also captures multiple births, delivery before the arrival of a skilled attendant, live births weighing less than 2.5 kg or equal to/more than 2.5 kg, stillbirths below 1 kg, 1.0–1.5 kg and above 1.5 kg. Congenital abnormalities, conditions such as pre-eclampsia, eclampsia, anaemia, post-partum haemorrhage, obstructed labour, ruptured uterus, sepsis, antepartum haemoorhage, 3rd or 4th degree tear, vesico-vaginal fistula and other complications are also monitored through this form.
Process indicators used to measure progress
Botswana also relies on process indicators for regular programme monitoring.Citation1 The indicators describe the functionality of health services and their capacity to address life-threatening complications during pregnancy and delivery. These indicators include number and distribution of essential obstetric care services, the proportion of deliveries attended by skilled attendants and occurring in institutional settings, the rates of operative delivery and institution or case-fatality rates.Citation1,13,14 Surveys and facility-based assessment studies are used to collect data on process indicators.
Data compilation and analysis
The National Maternal Mortality Audit Committee analyses the data to assess the management of the patient. Written feedback from the Committee is given to staff at the facilities involved via the Research and Evaluation section of the Sexual and Reproductive Health Unit. Feedback is in the form of recommendations on how to handle similar cases in future. For instance, if the analysis reveals that a morbidity or mortality occurred because of shortage of staff, then the Committee recommends additional staff for that facility.
During a recent Committee meeting, there was a case of a woman who died because her blood pressure was too high, and she was managed at a lower level facility which lacked essential drugs. Instead of transferring the woman to a referral hospital as per obstetric guidelines, a medical doctor at the receiving facility communicated with the referral hospital by telephone to ask for the drug, only to learn that the drug was out of stock. The doctor then decided not to refer the woman to a higher facility. The feedback given was that in future, similar cases should be referred on the basis of the written obstetric guidelines, which stipulate that they should be managed at a national referral hospital.
Data on the maternal mortality monitoring system
Notification forms
During regular, scheduled meetings of the National Maternal Mortality Audit Committee and support visits to the districts by national staff, it has been reported that the Confidential Maternal Death Notification Form is comprehensive enough and covers vital information, including the cause(s) of death. However, not all health facilities were submitting forms and some forms were being returned with incomplete information. We were told that staff in health facilities felt that the form was too lengthy and required a lot of time to complete.
Considering that maternal deaths in Botswana occur infrequently, we concluded that the concern expressed was not genuine. However, in 2006, the National Maternal Mortality Audit Committee reduced the form from eight to four pages, retaining sections for all the information considered essential. Copies of the revised form were sent to health facilities for use starting in January 2007.Citation7 The Committee continues to monitor the use of the form.
According to the Assistant Director of Clinical Services (a member of the Committee), maternal death notification by phone within 24 hours is working smoothly. However, the submission of the form within seven days has proved to be problematic. Health facility staff said that seven days was too short for the local monitoring committee to have met. Reasons given for this included the fact that some committee members might be on night shift, off duty or temporarily out of the duty station. This reasoning seemed faulty to us and indicated more of an attitudinal problem since, in a year, a facility might experience a maximum of two deaths.
It was observed that there was no focal person at the facility level responsible for monthly compilation of maternal morbidity and mortality statistics, which means no one can be held accountable for compiling the data.
The feedback from health facility staff on the maternal and perinatal monitoring tool (MH3123) was that it is user-friendly because of its short length. They also felt that it asked for relevant and concise information. In our view, however, although the form asks for concise information, it does not ascertain the rationale for procedures such as caesarean section or vacuum extraction. Nor does it ask for the steps that led to a stillbirth or attribute the stillbirth to either maternal conditions, such as syphilis or diabetes (macerated stillbirth), or to poor birth techniques resulting in avoidable death (fresh stillbirth).
Number and causes of maternal deaths
For the years 2004 and 2005, there were 116 maternal deaths reported from health facilities.Citation6 The direct causes of death were eclampsia, ante-and post-partum haemorrhage, obstructed labour, ruptured uterus, sepsis, pulmonary embolism, anaesthesia and disseminated intravascular coagulation, while indirect causes of death were malaria, AIDS, cancer and unknown causes (Boitumelo Thipe, National Safe Motherhood Programme Coordinator, Personal communication, 2007).
