Abstract
During the last few decades, the use of ultrasonography for the detection of fetal abnormalities has become widespread in many industrialised countries. This resulted in a shift in timing of the diagnosis of congenital abnormalities in infants from the neonatal period to the prenatal period. This has major implications for both clinicians and the couples involved. In case of ultrasound diagnosis of fetal anomaly there are several options for the obstetric management, ranging from standard care to non-aggressive care to termination of pregnancy. This essay explores the context of both clinical and parental decision-making after ultrasound diagnosis of fetal abnormality, with emphasis on the Dutch situation. While normal findings at ultrasound examination have strong beneficial psychological effects on the pregnant woman and her partner, the couple are often ill-prepared for bad news about the health of their unborn child in the case of abnormal findings. When parents consider end-of-life decisions, they experience both ambivalent and emotional feelings. On the one hand, they are committed to their pregnancy; on the other hand, they want to protect their child, themselves and the family from the burden of severe disability. These complex parental reactions have implications for the counselling strategy.
Résumé
Ces dernières décennies, l'utilisation des ultrasons pour dépister les anomalies fłtales s'est généralisée dans beaucoup de pays industrialisés. Par conséquent, les anomalies congénitales ne sont plus diagnostiquées pendant la période néonatale, mais pendant la période prénatale. Ce changement a des conséquences majeures pour les cliniciens et les couples concernés. En cas de diagnostic par échographie d'une anomalie fłtale, plusieurs options existent pour la prise en charge obstétricale, depuis des soins standard jusqu'à des soins non agressifs et l'interruption de la grossesse. Cet essai étudie le contexte de la prise de décision clinique et parentale après le diagnostic par ultrasons d'une anomalie fłtale, en se centrant sur la situation néerlandaise. Alors que les examens échographiques normaux ont des effets psychologiques fortement positifs sur la femme enceinte et son partenaire, le couple est souvent mal préparé aux mauvaises nouvelles sur la santé de l'enfant à naître. Quand les parents envisagent une décision de fin de vie, ils éprouvent des sentiments ambivalents et émotionnels. D'une part, ils tiennent à cette grossesse, mais de l'autre, ils veulent protéger leur enfant, eux-mêmes et la famille du fardeau d'un handicap grave. Ces réactions parentales complexes ont des répercussions sur la stratégie de conseil.
Resumen
Durante las últimas décadas, el uso de la ultrasonografía para la detección de anormalidades fetales se ha extendido en muchos países industrializados. Esto propició un cambio en el momento oportuno para el diagnóstico de anormalidades congénitas en bebés desde el período neonatal hasta el prenatal, lo cual presenta importantes implicaciones tanto para los profesionales médicos como para las parejas. En el caso de diagnóstico por ultrasonido de la anomalía fetal, existen varias opciones para el manejo obstétrico: desde la atención estándar hasta la atención no agresiva y la interrupción del embarazo. En este ensayo se explora el contexto de la toma de decisiones tanto de los profesionales médicos como de los padres después del diagnóstico por ultrasonido de la anormalidad fetal, con énfasis en la situación holandesa. Aunque los hallazgos normales en el examen por ultrasonido tienen importantes efectos psicológicos benéficos para la mujer embarazada y su pareja, a menudo los padres no están bien preparados para recibir malas noticias sobre la salud de su niño no nato en el caso de resultados anormales. Al considerar la decisión de terminar una vida, sienten tanto ambivalencia como diferentes emociones. Por un lado, están comprometidos a su embarazo; por otro lado, quieren proteger a su hijo, a sí mismos y a su familia de la carga de una discapacidad grave. Estas complejas reacciones de los padres tienen implicaciones para la estrategia de consejería.
