Abstract
Our research explored the reproductive desires of HIV-negative women and their HIV-positive partners who underwent assisted conception based on sperm-washing and intrauterine insemination in Italy. Twenty-two semi-structured interviews were conducted with former patients (6 women, 5 men and 11 couples). Desire for children, perceived risk from treatment and acceptability of the insemination technique were some of the issues explored. Participants had the treatment for a mean duration of 3.5 years, with a mean number of cycles of 5.3. They were highly motivated to conceive a biological child to bring purpose to their lives, and strongly desired options to conceive safely. Most rejected spontaneous conception. Those who successfully conceived reported a positive impact on their quality of life, fulfilling their desire to be parents and restoring their sense of “normalcy”. Participants strongly supported extending assisted conception services to all HIV negative women living with HIV positive partners who wished to become pregnant and felt that withholding such treatment was not ethically justified. They perceived assisted conception services to be a safe and effective alternative to spontaneous conception, and felt that society has a moral obligation to provide such services.
Résumé
Nous avons étudié les souhaits de femmes séronégatives au VIH et de leurs partenaires séropositifs qui s’étaient soumis à une procréation assistée avec lavage du sperme et insémination intra-utérine en Italie. Vingt-deux entretiens semi-structurés ont été menés avec d’anciens patients (6 femmes, 5 hommes et 11 couples). Le désir d’enfant, la perception du traitement et l’acceptabilité de la technique d’insémination figuraient parmi les questions abordées. Les participants ont suivi le traitement en moyenne pendant 3,5 ans, avec un nombre moyen de 5,3 cycles. Ils étaient très motivés pour concevoir un enfant biologique afin de donner un sens à leur vie, et demandaient des options pour procréer en toute sécurité. La plupart rejetaient la conception spontanée. Ceux qui ont conçu un enfant ont indiqué que cela avait eu des retombées positives sur leur qualité de vie, en satisfaisant leur désir d’être parents et leur redonnant un sentiment de « normalité ». Les participants soutenaient énergiquement l’élargissement des services de procréation assistée à toutes les femmes séronégatives vivant avec des partenaires séropositifs et qui souhaitaient avoir un enfant, et ils pensaient qu’il était moralement injustifié de refuser ce traitement. Ils estimaient aussi que la procréation assistée était une option sûre et efficace à la conception spontanée, et jugeaient que la société avait l’obligation morale de fournir de tels services.
Resumen
Nuestra investigación exploró los deseos reproductivos de mujeres VIH-negativas y sus parejas VIH-positivas, que pasaron por la concepción asistida basada en el lavado de espermatozoides e inseminación intrauterina, en Italia. Se realizaron 22 entrevistas semiestructuradas con antiguos pacientes (6 mujeres, 5 hombres y 11 parejas). Algunos de los aspectos explorados fueron: el deseo de tener hijos, el riesgo percibido del tratamiento y la aceptación de la técnica de inseminación. Los participantes recibieron el tratamiento por una duración media de 3.5 años, con un número medio de ciclos de 5.3. Estaban muy motivados a concebir un hijo biológico para darle sentido a sus vidas, y muy deseosos de tener opciones para concebir de manera segura. La mayoría rechazó la concepción espontánea. Aquéllos que lograron concebir informaron un impacto positivo en calidad de vida, realizar su deseo de ser padres y restaurar su sentido de “normalidad”. Los participantes apoyaron enfáticamente extender los servicios de concepción asistida a todas las mujeres VIH-negativas que viven con parejas VIH-positivas, que desean quedar embarazadas y opinan que la denegación de dicho tratamiento no se justifica éticamente. Percibieron los servicios de concepción asistida como una alternativa segura y eficaz a la concepción espontánea, y afirmaron que la sociedad tiene la obligación moral de proporcionar dichos servicios.
Several studies have focused on the reproductive options and desires of HIV positive women who face multiple challenges of disease management and vertical transmission during and after pregnancy.Citation1Citation2 Very little, however, is known about pregnancy decision-making of HIV negative women who are knowingly in relationships with an HIV positive partner, especially with regard to their perceived risk of seroconversion and their desire to conceive their own biological children. These couples may face difficult choices as they balance the risks of transmission associated with spontaneous conception with their desire to conceive.
