Abstract
Maternal mortality reduction in many countries is unlikely despite the availability of inexpensive, efficacious interventions that are part of official policy. This article explores the reasons why, based on research on maternity services in Bangladesh, Russia, South Africa and Uganda. A simple dynamic responses model shows that the key to understanding challenges in implementation lies in the reflexive, complex and dynamic responses of health workers and community members to policies and programmes. These responses are “dynamic” in that they arise due to forces from within and outside the system, and in turn exert forces of their own. They result in the difference between the health system that is envisaged in policy, and what is implemented by health workers and experienced by users. Programmes aiming to improve maternal health are not only technical but also social interventions that need to be evaluated as such, using methodologies that have been developed for evaluating complex social interventions whose aim is to bring about change. The components of effective programmes have been defined globally. However, in getting what works to happen, context matters. Thus, technical advisors need to give “advice” more circumspectly, local programme managers must be capacitated to make programme-improving adjustments continuously, and the detail related to process, not just outcomes, must be documented in evaluations.
Résumé
Une réduction du taux de mortalité maternelle est improbable dans beaucoup de pays, malgré la disponibilité d’interventions efficaces et peu coûteuses incluses dans la politique officielle. Cet article cherche à comprendre pourquoi, avec des recherches en Afrique du Sud, au Bangladesh, en Fédération de Russie et en Ouganda. Un modèle simple de réponses dynamiques montre que pour comprendre les problèmes de mise en oeuvre, il faut étudier les réponses dynamiques, complexes et réfléchies des agents de santé et des membres de la communauté aux politiques et programmes. Ces réponses sont « dynamiques » en cela qu’elles sont créées par des forces à l’intérieur et à l’extérieur du système, et qu’elles exercent à leur tour une force. Leur résultat est la différence entre le système de santé envisagé dans la politique et celui qui est appliqué par les agents de santé et que connaissent les usagers. Les programmes d’amélioration de la santé maternelle sont des interventions techniques, mais aussi sociales qui doivent être évaluées comme telles, avec des méthodologies élaborées pour jauger des interventions sociales complexes destinées à déclencher un changement. Les composantes de programmes opérants ont été définies au niveau international. Néanmoins, le contexte est important pour appliquer des mesures efficaces. Les conseillers techniques doivent donc « conseiller » avec plus de circonspection, il faut que les directeurs de programmes locaux soient capables d’ajuster constamment les programmes pour les améliorer et que les évaluations informent des détails liés au processus, et non pas seulement des résultats.
Resumen
En muchos países, resulta improbable disminuir la tasa de mortalidad materna, pese a la disponibilidad de intervenciones eficaces y poco costosas que son parte de la política oficial. En este artículo se explora el porqué, a raíz de investigaciones sobre los servicios de maternidad en Bangladesh, Rusia, Sudáfrica y Uganda. Un simple modelo de respuestas dinámicas muestra que la clave para entender los retos de la implementación radica en las respuestas reflexivas, complejas y dinámicas de los trabajadores de la salud y miembros de la comunidad a las políticas y los programas. Estas respuestas son “dinámicas” en el sentido de que emergen debido a fuerzas dentro y fuera del sistema, y, a su vez emplean sus propias fuerzas. Tienen como resultado la diferencia entre el sistema de salud que es concebido en la política, y lo que es puesto en práctica por los trabajadores de la salud y experimentado por las usuarias. Los programas que procuran mejorar la salud materna no son sólo técnicos sino también intervenciones sociales que deben ser evaluadas como tal, utilizando metodologías que fueron creadas para evaluar intervenciones sociales complejas cuyo objetivo es promover cambios. Los elementos de los programas eficaces fueron definidos mundialmente. Sin embargo, para lograr que suceda lo que funciona, importa el contexto. Por tanto, los asesores técnicos deben dar “consejos” con más cautela, los administradores de programas locales deben recibir capacitación para realizar ajustes que mejoren los programas continuamente, y el detalle relacionado con el proceso, y no sólo los resultados, debe documentarse en las evaluaciones.
In the last three years there have been a number of important publications on maternal health, including the World Health Report 2005, the Child and Maternal Health Task Team report on Transforming Health Systems for Women and Children and the Lancet series on maternal survival.Citation1–7 These have made valuable contributions, summarising current thinking among the most renowned experts in this area on why we have not made progress in terms of reducing maternal deaths, and what needs to be done to change the situation.