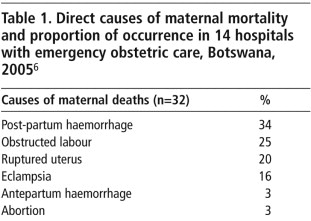
Table 1 shows the direct causes of maternal death in 2005. Ante-partum and post-partum haemorrhage were a result of abruptio placenta, placenta praevia and grand multi-parity. In 2007, a woman who was pregnant for the 15th time died of haemorrhage. Eclampsia is very common mainly because of hypertensive disorders of pregnancy. Also, high blood pressure is very common among the general population of Botswana. It was not clear from the forms whether the women who died had had eclamptic fits or pre-existing hypertension.
Abortion-related mortality is associated with the restrictive abortion law in Botswana. Abortion is only legal if the pregnancy is a result of rape, incest or defilement, or if pregnancy will result in poor maternal health, such as in situations where a woman has been diagnosed with cancer. Abortion is also legal if the pregnancy poses a risk to the woman’s life, or if the child would suffer serious physical or mental handicap. Two doctors have to confirm in writing that at least one of the conditions applies. Due to the restrictive nature of the law, some women with an unwanted pregnancy resort to illegal and in most cases unsafe abortion, often with crude instruments.Citation15Citation16 Abortion among HIV positive women is also common. The statistics on abortion are extremely inaccurate as abortion is under-reported for fear of repercussions.Citation17 Some of the women who have had induced abortions present with septicaemia and the underlying cause may be missed or not recorded. The unreliability of statistics is exacerbated by the fact that abortion is very secretive in Botswana.
There is a high rate of HIV (37–40%) among women of reproductive age in Botswana.Citation5 For 2004 through 2006, there were 6, 16 and 7 AIDS-related deaths, respectively. For the same time period, there were nine unclassified maternal deaths.Citation7
Contributory factors to maternal deaths were lack of blood supply for transfusion, delay in the decision to seek health care due to lack of knowledge about complications of pregnancy and delivery, delay in reaching a health facility due to transport problems and poor obstetric management. An association was found between grand multiparity and maternal mortality, but the MH2000 form does not collect data on other socio-cultural factors such as literacy, employment status, socio-economic status or early marriage.
In 2007, two out of 21 cases of maternal death to date occurred due to lack of blood (Boitumelo Thipe, National Safe Motherhood Coordinator, Personal communication, 2007). Some families in Botswana are living in great povertyCitation18 and do not have motor vehicles to transport the labouring woman to the nearest health facility. Although the government of Botswana has a policy that allows families to engage a private vehicle for emergencies, some families are not aware of this provision. As a result, they delay seeking help while negotiatiating with vehicle owners for cheaper rates. Some women arrive on time at the health facility, but due to a shortage of professional staff, there is a delay in obtaining emergency obstetric care.Citation19 For instance, one of the maternal deaths reported early in 2007 was due to failure to obtain emergency obstetric care as the only available doctor was engaged in theatre (Boitumelo Thipe, National Safe Motherhood Coordinator, Personal communication, 2007).
Neonatal data
Routine health statistics showed that there were 600 neonatal deaths and 36,000 live births in Botswana in 2004. This translates to a national neonatal mortality rate of 16.6 neonatal deaths per 1,000 live births. The proportion of neonatal deaths varied by facility, with a range of 21 to 52 deaths per 1000 live births. The facility which recorded the highest neonatal deaths was a referral hospital. Of the 36,000 live births in 2004, 4,668 infants weighed less than 2.5 kg, or 13% were of low birthweight.
Process indicators
In relation to process indicators, a community-based national impact survey conducted in 2001 revealed that 70% of pregnant women attended antenatal care either in the second or third trimester. The same survey found that access to emergency obstetric care was uneven. In the Eastern and Southern regions, 28 out of 34 sampled clinics were located 50 km or less from an emergency obstetric care facility, while in the Western region, the average distance was over 181 km. All surveyed facilities, including clinics with maternity care, reported that they provided labour and delivery services on a 24-hour basis, while out of 14 sampled hospitals, 11 provided comprehensive emergency obstetric care.Citation20
In 2006, the Sexual and Reproductive Health Unit of the Ministry of Health conducted a facility-based assessment study to obtain baseline data on the availability and utilisation of emergency obstetric care services in the country.Citation6 The assessment included two out of three referral hospitals, four out of 13 district hospitals, eight out of 18 primary hospitals and 14 out of 102 clinics with maternity care, a total of 28 maternity-based facilities surveyed out of a total of 136. Health facilities without maternity services were not surveyed. The study found that all facilities with maternity services provided 24-hour labour and delivery care. Fourteen of the 28 provided laboratory, theatre and anaesthetic services and blood supply. Over 50% of the doctors and 67% of the midwives were trained in life-saving skills. Most essential services were conducted by qualified medical officers and midwives.