Assisted reproduction for serodiscordant couples is increasingly recognised as a need by public health agencies globally.Citation3Citation4 In 2006, the World Health Organization noted that artificial reproduction techniques can significantly influence the prevention of HIV transmission among discordant couples where the woman is HIV positive. However, preventing male-to-female transmission is more complex when the woman is HIV negative since there is no risk-free method to ensure safe conception.Citation3 In the USA the need to establish guidelines for health care providers to help serodiscordant couples conceive safely has been well documented.Citation4 The US Centers for Disease Control and Prevention does not recommend insemination of HIV negative women with semen from men with HIV.Citation5 The only assisted conception offered to serodiscordant couples in the USA is based on in vitro fertilisation–intracytoplasmic sperm injection (IVF–ICSI).Citation6 This procedure minimises the risk of viral transmission but is primarily intended for infertility treatment, with its associated risks and low success rates.Citation7 Statements by professional organisations such as the American Society for Reproductive Medicine (2002) and the American College of Obstetrics and Gynecology (2004) show support for providing fertility services for HIV -1 serodiscordant couples.Citation8Citation9
In Italy, in 1987 the Italian ethics committee approved the provision of reproductive assistance services to HIV discordant couples with male seropositivity, as a means to reduce the risk of HIV transmission to the female partner. When the results of this initiative were published and indicated no cases of infection to the women, other centres in Europe started offering these services.Citation10Citation11
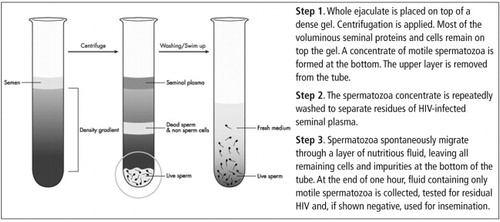
Risk-avoiding options, such as conception with donor sperm or adoption, may not be acceptable to many serodiscordant couples. Another option, which was adopted by the Italian initiative in 1987, is based on reducing the risk of viral transmission through sperm-washing followed by intrauterine insemination (SW+IUI).Citation10Citation11 This procedure uses timed intrauterine transfer of semen processed by a method that combines gradient centrifugation, washing and sperm migration, and has been available in Milan, Italy, since the 1989. This programme was offered to HIV discordant couples in the San Paolo hospital from 1989 to 1999. As of 1999, it ceased operating at the San Paolo hospital. Currently, two clinical centres, a public hospital and a private clinic in Milan, offer reproductive assistance services based on the programme developed in the San Paolo hospital. Patients entering the Milan programme after 1997 were tested for viral load prior to admission.Citation10Citation11
This paper presents findings from the formative evaluation phase of a retrospective follow-up study of HIV-discordant couples, conducted in Milan, Italy, who received assisted conception using SW+IUI in two public hospitals (including the original San Paolo hospital) and one private clinic. The initial cohort consisted of 811 women and their partners who were treated by either SW+IUI or by IVF–embryo transfer (ET) with processed semen provided by their HIV positive partner. As of 2006, 389 children have been born to 289 women.
In this formative study, we interviewed a sample of former patients who received treatment with SW+IUI about their need for, and satisfaction with, the procedure. The formative evaluation explored the reproductive choices, desires and intentions of patients who had sought treatment.
Methods
Patients were considered eligible if they were no longer currently enrolled in the assisted conception programme, had completed at least three insemination cycles or had participated in the programme for over a year. Patients from the rosters of two public hospitals and one private clinic in Milan meeting these eligibility criteria were then further screened based on distance from Milan and treatment outcomes. Seventy-one such patients were identified and were contacted by telephone by the study staff to gauge their interest in participating. Thirty-three of them (46%) agreed to participate.Footnote*
A female qualitative researcher (LH) met with the 33 participants who agreed to participate in the study office or in their homes. She described study objectives and procedures, obtained written informed consent and asked the participants to complete a baseline form to gather the following information: marital status, years of relationship, education, employment, mode of HIV transmission, immunological status of partner at time of first treatment, pregnancy history and treatment outcomes.