In the most recent Lancet series, one contribution focused on “getting on with what works”Citation1Citation7 and another on “going to scale with professionally skilled care”Citation7. These emphasise the need to invest in maternal health, and the elements of maternal care packages to invest in. For example, they summarise evidence that a health centre-based strategy providing intrapartum care will have the greatest effect on maternal mortality, and that a scaled-up maternal care workforce is needed. Campbell and GrahamCitation1 make the point that “strategies will work if the component packages are effective and the means used for their distribution achieve high coverage of the intended target group” (Key messages, p.1284).
At the end of a five-year programme of health system research in Bangladesh, Russia, South Africa and Uganda with maternal health services as a key focus area, we have come to the conclusion that this argument needs to be turned on its head. A greater focus is required instead on the principle that strategies will not work if the component packages are not rendered effective and the means used for their distribution do not achieve high coverage of the intended group. In maternal health, there are a range of demonstrated efficacious interventions that should reduce maternal mortality. Many of them are official policy almost everywhere where they need to be in place. But as is widely acknowledged in practice, and to a greater degree in lower-than in higher-income countries, intended interventions are not being provided effectively where they are needed. Refining the set of interventions to achieve the best combination of the most efficacious interventions does not address this problem.
One factor that often contributes to the failure to deliver planned interventions effectively is the failure to invest sufficient resources. This implies that inputs will not be physically available. Inadequate numbers of skilled birth attendants, highlighted by KoblinskyCitation7, provides an example of this failure, clearly a widespread one. The call for more resources is therefore appropriate. Inputs may also be poorly distributed – an individual or group intended to receive the intervention, a health worker qualified to deliver the intervention and the instruments and supplies required all need to be in the same place at the same time to make the effective delivery of the intervention possible. All three may not be present simultaneously due to failures of logistics systems, inadequate training opportunities, poorly planned delivery strategies and other factors capable of technical resolution. Again, advice regarding such matters from technical experts is helpful.
However, there are also frequent examples of failure to render strategies effective or to deliver them to intended groups despite the availability of inputs and appropriately trained staff in the right place at the right time. In some of these cases, while availability of inputs and staff are problematic, it is other factors that have derailed the interventions and made them ineffective. This paper focuses on these constraints to maternal survival.
The Health Systems Development Programme
The Health Systems Development Programme was a Department for International Development (DFID) Knowledge Programme which ran from 2001 to 2006. The majority of work in this programme was carried out in Bangladesh, Russia, South Africa and Uganda. This selection of countries contrasted “transitional” middle-income countries, whose principal health system failures resulted from inequalities, with low-income countries, whose health system problems were more uniformly distributed. Both these system problems are important for addressing maternal survival globally, but they may exhibit quite different systemic characteristics. The Programme focused on a range of health services and conditions as “probes” that could give insight into the functioning of the health system. Maternal health services rely on a functioning health system at a range of different levels, and they make particular demands on the periphery of the system to function in emergencies.
At the start of the programme a situation analysis of maternal health services was undertaken in all four countries involving review of published and grey materials, interviewing key actors, and analysing available secondary data. The research programme then carried out a range of projects exploring key issues that arose out of the situation analyses. In Bangladesh and Uganda, where utilisation of services was the key issue, this was the focus of subsequent studies. In Russia, factors that explained large variations in practice and outcomes in facilities and why evidence-based clinical knowledge was not embraced and implemented by practitioners, were investigated. In South Africa, where poor provider practice was identified as a key factor contributing to maternal deaths, the main focus was on factors shaping the practice of midwives in maternity wards, and also those influencing staffing levels, turnover and motivation. Full details of all these research projects and publications are available at <www.hsd.lshtm.ac.uk/links/index.htm>.
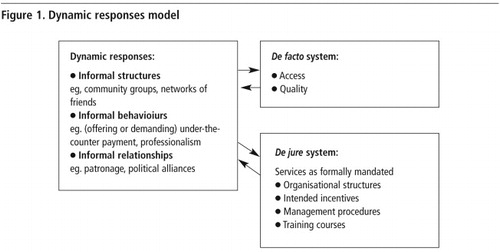
Towards the end of the programme, arising out of joint reflections on work on maternal health completed across the four countries as well as other probes, a conceptual framework was developed (). In this model, context as well as health care workers, patients and community responses are recognised as shaping how local health systems operate, and the success or lack of success of new policies and programmes attempting to improve maternal health services within that environment.