Not all hospitals provided comprehensive emergency obstetric care, and not all health facilities had essential supplies and equipment. Three out of four district hospitals were providing comprehensive essential obstetric care while two out of eight primary hospitals were providing basic essential obstetric care. Unfortunately, the survey report did not state the names of the facilities providing comprehensive or basic care. As a result, it is not possible to account for which population received one or the other.
The proportion of births in facilities with essential obstetric care (76%) and of caesarean sections (7%) as a percentage of all expected births were found to be within the UN-recommended levels. As to availability of essential drugs, the study revealed that antibiotics were available in abundance for emergency obstetric care while magnesium sulphate and diazepam were in short supply, especially in district hospitals. Oxytoxic drugs such as ergometrine and syntometrine were also in short supply. There were shortages of other types of equipment and supplies, such as manual vacuum aspiration kits, as well.
The case-fatality rate was 0.76, below the 1.0 recommended by the UN. However, it was found that most complications leading to a maternal death were not recorded. On the other hand, there were some improvements in communications, such as tele-medicine (where a specialist in a referral hospital is able to communicate with a doctor in a facility without an obstetrician–gynaecologist), a flying mission (patients are transported by aeroplane to a higher level of care) and improved road networks.
Discussion
The confidential Maternal Death Notification Form is generally a useful tool. However, it only captures hospital-based data, which can be a poor reflection of the extent of the maternal mortality at district and national levels. District and national mortality estimates require information on all deaths, institution and community-based. Also, if not all deaths are reported through the form or are incomplete, then there is under-reporting of maternal deaths, which in turn may lead to incorrect projections in relation to resource requirements. It is hoped that the shorter form will encourage submission of complete and reliable data.
Monitoring through the MH2000 form has revealed that there are problems at both facility and district levels. First, it has been observed that facility-based committees are not functioning optimally and do not meet regularly. There seems to be lack of ownership as the committees are attached to individuals rather than positions or cadres. Regular monitoring and supervisory visits to the districts by the secretariat of the Sexual and Reproductive Health Unit could help resuscitate the committees at both facility and district levels.
Research on maternal mortality process indicators has so far been limited to a few small-scale quantitative studies. These studies also focus only on the number of facilities providing basic and comprehensive essential obstetric services without reference to the population covered.
Some of the data collected on process indicators could not be relied upon. For instance, although the caesarean section rate was found to be within the acceptable range, indications for the operation were not recorded. As a result, it is not clear whether surgery was appropriate or not. Although it is possible to trace the indications from obstetric records, it is not easy to get hold of these records since computerisation of patient data is relatively new in Botswana.
The monitoring system has helped to improve and expand some aspects of maternal health care. Due to the findings of the monitoring system, maternal death was made a notifiable event in 2006 and plans are underway to enact legislation to criminalise the failure to report maternal deaths. Furthermore, extensive training for skilled attendants is ongoing. The Ministry of Health has intensified recruitment of qualified midwives and doctors from other countries, such as Cuba and China. As of June 2007, a medical school has been set up at the University of Botswana in Gaborone, the capital of Botswana, and the first intake of medical students is expected by 2008. It is hoped that the existence of the medical school will increase the number of skilled attendants for childbearing women.