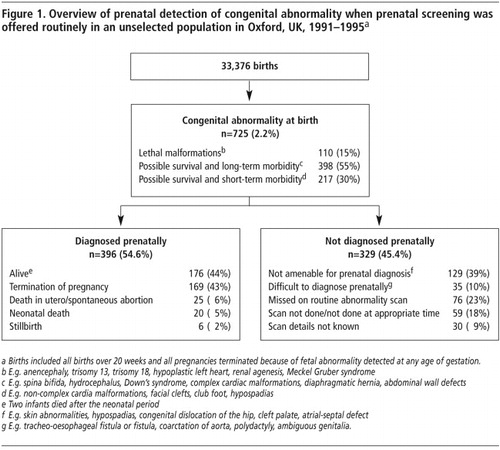
Congenital abnormalities are the main cause of infant death in industrialised countries.Citation1Citation2 Congenital abnormalities are frequently diagnosed before birth, as many of the major fetal abnormalities can be detected by a prenatal ultrasound examination.Citation3–5 From data derived from a routine ultrasound screening setting of an unselected population in Oxford,Citation6 the estimated birth prevalence of infants with abnormalities is 2.2% (). Just over half (55%) of them were diagnosed with abnormalities that were identified prenatally. Currently, ultrasound scanning is considered the most important tool for prenatal diagnosis of fetal congenital abnormalities. It detects the majority but certainly not all of the fetal abnormalities.Citation6 In specialist centres for prenatal diagnosis detection rates of fetal abnormalities range from 80% to 95%.Citation4Citation7 Detection rates in screening settings are probably lower. The detection rates also depend on the nature, type and numbers of abnormalities. For example, prenatal detection rates of neural tube defects approximate 98% while those of congenital heart defects are about 38%. Apart from the nature of the fetal abnormality, maternal obesity has a considerable impact on detection rates.Citation8
The study in Oxford also addressed the overall impact of prenatal ultrasound diagnosis in terms of numbers of infants born with conditions that result in mortality or severe morbidity ().Citation6 In fact, when severe congenital abnormalities are detected prenatally, termination of pregnancy is an option for the couple involved. In the majority of end-of-life decisions in the prenatal period, suspicion of fetal abnormality was first aroused after ultrasound scan.Citation6 Hence, the practice of ultrasound scanning is closely related to that of end-of-life-decisions.
Developments in fetal ultrasound
Since the early 1960s, when the first ultrasound images of the fetus were made, ultrasound has evolved into the most important diagnostic tool in fetal medicine.Citation9 First, only static images of the fetus were available. In 1977 real-time scanning was introduced, which allowed for moving images of the fetus. Soon thereafter, ultrasound became widely available in clinical practice. In a short period of time a myriad of reports on both normal and abnormal anatomy of the fetus appeared in the medical literature. Nowadays, routine ultrasound examination during pregnancy is an integral part of prenatal care in most industrialised countries.Citation9–11 Routine ultrasound examination typically includes a dating scan in the first trimester of pregnancy and a fetal abnormality scan at approximately 18 to 20 weeks' gestation.Citation9
In countries with a routine ultrasound screening policy, more than half of all congenital abnormalities are diagnosed prenatally, including 74% of the major abnormalities (i.e. abnormalities that have implications for the infant's health) and 46% of the minor abnormalities (i.e. abnormalities that have no implications for the infant's health).Citation6,12
Ultrasound screening
From the perspective of public health, the potential benefits and limitations of ultrasound screening for fetal abnormalities have been debated extensively.Citation4Citation9 To date, reports on the benefits of ultrasound screening for the detection of both lethal and non-lethal abnormalities among unselected populations are inconclusive.Citation13 Randomised controlled trials have been done, but have used perinatal mortality and morbidity as outcome variables. Moreover, in research settings there was a wide variation in expertise levels of sonographers. The interpretation of the research findings is further impeded by the time period of the studies being conducted: ultrasound nowadays is more advanced than in former days.Citation10 These methodological problems are reflected in an enormous variation of reported overall sensitivity of the detection of congenital abnormalities, which ranges between 14% and 96%.Citation3–5,13 Apart from these methodological flaws, the use of perinatal mortality and morbidity as the most important outcome variables is questionable.Citation10 Other outcome variables, such as improved information of pregnant women about the health status of their offspring, enhanced care for the affected neonate, better fetal–maternal bonding, and the potential prevention of a “wrongful life” are relevant as well.Citation13 These issues warrant additional questions about the aims of screening. The answer to these questions should not only pertain to medical data, but should also incorporate moral choices.Citation10,11,14
In the Netherlands, the implementation of ultrasound screening into clinical practice has been a matter of strong debate.Citation11 Initially, the government decided that ultrasound is only to be offered for “genetic” indications, i.e. targeted at women at increased risk of congenital abnormalities in offspring.Citation11 This policy should be seen within the Dutch sociocultural context. Dutch law typically bans population screening, unless certain conditions are fulfilled, such as the availability of effective treatment for the outcome of interest.Citation11 In the context of prenatal screening for fetal abnormalities, abortion is not considered as an “effective” modality. Furthermore, there were concerns about the implications of prenatal screening in terms of medicalisation of the pregnancy and regarding the position of handicapped people in the society at large.Citation11 Only recently, Dutch law became more compliant, which resulted in a trend towards offering all pregnant women an ultrasound examination at 20 weeks' gestation.