The framework emphasises: 1) more complex processes of determination, i.e. not just simple cause-and-effect relationships but chains of factors, potentially quite long, causing multiple interactions, and 2) the social nature of the functioning of health systems, i.e. the importance of interaction between human actors. This approach acknowledges that health care workers are complex human beings, motivated by a range of different financial and non-financial incentives, steeped in cultural and professional value systems. They are not robots, who blindly without thinking implement whatever they are told, nor are they angels who think of nothing but the good of their patients.Citation8 Similarly, patients and the communities in which they are based are not empty vessels waiting for “education” or for financial and physical barriers to be lifted, but are active participants in a series of processes that do or do not result in effective access. The “often messy behaviour of individuals is often difficult to quantify”.Citation9
In this model, the responses of health care workers and community members are the lynchpin between formal arrangements (the de jure system, what is meant to happen), and the de facto system (what is actually happening in facilities and experienced by people who use health services). These responses are labelled “dynamic” in the sense that they arise due to forces from within and outside the system, and in turn exert forces of their own. Whilst formal arrangements offer the entry point for intervention, the ability of people to access services responsive to their needs crucially depends on how health care workers and managers who are implementing the de jure system respond. As such, the relationships and contexts that exist on the ground are as important as the set of inputs, and must be addressed accordingly. The policy, and how the policy is implemented and why, are equally important and worthy of forethought and evaluation. The development of programmes and policy that improve outcomes for users therefore requires direct engagement with context and with how formal organisational structures, intended incentives and management procedures interact with informal structures, behaviours and relationships on the ground.
The critical feature of the model is that it draws no direct link between the de jure and de facto systems, and therefore no necessary link between the provision of inputs and the organisation and management of these inputs de jure, and the outcomes that emerge. The only health system that can be experienced by its users is the one that emerges from multiple human interactions.
Studies focused on dynamic responses in maternal health
We draw on examples from our work to illustrate what we are trying to argue in the model. We have used our own work partly because we are most familiar with it, but also because although the issues that we identified are not unique to our research, our work was motivated by exploring these dynamics. In other research informal relationships, informal structures and informal behaviours are acknowledged, but how they interact and influence policy or strategy has rarely been the central focus.
South Africa
The situation analysis of maternal health services in South Africa concluded that South Africa performs poorly for a middle-income country with a considerable health infrastructure, availability of staff, legal abortion, free health care for pregnant women and high levels of utilisation of delivery services (92% in the 1993 Demographic and Health Survey). Key explanatory factors identified included high levels of inequality, impact of HIV/AIDS, and problems with provider practice and motivation. Two studies were then carried out that further explored provider-related issues.
An ethnography of two labour wards
This study was carried out in two district hospitals, one urban and one rural. The project aimed to explore the factors that shaped provider practice given that it had been identified as a major contributor to maternal deaths.Citation10 The study found a considerable gap between the practice set out in national policy documents (the de jure system), and what was in reality happening in the labour wards in terms of patient care (the de facto system). Midwives were mired in a hierarchical system, where they were struggling to implement a huge range of new policies, mostly not directly maternal health-related. Faced with huge demands, they prioritised policies that they believed their managers cared most about, ones they would be penalised for not implementing or ones they could implement easily. They implemented aspects of new policies that were easy – putting up posters with guidelines for treatment of major causes of maternal death, for example, but little was done to support the guidelines otherwise. More complex or difficult changes, particularly if they impacted on the culture of the facility or challenged existing power dynamics, were ignored. The intention of policies was rarely explained or discussed with staff; instead, they were presented with a list of tasks that had to be carried out.
This was particularly noticeable with a range of policies that attempted to empower patients and improve patient–provider relationships. Nurses had to wear name labels, and were penalised by managers if they did not, but it was not clear (or regarded as important by those same managers) that this improved relationships with patients. During the study, the researcher observed one senior nurse ridiculing patients for not being able to read the name labels, and in numerous interactions observed that patients never used nurse’s names or appeared to remember them if they wanted to complain about a particular nurse. Suggestion boxes were on the wall in both wards. In one hospital, there were no slips, while in the other hospital, patients were routinely asked to fill in slips as part of the hospital discharge process. Patients’ comments on the slips were used to write monthly reports which were submitted to the hospital management and the provincial government, but the content of the complaints was not addressed. What was seen as important, and what was evaluated as part of the ward manager’s job performance, was that the reports were written.