We have also made the following recommendations for improvements in maternity care and monitoring of the maternity services:
| • | Information for the community should be strengthened on utilisation of private vehicles in cases of obstetric emergency. | ||||
| • | Staffing and equipment norms per level of care concerned with maternity services should be established. | ||||
| • | The secretariat of the Sexual and Reproductive Health Unit should train facility and district level committee members in the importance of data collection, collation and analysis. Members of these committees should meet periodically to analyse data and make evidenced-based decisions about future care. | ||||
| • | In order to address non-institutional maternal deaths, the various monitoring committees (at facility and district level) should include representatives from local government, non-governmental organisations, community leaders and other relevant stakeholders. | ||||
| • | The Sexual and Reproductive Health Unit and Department of Civil Registration need to develop a mechanism to interface medical records and the civil registration system to allow timely delivery of data. The Central Statistics Office and Sexual and Reproductive Health Unit should collaborate and work closely for the harmonisation and reliability of health statistics. | ||||
| • | The manager of the Sexual and Reproductive Health Unit should ensure that reporting by all health facilities is mandatory. The heads of maternity services, and obstetrics and gynaecology, should appoint or delegate a medical doctor or midwife as the focal person. | ||||
| • | The Ministry of Health, academic institutions and other research centres such as Botswana Institute of Development and Policy Analysis should conduct another study of process indicators which covers a representative sample of facilities that provide maternity services. | ||||
| • | The Ministry of Health should liaise with Central Medical Stores to ensure timely and adequate procurement of essential drugs. | ||||
| • | Guidelines on the management of obstetric emergencies must be displayed and followed in all maternity service centres. | ||||
In conclusion, the findings of the review of the National Maternal Morbidity and Mortality monitoring system have highlighted the constraints on the accurate reporting and recording of maternal deaths and obstetric complications. The existing information points to the need for continued monitoring and further health system changes based on the findings.
Acknowledgement
We acknowledge the National Safe Motherhood Coordinator for assistance with some of the data used in this paper.
References
- Government of Botswana, United Nations. Botswana Millenium Development Goals. Status Report. 2004; Tiger Design and Graphics: Gaborone.
- OL Omondi, M Kobue. Determinants of Maternal Mortality in Botswana: An Institutional, Household and Community Perspective. 1993; Government Printer: Gaborone.
- WHO/UNICEF/UNFPA. Maternal Mortality in 1995: Estimates Developed by WHO/UNICEF/UNFPA. 2001; WHO: Geneva.
- World Health Organization. Maternal Mortality: A Global Fact Book. 2000; WHO: Geneva.
- Ministry of Health. Report of the 2004 Maternal Morbidity and Mortality Conditions in Botswana. 2005; MOH: Gaborone(Unpublished)
- Ministry of Health/WHO/UNFPA. Emergency obstetric care assessment in selected health facilities in Botswana. 2006; MOH: Gaborone(Unpublished)
- Ministry of Health. National Maternal Mortality Audit Committee Report. 2007; MOH: Gaborone(Unpublished)
- Central Statistics Office. Botswana Multiple Indicator Survey. 2001; Government Printer: Gaborone.
- Central Statistics Office. Botswana Housing and Population Census. 2001; Government Printer: Gaborone.
- Ministry of Finance and Development Planning. National Development Plan 9. 2003/04–2008/09. 2003; Government Printer: Gaborone.
- WHO/UNICEF/UNFPA/Ministry of Health. The Safe Motherhood Initiative: the maternal morbidity and mortality monitoring system in Botswana. Gaborone, 1998. (Unpublished)
- UNICEF/UNFPA/Ministry of Health. The Maternal Morbidity and Mortality Monitoring System in Botswana. 2002; Government Printer: Gaborone.
- T Wardlaw, D Maine. Process indicators for maternal mortality programmes. TKS avindran, TKS Ravindran. Safe Motherhood Initiatives: Critical Issues. 1999; Reproductive Health Matters: London, 24–30.
- D Maine, P Bailey. Indicators for design, monitoring and evaluation of maternal mortality programs. January. 2001 At: <www.amdd.hs.columbia.edu/docs/monitoring.rtf>. Accessed August 2007
- Letamo G, Mejelantle R. The reproductive health problems of teenage childbearing in Botswana. Gaborone, 2000. (Unpublished)
- J Strickler, A Heimburger, K Rodriguez. Clandestine abortion in Latin America: a clinic profile. International Family Planning Perspectives. 27(1): 2001
- Letamo G, Bainame K, Majelantle R. Clandestinely induced abortion in Botswana. Gaborone, 2006. (Unpublished)
- S Shaibu. Community home based care in a rural village: challenges and strategies. Journal of Transcultural Nursing. 17(1): 2006; 1–6.
- UNFPA. Maternal Mortality Update 2002: A Focus on Emergency Obstetric Care. 2003; UNFPA: New YorkAt: <www.unfpa.org/Publications>. Accessed December 2006
- Central Statistics Office. Botswana AIDS Impact Survey: Statistical Report. Gaborone: Government Printer, 2001.