We conducted 22 face-to-face, semi-structured interviews in all, 11 with individual participants (six women, five men) and 11 with couples. The interviews, conducted by LH in Italian, lasted an average of two hours and included a series of open-ended questions with follow-up probes.Citation12–14 They explored four areas: i) HIV infection and the desire for children, including alternatives considered; ii) access to assisted conception programmes and the need for these services; iii) experience with the programme; and iv) impact of the programme on the couple’s relationship, quality of life and sexual risk behaviour.
Sessions were tape-recorded, transcribed and translated into English. Over 700 pages of transcripts were obtained. LH monitored the quality and variety of the information collected in the interviews, and stopped enrollment of participants after determining that saturation was achieved for all areas of interest.
Grounded theory guided the analysis.Citation15 First, two readers (SS, LH) independently reviewed the Italian transcripts and English translations to ensure consistency in translation. To gain familiarity with the text, interviews were read multiple times. These readings led to the initial identification of categories of data that were repeated across a range of respondents and revealed that many interviews diverged from the initial set of discussion topics. The interviewer kept detailed notes of her own on each transcript, including the reason for not obtaining information on some topics. In some instances, a topic was dropped from the interview guide after a few interviews because the topic was not relevant to the participants.
Two readers (SS, LH) selected five transcripts to evaluate the responses related to each topic listed in the interview guide. Comparisons were made across the five transcripts to identify patterns in the responses. The transcripts showed an emerging pattern that led to the identification of seven themes.
A single reader (SS) read the English translation of the remaining transcripts and prepared a summary containing information from the baseline form and salient themes and quotes from the interview. Four analysts (SS, LH, FO, MM) reviewed the summary sheets and reached consensus on the main findings. Quotes were abstracted from source transcripts to illustrate how participants addressed the main themes of the research.
The protocol for this study was reviewed and approved by the US Centers for Disease Control and Prevention Institutional Review Board and by the ethics board of the Azienda Sanitaria Locale (local health department) of the city of Milan.
Characteristics of the participants
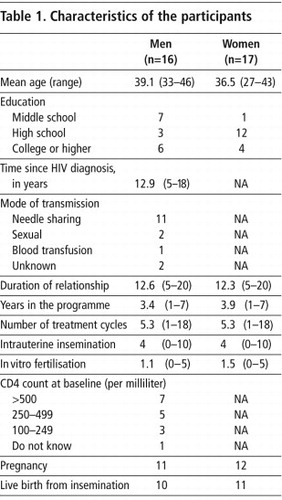
The mean age of the women was 36.5 years (range: 27–43) and 39.1 years among the men (range 33–46) (Table 1). The mean time since the men’s HIV diagnosis was 12.9 years and the most common mode of acquisition was intravenous drug use (11 of 16 men). All 33 participants were in a stable, long-term relationship and had spent an average of 3.4 years in the programme. Overall, 18 children were born to the participants in this study with no evidence of transmission to the HIV negative mother. One couple dropped out of the programme and conceived spontaneously. All the women reported that they and their infants were HIV seronegative at the time of the interviews.
In 17 of 22 interviews the woman said she knew about her partner’s HIV status at the beginning of the relationship. In the remaining five interviews, the men were diagnosed with HIV after the beginning of the relationship and the disclosure of HIV did not lead to its breakup.
Range of views expressed
Below, we describe the main issues and the range of views expressed.
• Desire for children
The desire for children grew with the knowledge that treatment existed, grew with improvement in HIV status of the male partner, diminished with treatment failure but persisted even when treatment failed. Participants’ decision to have a child was not influenced by friends and relatives. Participants described the desire for biologic children as a normal instinct which they often had to renounce because of HIV. Knowledge of the sperm-washing treatment rekindled this desire. Additionally, having a child provided a sense of “normalcy”, which was often lacking in their lives as a result of the disease.
“My dream has always been that of having kids. Later I met my husband and then I didn’t think about it anymore. When they told us about this centre I said, ‘Great, let’s try.’” (Patient A)
“Look, I believe that it’s the only thing, apart from the medicines that may pop up to cure this disease, I believe that it’s one of the few hopes that HIV-discordant couples can have. Because one says ‘Yes, I can have a kid, too, therefore, I’m not so different from the others.’” (Patient B)
• Perception of risk from treatment
Risk of infection to mother and child from insemination was of paramount importance. Some men were more concerned with transmission risks to their partners than to their unborn child. Some couples relied heavily on the “science” of treatment. Patients made their decisions based on chances of conception and low risks of HIV transmission. Most believed that assisted conception, although not risk free, provided a safer alternative to natural conception.