The government's initial decision not to incorporate routine ultrasound screening into clinical practice resulted in large practice variations, i.e. some women having no ultrasound examination at all, while others having a two-scan policy or a “pleasure scan” in a commercial setting. The latter may give false reassurance as these ultrasound examinations are not intended for the detection of fetal abnormalities.Citation11Citation15 Until recently, there were neither formal guidelines for the timing of the ultrasound and counselling nor for qualifications of sonographers. So even if women have had one or multiple ultrasound examinations, potentially detectable major fetal abnormalities have still been missed.
Psychological effects of normal ultrasound
Normal findings at ultrasound examination have strong beneficial psychological effects on the pregnant woman and her partner. For couples, ultrasound is a way of “meeting” the unborn child.Citation16–19 The personalisation of the fetus enhances both maternal–fetal bonding and bonding of the pregnant woman and her partner.Citation18,20,21 A normal ultrasound also reassures parents about their pregnancies.Citation20,22–25 The positive effects of ultrasound are stronger when more feedback is provided, such as showing images on an additional monitor, and explaining what can be seen.Citation20Citation24
In fact, fetal ultrasound is highly appreciated by pregnant women and their partners.Citation19,25–27 Most women consider ultrasound examinations as an integral part of prenatal care.Citation26 However, frequently women lack information about the purpose of ultrasound examinations and their technical limitations. As a result, women are often unprepared for adverse findings.Citation27Citation28
Psychological effects of abnormal ultrasound
The news of abnormal findings of the ultrasound examination frequently comes unexpectedly and is often intensely shocking for the would-be parents, in particular when major congenital abnormalities are encountered.Citation27Citation29 Pregnant women and their partners may have several emotional reactions when fetal abnormalities are revealed. Firstly, they may have negative feelings typically associated with psychological trauma in general, such as anxiety, grief, anger, loneliness, hopelessness, prostration and guilt.Citation28–33 These feelings may be aggravated by the loss of the imagined future, as the pregnancy may end in the daily reality of having no child or a severely handicapped child, requiring readjustments by the entire family. These negative feelings can be enhanced by the confrontation with reality, when having to decide about very pragmatic issues “Should I furnish the nursery?”, “Should I make arrangements for the funeral?”, and “What should I tell my other child?”. Finally, some parents experience a loss of reference. The news of a fetal abnormality in an apparently uneventful pregnancy usually comes so unexpectedly, and is in such contrast with the pleasant experiences that often go along with a much wanted pregnancy, that parents have severe difficulty grasping the facts. It seems so unreal that the child, who is kicking inside the womb, is severely disabled and will perhaps die, thereby making life meaningless. When parents consider pregnancy termination, the ambivalent feelings they experience may enhance this loss of reference. On the one hand, they are committed to their – desired and intended – pregnancy, while on the other hand, they want to protect their child, themselves and their family from the burden of severe disability.Citation34
End-of-life-decisions after ultrasound diagnosis of fetal abnormality
With the burgeoning of ultrasound, questions around the appropriate obstetric management in case of sonographically-established fetal abnormalities have arisen. Should we apply every means possible to keep a fetus with a very poor prognosis alive? Do medical professionals in the field of perinatal medicine agree on fetal prognosis after ultrasound diagnosis of fetal abnormality? How should obstetric and neonatal management be attuned? How do parents view end-of-life decisions concerning their unborn infant? These and other issues have opened a new field of research: end-of-life decision-making after ultrasound diagnosis of fetal abnormality. End-of-life decisions are decisions about medical interventions at the end of life, which certainly or probably hasten death.Citation35