Another clear example of where informal relations had an impact on the de facto services that were provided, related to training. Training did take place but there was contestation about who received it between staff in the ward, and between management and unions. This meant that training was not always fed back to the rest of the ward, and that inappropriate people received training to make sure that it was “fair”.Citation11
In terms of patient and community responses, the ethnographic study found that patients were making decisions about which hospital they wanted to deliver in, which was counter to what health planners had envisaged. For example, both white and black women preferred to deliver in what had previously been white-only hospitals, due to a perception that the quality of care was better. This occurred despite the fact that these hospitals were further from where they lived, were lower level hospitals and caesarean sections were not always available.Citation11
Nursing staff dynamics in maternity wards
A second study was carried out in three of the poorest provinces in South Africa. A fax questionnaire was sent out to all public sector hospitals providing maternity services in the three provinces. Site visits were made to 15 hospitals and 27 clinics selected through multi-stage cluster sampling. The study had four components: a tool to measure staff turnover, absenteeism, vacancy rates and workload; a motivation survey; a discrete choice experiment; and a qualitative section that explored nurse managers’ views of the challenges of managing and retaining staff in maternity wards. The study found that nursing staff were demotivated and over half were considering leaving. Inadequate pay, poor promotion prospects, feeling unsupported by management and poor relationships with colleagues were all associated with lack of organisational commitment. The discrete choice experiment found that both financial and non-financial factors influenced nurses’ decisions about their work. Good management and a well equipped hospital were as influential over nurses’ decisions of where to work as a 15% pay increase.
The qualitative section of the research identified many examples of policies that were not working as intended. For example the South African government introduced a rural allowance to retain staff in rural areas. However only professional nurses and not lower grades of nurses received the allowance, and this had caused high levels of tension in maternity wards. The reform appeared to have had the impact not only of demotivating the staff who did not get the allowance but also causing “double demotivation”Citation12 among staff who did get the allowance, who felt guilty, embarrassed or awkward that their colleagues did not, and struggled with staff they were managing who said: “You get the allowance, you do the work”.
Another key finding was that in many of the hospitals, ward and hospital managers were struggling with their roles. Many were “acting” in their positions and felt that they had responsibility without reward. Many expressed the belief that appointment processes were not fair. “They give the job to just anybody, usually they are the girlfriend of somebody, it doesn’t matter if they don’t know anything about management.”
In some of the facilities there had been a high turnover of management, and in some facilities management was in disarray. For example, in one facility three different staff members identified themselves as the acting chief executive officer. In other hospitals management and staff were locked in conflict over particular issues which affected all aspects of working in the hospital, including staff refusing to implement various policies and aspects of patient care as a challenge to the chief executive.Citation13
In these circumstances it is difficult to imagine how an intervention aimed at improving aspects of maternal health would not be fundamentally distorted.
Russia
In Russia the situation analysis found that despite an extensive infrastructure that is widely used by women, the system fails to achieve good health outcomes. One explanation for this has been that marginalised groups, who are most in need, face systematic barriers to access, and services may not be responsive to their needs.Citation14Citation15 A second key finding was a wide variation in practice in maternity units, as well as deviation from internationally recognised evidence-based practice. For example, many women were hospitalised for long periods of time after their pregnancies were labelled “abnormal”.
Explaining variation in provider practice in Tula oblast
The Tula region was selected for study due to the availability of a database that had been set up to collect extended data on pregnancies and birth outcomes in the region.Citation15 The study involved secondary data analysis, in-depth interviews with policymakers, practitioners and facility managers as well as a review of policy documents.
The birth rate in Tula, as in the rest of Russia, fell by half between 1987 and 1999. However, the de jure system did not respond – neither bed capacity levels nor incentives to maintain capacity, which linked funding to bed numbers, were adjusted. The result in the de facto system was an increase in the number of women hospitalised for poorly defined conditions such as “prevention of miscarriage”. In some facilities, all expectant mothers were hospitalised for this reason, typically for 28 days. The proportion of beds used for these sorts of antenatal conditions compared to those used for delivery increased from 21% to 45% of all maternal beds between 1985 and 2001.