“The issues of risk were not in a second place… [they were] extremely important and in the very first place.” (Patient C)
“More than anything, I was interested in the fact that the child would be healthy. And the risk percentages were very, very low.” (Patient D)
• Conception through unprotected intercourse
Opinions about spontaneous conception varied widely among the participants. The responses included “would never consider”, “never considered before treatment but only after treatment failed” and “always considered spontaneous conception”. All but one were unwilling to try it. Most knew of serodiscordant couples who had conceived spontaneously without infecting mother or child.
“It’s not a disease that can be wished on anybody… least of all on my wife, or eventually on my son. I have always said to myself: ‘Well… the risk (spontaneous conception) is too big.’” (Patient E)
“I have never intended to play Russian roulette. Not on my own head and especially not on that of [my child].” (Patient C)
Only one couple that had previously conceived twice through spontaneous conception and spent four years in the programme without success reported having children by abandoning condom use. The man’s HIV viral load was low for two years, and they considered the risk worth taking. The woman noted:
“It was only to have a kid that we suspended. Our intercourse is always protected.” (Patient F)
• Alternatives to assisted conception
Many would have considered adoption but perceived the process as discriminatory against people with HIV.
“Because when the relationship with my husband started, I said ‘OK, I fell in love with him, then I have to give this up [children]’. I said ‘Let’s try with the adoption’, but nobody gives kids to a person who is [HIV positive].” (Patient A)
“They are ridiculous… they would rather leave him in the orphanage but they will never give him to you.” (Patient G)
Sperm donation as an option was less appealing to the women, who wanted their partner’s biologic child as an expression of love.
“My wife’s attachment to my genes surprised me a bit.” (Patient H)
“When we only started this process, he said: ‘Listen, but if we made this child without my sperm? Have a donation from someone else?’ He offered me this… And I was against it. I said ‘No, if we have a child I want him to be yours.’” (Patient I)
• HIV stigma
The effect of HIV stigma on the decision to have children emerged during the interviews. Rarely did anybody outside the family know about the man’s HIV-positive status. They could not share the difficulties of infertility treatment because of HIV.
“We can’t speak about it. At least not about the reason why we do it. Because it is something nobody knows. So it is difficult to speak. Therefore, from the point of view of emotional fragility, HIV-discordant couples are couples with more difficulties than others.” (Patient B)
Participants were very concerned about protecting their children from the stigma associated with HIV.
“In the family only my mother-in-law basically knows it and nobody else. And we were afraid, not for me or for my husband. I was afraid that then after this kid, my son would be isolated. And we continued to keep this thing because, as I said, my son is 11 years old and he doesn’t know it… Only to protect him. Not for me, nor my husband. Only the child.” (Patient F)
Difficulty existed even with disclosure to family members.
“My parents don’t know anything about my husband. Nobody knows about his HIV status because most people still fear it.” (Patient D)
“We live in a small town… they see it precisely as the worst thing.” (Patient G)
• Psychological impact of the treatment
The program’s psychological impact varied according to the outcome of the treatment (success or failure) and by personal experience (duration of the programme, logistics, costs and quality of services). Most patients stressed the need for counselling before and during treatment. The first cycle was associated with the highest expectations.
“I approached this thing convinced that the first time would be decisive… The reality is different because the majority of couples have to try at least three or four times.” (Patient B)
Women described their lives as being driven by their menstrual cycles.
“When the cycle arrives, and when it doesn’t arrive. Everything is marked by the menstrual cycle and it destroys your soul because it is coming, it isn’t coming, it has come.” (Patient J)
The duration of participation in the programme also caused fatigue and stress in the participants.
“And then the time, time in my opinion is fundamental… we were at it for two years.” (Patient K)
The mechanical aspects of assisted conception were often represented as the main reason for dropping out.
“Doing it on the gynaecologists’ bed is something manipulated… Then I’d been manipulated enough… I was tired of these things.” (Patient F)
Describing the range of emotions after a failed cycle, a woman noted:
“We were already walking like pregnant women. Because we were already more than convinced that we had succeeded. So all these attitudes, such as ‘I can’t drink coffee, I can’t do sport, I don’t smoke’… absurd stuff. But for us we were already pregnant and that’s it. Then, clearly… waking up was horrible.” (Patient L)
Men felt responsible for the suffering (physical or emotional) of their partner.