Two kinds of end-of-life decisions can be distinguished after ultrasound diagnosis of fetal abnormality: 1) non-aggressive obstetric management and 2) termination of pregnancy. Non-aggressive obstetric management refers to obstetric management in which interventions needed to sustain fetal life are forgone because of the poor prognosis of the fetus concerned. Chervenak and McCullough first reported the non-aggresive obstetric management approach in 1989.Citation36 They described 13 cases where such an approach was adopted. They regarded non-aggressive obstetric management as permissible, and even preferable, when there is certainty of death or absence of cognitive developmental capacity as an outcome of the congenital abnormality. They argued that in such cases the fetus does not benefit from obstetric intervention, while such intervention may harm the pregnant woman and interfere with her autonomy.Citation36Citation37 However, empirical data needed for a balanced professional and societal debate about forgoing fetal life-sustaining treatment are scarce.Citation36,38,39
Termination of pregnancy is a management option in which the pregnancy is terminated with the explicit intention of hastening fetal death. Termination of pregnancy is done by induction of labour, which may be preceded by fetal intra-cardial potassium injection. The first termination of pregnancy after ultrasound diagnosis of fetal abnormality was reported in 1972 by Campbell et al.Citation40 Their report concerned a fetus with anencephaly. Termination of pregnancy has far-reaching implications for the couple. It has lasting consequences and evokes strong emotions in the couples involved.Citation41Citation42
End-of-life decision-making after ultrasound diagnosis of fetal abnormality must take into account both the interests of the fetus and the pregnant woman. Therefore, these difficult decisions are usually made by a multidisciplinary team. These typically consist of obstetricians, neonatologists, paediatric surgeons and other paediatric specialists, such as paediatric urologists, paediatric neurologists and paediatric neurosurgeons.Citation43–47 However, little is known about how exactly decisions are being taken in these teams.
Parental decision-making after ultrasound diagnosis of fetal abnormality also remains a largely unknown territory. Studies to date that have evaluated determinants of parental decisions regarding termination of pregnancy have found that low gestational age, severe abnormality, involvement of the central nervous system, previous uncompleted pregnancies, low maternal educational level and the presence of chromosomal abnormalities are associated with high rates of women deciding for termination of pregnancy.Citation48–51 However, these data are not conclusive and do not reflect why and in what way some factors are important for the parents. Sandelowski studied parental decision-making concerning prenatal diagnosis of fetal abnormality in more depth. She interviewed 15 women and 12 of their partners. Her study showed that women have highly variable perceptions of choice. In fact, women in comparable circumstances feel differently about whether or not they have a choice about the future of their pregnancy.Citation52
Legal context and current guidelines
In the Netherlands, the law prohibits termination of pregnancy at a gestational age of 24 weeks or beyond. However, in cases where it is considered good clinical practice, physicians will not be prosecuted.Citation53–55 Good clinical practice is described in guidelines that were made by a collaborative group of the Ministry of Health, Ministry of Justice and the Dutch Society of Obstetricians and Gynaecologists. According to these guidelines, when parents persist in their request for termination of pregnancy, this will be granted when fetal prognosis is considered lethal. Fetal prognosis is considered lethal if (1) the infant has no chance of survival and the abnormalities can not be treated or (2) the infant has a chance of extra-uterine survival but post-natal use of life-prolonging medical treatment is considered futile.Citation54
In conclusion
In most industrialised countries, ultrasonography for the detection of fetal abnormalities has become an integral part of prenatal care. In general, women are often ill-prepared for bad news about the health of their unborn child. It is crucial that, prior to the examination, women are provided with objective and balanced information about ultrasound screening, both in terms of its potential virtues and its limitations. In this context, ultrasound should not be regarded solely as an enjoyable technique to visualise the baby, but also as a method to detect fetal abnormalities. When an abnormality is detected, women and their partners are confronted with a number of dilemmas, including the decision whether or not to continue the pregnancy. Their perceptions of the options they have vary markedly among couples, which challenges the counselling strategy. Further research is required into individuals' valuations of the different outcomes that might accrue from participation or non-participation in ultrasound screening.