Further changes made informally at local level were to allow now unnecessary posts to remain vacant and to use the resulting budget surplus to pay others more and to fill unbudgeted but more needed roles in administration and specialist care such as anaesthesia.
The study found a highly regulated de jure system specifying a long list of procedures. In many cases, “obligatory protocols” did not reflect international evidence of effectiveness. They included routine enema and shaving, recumbent bed position in labour and routine fetal monitoring. However, few of those interviewed could recall these provisions; they were more familiar with older decrees of the Soviet Union that prescribed the required structure of the maternal health services. Routine obstetric practices were equally uninformed by international evidence, and included routine prescription of multivitamins and strict dietary restrictions, for example, on red fruit and vegetables.
The application of some procedures was found to be associated with patient characteristics that had no obvious link to a need for the procedure. Younger rather than older patients were more likely to receive amniocentesis, for example.
The study highlighted resistance to formal change in the system examined, which was exemplified by the failure to respond to falling birth rates, but a level of informal responsiveness, exemplified by the flexibility with which resources intended to reimburse maternal health workers could be used instead for prioritised purposes. Some informal responses, such as this one, compensated for formal policy weaknesses, whereas others were more likely to exacerbate these. It was suggested that effective policy would need to start by recognising the system’s capacity for informal response.
Bangladesh and Uganda
In Bangladesh and Uganda, two key issues arose in the situation analyses: firstly, low levels of utilisation of available maternity services were identified as the major constraint to progress in maternal survival, and secondly, the impact of health sector wide reforms on maternity services was found to be important. These factors dominate both situation analyses. Two joint research projects on factors influencing utilisation and on the impact of health sector reforms on health care workers were then undertaken to explore these issues further. Only the first of these is reported here, for reasons of space. The health sector reform study corroborated the conclusions of the South African studies – policies intended to leverage efficiency and equity gains were often distorted by their interpretation and implementation, producing unintended consequences. This emphasises the evolving dynamics of the whole system as the context in which the more micro-level dynamic responses that we are focusing on work themselves out.
Motivations and strategies for accessing obstetric care in Uganda and Bangladesh
The first study was a qualitative study that, instead of exploring reasons for non-utilisation of maternity services, focused on women who did deliver in facilities, the motivations behind this and how they and their families managed to overcome access barriers to delivery care that have been well documented in both countries. The study was conducted in one rural district each in Bangladesh and Uganda. In each country, 30 women who had recently delivered in a facility were interviewed.
In Uganda, 28 of the 30 women interviewed had planned to deliver in a facility; the principal motivation they mentioned was fear of possible antenatal and delivery complications. For example, one woman said: “It is better to deliver in a health centre because a woman can get immediate professional attention, especially if there are complications.” Citation16
Husbands were reported to have started saving at the beginning of the pregnancy to pay for transport costs; maternity care itself was free, or informal payments were relatively small. Women also reported that in their social circle most women believed it was right to deliver in facilities. This was surprising in an area where facility-based deliveries were only 39% of all births. This might be a clustered pattern of health care-seeking behaviour, in which groups of women connected through a social network may have higher then average rates of use of facilities, suggesting a set of dynamic responses among service users within a network. An alternative explanation, however, could be respondent bias; women may have felt this was the “correct” answer to give when asked about their friends’ practices.
In Bangladesh, the situation was different. Twenty-two of the 30 women had first attempted to deliver at home, believing that was the correct thing to do, and only when the delivery had not progressed well had they attempted to seek help at the clinic or hospital. Of those women who did plan to deliver in hospital, two had lost babies in previous home deliveries and one had lost a sister to a maternal death. Hence, even most of those who did deliver in hospital did not see it as the norm.
Whereas in Uganda women reported that they and their husbands were the ones involved in the decision-making, in Bangladesh a much wider array of people were involved, including extended family members, community members and a range of traditional health care providers, such as spiritualists, herbalists, traditional birth attendants and local, unqualified “village doctors”. Community members, including policemen, teachers and untrained medical practitioners, played an important role in persuading women and their families that a facility-based delivery was needed, and facilitating it to happen.Citation16
Although in Uganda women were generally happy with the care that they had received, in Bangladesh there was distrust on the part of many of the women in relation to caesarean delivery. Some women alleged that caesarean section was used when not medically indicated, and suggested that financial incentives motivated the advice provided by both doctors and midwives.Citation15,17,18
In Uganda, existing strategies to improve maternal survival outcomes include a new sub-district health system, intended to bring emergency obstetric care closer to households, and in Bangladesh, the equipping and staffing of a primary health care network with the capacity to provide emergency obstetric care. Again, the findings imply that these strategies are mediated by a complex set of dynamic responses to available services, in this case largely operating within communities and between patients and their community. Strategies informed by this understanding have a better chance of success. For example, it was suggested that in Bangladesh, a flexible set of criteria indicating to women the need for delivery in a facility might make it easier for women to access care, given the socially approved norm of home delivery.