“…You also feel a sense of guilt because you see how much your partner has to suffer… you feel you are the cause of great suffering.” (Patient J)
A woman commented on the impact on men:
“I think that they suffer more, more than we do. We may be the ones who endure more because it is to us that they do all these things. [But] because of everything, he is really suffering psychologically.” (Patient I)
When the outcome was positive, the effect on quality of life was remarkable.
“I think that this is the most beautiful thing that has happened to me (laughs), imagine the happiness, well, apart from ours also that of our parents, for my parents this is the first grandchild… to me it seems as if I’ve been living a dream… the impact on me is this miracle [his son].” (Patient M)
• Need to expand assisted conception services
Participants agreed there was an urgent need to let people know about the availability of these programmes, especially because there were so many young people living with HIV. They were strongly in favour of providing these services to more HIV-discordant couples.
“In my opinion, it’s an opportunity that should be given to everybody… I mean if there wasn’t a solution, you say that’s fine, one accepts what there is. But it’s not right to withhold something as important as procreation [from] people because they have a disease… you are a person like all others, therefore this big joy must not be [taken from] you … it’s fundamental, it has to be there.” (Patient N)
“To me [assisted conception] is fundamental… For the couples, they can live a normal life like everybody else.” (Patient O)
Even participants who had failed to conceive said this option was a “positive opportunity”.
“Otherwise there weren’t any alternatives.” (Patient E)
“I’m happy to have tried… If I had to go back, I would do exactly the same.” (Patient B)
Discussion
Previous research indicates that being HIV positive does not eliminate the desire to have children.Citation2,16–19 Some studies report that HIV-positive adults living in relative good health not only desire children but also have high expectations of having children in the future.Citation2,17,18 Nearly 30% of HIV-positive men and women in one large study in the USA desired to have children and, of these, nearly 70% of the women and 60% of the men actually expected to have more than one child in the future.Citation2 In another US study, the desire for children was greater in women who had no previous children.Citation1 Similar findings have been reported from other countries as well. In a Brazilian study of men and women living with HIV, parenthood desires were reported to be stronger in men than in women.Citation20 Many studies report that with the advent of potent antiretroviral therapy, the desire to have children has become more and more common in HIV serodiscordant couples where the male partner is HIV positive but the female partner is negative. A study in Spain reported that the desire to have children was very strong among serodiscordant couples, partly because having healthy children could help normalise their lives.Citation21 Similarly, a significant proportion of HIV affected individuals expressed a wish for parenthood in a Swiss cohort study.Citation22
In this study, the desire for children was strong in the selected group of serodiscordant couples who sought to have children through assisted conception. Having a child brought a sense of “normalcy” to their lives that was often lacking due to the burden of the disease and the stigma associated with HIV. They cited raising children as a way to bring purpose to their lives, which has also been seen in previous studies.Citation2,23,24. This reiterates previous findings that people with HIV want children so as to “leave something of themselves behind” or because children represent “normality”.Citation25Citation26 Participants wanted their own biologic children, although some were open to adoption. It should be noted that most believed, incorrectly, that adoption agencies would not allow serodiscordant couples to adopt children.Footnote*
To our knowledge, this is the only study to examine patients’ perceptions of risk from insemination with the washed sperm of the HIV positive male partner. Responses revealed general confidence in the safety of the procedure, as most participants perceived the risk to be low. It is unclear whether this perception of low risk was held before the patients entered the programme (possibly a result of reassurance by medical staff offering the treatment) or was a result of their actual experience with the programme. No seroconversions to HIV in infants were reported by the participants.
Studies suggest that HIV-discordant couples may not be consistent users of condoms and that they are often willing to practise unsafe sex to conceive.Citation18Citation24 In this study, only one couple actually reported attempting conception via unprotected sex, after treatment failed. Most couples in this study practised safer sex during treatment.