Acknowledgements
This paper, slightly revised and with a different concluding section, is reprinted from Bijma HH et al, Decision-making after ultrasound diagnosis of fetal abnormality. European Clinics in Obstetrics and Gynaecology 2007;3(2):89–95, with kind permission from Springer, who retain the copyright.
References
- J Petrini, K Damus, R Russell. Contribution of birth defects to infant mortality in the United States. Teratology. 66(Suppl 1): 2002; S3–S6.
- K Lee, B Khoshnood, L Chen. Infant mortality from congenital malformations in the United States, 1970–1997. Obstetrics and Gynecology. 98: 2001; 620–627.
- F Lys, P De Wals, I Borlee-Grimee. Evaluation of routine ultrasound examination for the prenatal diagnosis of malformation. European Journal of Obstetrics, Gynecology and Reproductive Biology. 30: 1989; 101–109.
- S Levi. Ultrasound in prenatal diagnosis: polemics around routine ultrasound screening for second trimester fetal malformations. Prenatal Diagnosis. 22: 2002; 285–295.
- JM Carrera, M Torrents, C Mortera. Routine prenatal ultrasound screening for fetal abnormalities: 22 years' experience. Ultrasound in Obstetrics and Gynecology. 5: 1995; 174–179.
- PA Boyd, P Chamberlain, NR Hicks. 6-year experience of prenatal diagnosis in an unselected population in Oxford, UK. Lancet. 352: 1998; 1577–1581.
- JW Wladimiroff, TE Cohen-Overbeek, NT Ursem. Geavanceerd ultrageluidonderzoek naar aangeboren afwijkingen in Rotterdam; 20 jaar ervaring. [Twenty years of experience in advanced ultrasound scanning for fetal abnormalities in Rotterdam]. Nederlands Tijdschrift voor Geneeskunde. 147: 2003; 2106–2110.
- A Tabor, M Zdravkovic, A Perslev. Screening for congenital malformations by ultrasonography in the general population of pregnant women: factors affecting the efficacy. Acta Obstetricia et Gynecologica Scandinavica. 82: 2003; 1092–1098.
- MB McNay, JE Fleming. Forty years of obstetric ultrasound 1957–1997: from A-scope to three dimensions. Ultrasound in Medicine and Biology. 25: 1999; 3–56.
- PS Romano, NJ Waitzman. Can decision analysis help us decide whether ultrasound screening for fetal abnormalities is worth it?. Annals of the New York Academy of Science. 847: 1998; 154–172.
- Health Council of the Netherlands. Prenatal Screening: Down's syndrome, neural tube defects, routine-ultrasonography. No.2001/11. 2001; Health Council of the Netherlands: Den Haag.
- H Grandjean, D Larroque, S Levi. Sensitivity of routine ultrasound screening of pregnancies in the Eurofetus database. The Eurofetus Team. Annals of the New York Academy of Science. 847: 1998; 118–124.
- JW Wladimiroff. Routine ultrasonography for the detection of fetal structural anomalies. HIJ Wildschut, CP Weiner, TJ Peters. When to Screen in Obstetrics and Gynecology. 2nd ed., 2006; WB Saunders: Philadelphia, 244–252.
- L Getz, AL Kirkengen. Ultrasound screening in pregnancy: advancing technology, soft markers for fetal chromosomal aberrations, and unacknowledged ethical dilemmas. Social Sciences and Medicine. 56: 2003; 2045–2057.
- HIJ Wildschut, P ten Hoope-Bender, M Borkent-Polet. Practice variation of test procedures reportedly used in routine antenatal care in the Netherlands. Acta Obstetricia et Gynecologica Scandinavica. 78: 1999; 27–32.
- JE Puddifoot, MP Johnson. The legitimacy of grieving: the partner's experience at miscarriage. Social Science and Medicine. 45: 1997; 837–845.
- I Kowalcek, G Huber, I Bieniakiewitz. The influence of gestational age on depressive reactions, stress and anxiety of pregnant women and their partners in relation to prenatal diagnosis. Journal of Psychosomatic Obstetrics and Gynaecology. 24: 2003; 239–245.
- L Bricker, J Garcia, J Henderson. Ultrasound screening in pregnancy: a systematic review of the clinical effectiveness, cost-effectiveness and women's views. Health Technology Assessment. 4: 2000. i-vi/1–193.