Discussion and conclusions
The first priority for low-and middle-income countries is to devise better strategies to implement effective interventions. More evidence about effectiveness of interventions does not support that priority. The simple conceptual model we have proposed seeks to put the strategic emphasis on managing implementation rather than devising and refining the content of intervention.
Intervention programmes set off a series of dynamic responses that interact in a manner characterised by complexity.Citation19 One implication is that an apparently insignificant detail can be amplified in its effects through a series of chain reactions. Similarly, the effect of a seemingly significant component of a reform or policy can be dampened down by dynamic responses. Hence, predicting the impact of an intervention becomes an art rather than a science that is based on recognising familiar patterns of response and preparing for their possible occurrence.
What this means for getting what works to happen is that strategies that have been evaluated as effective elsewhere are a starting point rather than an end point. It is often noted that “the devil is in the detail”. And details are what studies of maternity services need to focus on, so that patterns can be deduced and strategy tailored to take account of responses that have been observed in other studies. The critical importance of these factors to outcome is not reflected adequately in the policy advice currently being offered, or given the attention in official reports and publications that it deserves.
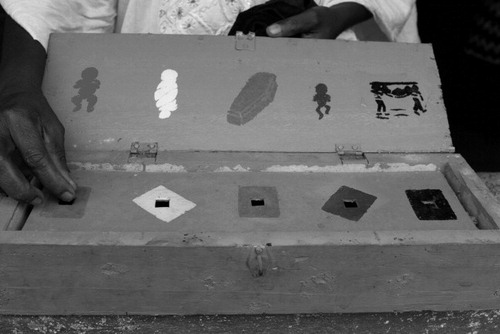
For example, a programme may be defined as “training midwives” or “expanding skilled birth
Village midwives in Sierra Leone use this box to record births, putting a pebble through the relevant hole. Symbols on the lid from left to right are: live birth, cord wrapped around the baby, baby has died, baby is low birthweight, mother has complications and has been taken to hospital.
The dynamic response model necessitates a different way of evaluating the impact of the outcomes of maternal health interventions, and explaining what did and did not work. Programmes and policies that aim to improve how maternal health care is delivered are social interventions, not only technical ones. Therefore, instead of trying to repeat effectiveness study methods that have worked well in clinical sciences, methods of evaluation need to be developed that enable learning to take place, and patterns to emerge, while also acknowledging the role of the reflexive, complex dynamic responses of staff and community to any policies and programmes.
There is already a large literature exploring how to evaluate complex social interventions that builds on this understanding, yet it has been little applied to maternal survival programmes in low and middle-income countries. For example, the Aspen Institute in Washington DC has, since 1992, been developing methods for community intervention and its evaluation. It emphasises, in its publications, the need for a “theory of change” that drives intervention design, implementation strategy and evaluation. This theory of change is derived from consultation between groups of stakeholders and evaluators to articulate what are perceived as the key elements of a programme that motivate change. This theory becomes the hypothesis to be tested against data gathered by evaluators. The theory requires evidence of community change and the key elements that have underpinned it in other contexts: “A better knowledge base will help us develop better theories of change, and better theories of change will improve both the design of our initiatives and the opportunities for learning about change.” Citation21
Pawson and TilleyCitation22 have advocated a similar approach, labelled “realistic evaluation” in which they focus on “context–mechanism–outcome configurations”, i.e. that in specific contexts, mechanisms of effect operate to produce an outcome. Programmes work by introducing new ideas and/or resources into an existing set of social relationships. A crucial task of evaluation should be to include (via hypothesis-making and research design) investigation of the extent to which these pre-existing structures enable or disable the intended mechanisms of change. This would then allow policymakers in other countries to look at patterns that develop across countries, to learn from mistakes and problems experienced, as well as successes.