Most participants were in stable relationships. This finding contrasts with previous studies examining the effects of HIV-related stigma, which have often reported significant relationship problems in couples coping with HIV, particularly where the women were seronegative.Citation27Citation28 HIV-serodiscordant couples often face unique challenges managing emotional and sexual intimacy. It is possible that only stable couples participated in this programme and therefore are not representative of the population of serodiscordant couples.
Our study is one of the first to report the impact of assisted conception on quality of life among serodiscordant couples who did not have fertility problems but enrolled in the programme to reduce risks of HIV transmission. These couples reported psychological distress resulting from childlessness just like couples facing infertility.Citation29 In particular, the male partner reported feelings of self-blame for their childlessness.
Ethical issues surrounding assisted conception for couples with HIV have been intensely debated.Citation4 Whereas it seems unethical to withhold assisted conception options from serodiscordant couples who desire their own biological children, it is still unclear whether the risk of HIV transmission using assisted conception is sufficiently low to meet the imperative of “doing no harm.” In this study, regardless of treatment outcomes, women and their HIV-positive partners said that it was unethical to withhold these services from couples that wanted them or to discriminate against HIV-discordant couples seeking them. They generally perceived the risk of transmission associated with the treatment to be comparable to the risks they experienced in their daily life.
The proportion of serodiscordant couples with a male partner who is HIV positive in the HIV population is growing worldwide. In this study, most of the men were healthy and wanted children even after 12 or more years with HIV. Many serodiscordant couples express the right to have children as a fundamental right. To date, very few clinics outside of Europe offer sperm washing treatment. Currently, assisted conception programmes based on sperm washing and IUI–ART are available only in a few centres in Western Europe. Worldwide, the lack of treatment centres offering reproductive assistance to couples with HIV does not satisfy the needs of people living with HIV.Citation30
In conclusion, participants exhibited a strong desire for children and recommended increased provision of assisted conception services and safer alternatives to unprotected sex. Couples living with HIV said that society had a moral obligation to provide safe and effective alternatives to spontaneous conception. They argued that these options are not developing fast enough because of discrimination against people with HIV.
Acknowledgements
Some of the results in this paper were presented in a poster session and as an extended abstract (Well-being and quality of life) at the XV International AIDS Conference, Bangkok, 11-16 July 2004. Abstract No. MoPeD3751. Support for this project (CSA-01-288) was provided by CONRAD, Contraceptive Research and Development Program, Eastern Virginia Medical School, under a Cooperative Agreement with the United States Agency for International Development (HRN-A-00-98-00020-00), which in turn receives funds for AIDS research from an inter-agency agreement with the Division of Reproductive Health, US Centers for Disease Control and Prevention. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of CONRAD, USAID or CDC.
Notes
* We were unable to trace some patients due to changes of address or phone number. Some declined to participate in face-to-face interviews. Reasons for refusal included lack of time, reluctance to discuss personal issues and recent partner death.
* In Italy, there are no official legal or policy barriers to adoption for couples with HIV. However, the participants did have negative experiences of trying to adopt, as expressed here.
References
- SB Kirshenbaum, EA Hirky, J Correale. “Throwing the dice”: pregnancy decision-making among HIV-positive women in four US cities. Perspectives on Sexual and Reproductive Health. 36: 2004; 106–113.
- JL Chen, KA Philips, DE Kanouse. Fertility desires and intentions of HIV-positive men and women. Family Planning Perspectives. 33: 2001. 144–52/165.
- World Health Organization. Sexual and Reproductive Health of Women Living with HIV/AIDS. December 2006.
- KA Bendikson, D Anderson, MD Hornstein. Fertility options for HIV patients. Current Opinion in Obstetrics & Gynecology. 14: 2002; 453–457.
- US Centers for Disease Control. Revised guidelines for HIV counseling, testing, and referral. Morbidity and Mortality Weekly Report. Recommendations and Reports. 50(RR-19): 2001; 1–57.
- MC Chu, JE Pena, MH Thornton. Assessing the treatment efficacy of IVF with intracytoplasmic sperm injection in human immunodeficiency virus-1 (HIV-1) serodiscordant couples. Reproductive Biomedicine Online. 10: 2005; 130–134.
- A Duerr, DJ Jamieson. Assisted reproductive technologies for HIV-discordant couples. American Journal of Bioethics. 3: 2003; 45–47.
- Ethics Committee American Society for Reproductive Medicine. Human immunodeficiency virus and infertility treatment. Fertility and Sterility. 7: 2002; 218–222.
- Committee on Ethics American College of Obstetricians and Gynecologists. Ethics in Obstetrics and Gynecology. 2nd ed., 2004; ACOG: Washington DC.
- AE Semprini, P Levi-Setti, M Bozzo. Insemination of HIV-negative women with processed semen of HIV-positive partners. Lancet. 340: 1992; 1317–1319.
- AE Semprini. Insemination of HIV-negative women with processed semen of HIV-positive partners. Lancet. 341: 1993; 1343–1344.
- M Agar. Ethnography in the streets and in the joint. R Weppner. Street Ethnography: Selected Studies of Crime and Drug Use in Natural Settings. 1977; Sage Publications: Beverly Hills CA, 143–156.
- M Agar. The Professional Stranger: An Informal Introduction to Ethnography. 1980; Academic Press: New York.
- M Agar. Speaking of Ethnography. 1986; Sage Publications: Beverly Hills CA.
- B Glaser, A Strauss. The Discovery of Grounded Theory: Strategies for Qualitative Research. 1967; Aldine: Chicago.
- MV Sauer, PL Chang. Establishing a clinical program for human immunodeficiency virus 1-seropositive men to father seronegative children by means of in vitro fertilization with intracytoplasmic sperm injection. American Journal of Obstetrics and Gynecology. 186: 2002; 627–633.
- MV Sauer. American physicians remain slow to embrace the reproductive needs of human immunodeficiency virus-infected patients. Fertility and Sterility. 85: 2006; 295–297.
- J Klein, JE Pena, MH Thornton. Understanding the motivations, concerns, and desires of human immunodeficiency virus 1-serodiscordant couples wishing to have children through assisted reproduction. Obstetrics and Gynecology. 101: 2003; 987–994.
- N De Van Devanter, PD Cleary, J Moore. Reproductive behavior in HIV-discordant heterosexual couples: implications for counseling. AIDS Patient Care and STDS. 12: 1998; 43–49.
- V Paiva, EV Filipe, N Santos. The right to love: the desire for parenthood among men living with HIV. Reproductive Health Matters. 11(22): 2003; 91–100.
- O Coll, R Vidal, T Martinez. Management of HIV serodiscordant couples. The clinician’s point of view. Contraception, Fertilité, Sexualité. 27: 1999; 399–404.
- L Panozzo, M Battegay, A Friedl. High risk behaviour and fertility desires among heterosexual HIV-positive patients with a serodiscordant partner – two challenging issues. Swiss Medical Weekly. 133: 2003; 124–127.
- J White, D Mevin, C Moore. Parental HIV discordancy and its impact on the family. AIDS Care. 9: 1997; 609–615.
- AC Thornton, F Romanelli, JD Collins. Reproduction decision making for couples affected by HIV: a review of the literature. Topics in HIV Medicine. 12: 2004; 61–67.
- D Cooper, H Bracken, L Myer. Reproductive intentions and choices among HIV-infected individuals in Cape Town, South Africa: lessons for reproductive policy and service provision from a qualitative study. September. 2005; Women’s Health Research Unit, Infectious Diseases Epidemiology Unit, University of Cape Town, School of Public Health & Family Medicine, Population Council: New York City.
- S Gruskin, L Ferguson, J O’Malley. Ensuring sexual and reproductive health for people living with HIV: an overview of key human rights, policy and health systems issues. Reproductive Health Matters. 15(29 Suppl): 2007; 4–26.
- A Van der Straten, KA Vernon, KR Knight. Managing HIV among serodiscordant heterosexual couples: serostatus, stigma and sex. AIDS Care. 10: 1998; 533–548.
- NL Beckerman. Couples coping with discordant HIV status. AIDS Patient Care and STDs. 6: 2002; 55–59.
- TM Cousineau, AD Domar. Psychological impact of infertility. Best Practice & Research Clinical Obstetrics and Gynaecology. 20: 2007; 1–16.
- L Bujan, L Hollander, M Coudert. Safety and efficacy of sperm washing in HIV-1-serodiscordant couples where the male is infected:results from the European CREAThE network. AIDS. 21: 2007; 1909–1914.