Plausible components of effective programmes can be and have been defined globally. However, the detail is critical to getting what works to happen and must be defined locally in space and time (i.e. not once-and-for-all but on a continuous basis of re-evaluation). This implies:
| • | that international agencies and technical advisors need to give “advice” more circumspectly, | ||||
| • | that it is necessary to capacitate local programme managers to continuously make programme-improving adjustments, and | ||||
| • | that when evaluating programmes and learning lessons, the detail related to process, not just outcomes, must be documented. | ||||
Acknowledgements
The Health Systems Development Programme was funded by the UK Department for International Development.
References
- O Campbell, W Graham. On behalf of Lancet Maternal Survival Series steering group Strategies for reducing maternal mortality: getting on with what works. Lancet. 368: 2006; 1284–1299.
- J Borghi, T Ensor, A Samanathan. Lancet Maternal Survival steering group. Mobilising financial resources for maternal health. Lancet. 368(9545): 2006; 1457–1465.
- World Health Organization. The World Health Report 2005: Make Every Mother and Child Count. 2005; WHO: Geneva.
- UN Millennium Project. Who’s got the power? Transforming Health Systems for Women and Children. 2005; UN: New York.
- C Ronsmans, W Graham. on behalf of Lancet Maternal Survival Series steering group Maternal mortality: who, when, where and why. Lancet. 368: 2006; 1189–1200.
- V Filippi, C Ronsmans, O Campbell. Maternal health in poor countries: the broader context and a call for action. Lancet. 368: 2006; 1535–1541.
- M Koblinsky, Z Matthews, J Hussein. Going to scale with professional skilled care. Lancet. 368: 2006; 1377–1386.
- D Blaauw, M Ambegaokar, B McPake. Neither angels nor robots: the ‘dynamic responses’ of health care workers and the unintended effects of health system functioning. 2006; Health System Development Programme: London.
- D Balabanova, J Parkhurst, M McKee. Access to health care: taking into account health systems complexity. 2006; Health Systems Development Programme: London.
- B Pattinson. Saving Mothers: Third Report on Confidential Enquiry into Maternal Deaths in South Africa 2002–2004. 2006; Department of Health South Africa: Pretoria.
- L Penn-Kekana. Ethnography of two labour wards. 2006; Health Systems Development Programme: London.
- S Carr, D McLoughlin, M Hodgson. Effects of unreasonable pay discrepancies for under and overpayment on double demotivation. Genetic, Social and General Psychology Monographs. 122(4): 1996; 475–494.
- L Penn-Kekana, D Blaauw, SK Tint. Nursing dynamics in the context of HIV/AIDS. 2004; Frontiers Programme, Population Council: Johannesburg.
- B Dimitrova, D Balabanova, R Atun. Health service providers’ perceptions of barriers to tuberculosis care in Russia. Health Policy and Planning. 21(4): 2006; 265–274.
- K Danishevski, D Balabanova, M McKee. Delivering babies in the time of transition in Tula, Russa. Health Policy and Planning. 21(3): 2006; 195–205.
- JR Parkhurst, SA Rahman, F Ssengoba. Overcoming access barriers for facility-based delivery in low-income settings: insights from Bangladesh and Uganda. Journal of Health Population and Nutrition. 24(4): 2006; 438–445.
- F Ssengooba, SA Rahman, C Hongoro. Health sector reforms and human resources for health in Uganda and Bangladesh: mechamisms of effect. Human Resources for Health. 5: 2007; 3.
- J Parkhurst, SA Rahman. Life saving or money wasting? Perceptions of caesarean sections among users of services in rural Bangladesh. Health Policy. 80(3): 2007; 392–401.
- Lewin. Complexity: Life at the Edge of Chaos. 2001. 2001; Phoenix: London.
- S Marks. Divided Sisterhood. 1994; Witwatersrand University Press: Johannesburg.
- P Auspos, AC Kubisch. Building Knowledge about Community Change: Moving Beyond Evaluations. 2004; Aspen Institute: Washington DCAt: <www.aspeninstitute.org/atf/cf/{DEB6F227-659B-4EC8-8F84-8DF23CA704F5}/BUILDINGKNOWLEDGE.pdf>. Accessed 16 August 2007
- R Pawson, N Tilley. Realistic Evaluation. 1997; Sage Publications: London.