- G Harris, L Connor, A Bisits. “Seeing the baby”: pleasures and dilemmas of ultrasound technologies for primiparous Australian women. Medical Anthropology Quarterly. 18: 2004; 23–47.
- AE Reading, DN Cox. The effects of ultrasound examination on maternal anxiety levels. Journal of Behavioral Medicine. 5: 1982; 237–247.
- M Sklansky, A Tang, D Levy. Maternal psychological impact of fetal echocardiography. Journal of American Society of Echocardiography. 15: 2002; 159–166.
- CE Harris. Aborting abnormal fetuses: the parental perspective. Journal of Applied Philosophy. 8: 1991; 57–68.
- G Bjorkhem, C Jorgensen, K Hanseus. Parental reactions to fetal echocardiography. Journal of Maternal and Fetal Medicine. 6: 1997; 87–92.
- Z Zlotogorski, O Tadmor, E Duniec. The effect of the amount of feedback on anxiety levels during ultrasound scanning. Journal of Clinical Ultrasound. 24: 1996; 21–24.
- T Larsen, TH Nguyen, M Munk. Ultrasound screening in the 2nd trimester. The pregnant woman's background knowledge, expectations, experiences and acceptances. Ultrasound in Obstetrics and Gynecology. 15: 2002; 383–386.
- E Georges. Fetal ultrasound imaging and the production of authoritative knowledge in Greece. Medical Anthropology Quarterly. 10: 1996; 157–175.
- J Garcia, L Bricker, J Henderson. Women's views of pregnancy ultrasound: a systematic review. Birth. 29: 2002; 225–250.
- H Statham, W Solomou, L Chitty. Prenatal diagnosis of fetal abnormality: psychological effects on women in low-risk pregnancies. Baillières Best Practice and Research in Clinical Obstetrics and Gynaecology. 14: 2000; 731–747.
- JJ Detraux, F Gillot-de Vries, S Vanden Eynde. Psychological impact of the announcement of a fetal abnormality on pregnant women and on professionals. Annals of the New York Academy of Science. 847: 1998; 210–219.
- JA Hunfeld, JW Wladimiroff, J Passchier. Emotional reactions in women in late pregnancy (24 weeks or longer) following the ultrasound diagnosis of a severe or lethal fetal malformation. Prenatal Diagnosis. 13: 1993; 603–612.
- M Langer, M Ringler. Prospective counselling after prenatal diagnosis of fetal malformations: interventions and parental reactions. Acta Obstetricia et Gynecologica Scandinavica. 68: 1989; 323–329.
- SR Leuthner, M Bolger, M Frommelt. The impact of abnormal fetal echocardiography on expectant parents' experience of pregnancy: a pilot study. Journal of Psychosomatic Obstetrics and Gynaecology. 24: 2003; 121–129.
- LM Mitchell. Women's experiences of unexpected ultrasound findings. Journal of Midwifery and Women's Health. 49: 2004; 228–234.
- DW Britt, ST Risinger, MK Mans. Devastation and relief: conflicting meanings of detected fetal abnormalities. Ultrasound in Obstetrics and Gynecology. 20: 2002; 1–5.
- JH Groenewoud. End-of-life-decisions in medicine, empirical studies on practices and attitudes in the Netherlands. 2002; Erasmus University Medical Centre Rotterdam: Rotterdam.
- FA Chervenak, LB McCullough. Nonaggressive obstetric management. An option for some fetal abnormalities during the third trimester. JAMA. 261: 1989; 3439–3440.
- FA Chervenak, LB McCullough, D Skupski. Ethical issues in the management of pregnancies complicated by fetal abnormalities. Obstetrical and Gynecological Survey. 58: 2003; 473–483.
- P Kirkinen, P Jouppila, R Herva. Fatal fetal abnormalities. Route of delivery and effect of the development of antepartum diagnostics in the last 13 years. Journal of Reproductive Medicine. 37: 1992; 645–668.
- JA Spinnato, VD Cook, CR Cook. Aggressive intrapartum management of lethal fetal abnormalities: beyond fetal beneficence. Obstetrics and Gynecology. 85: 1995; 89–92.
- S Campbell, FD Johnstone, EM Holt. Anencephaly: early ultrasonic diagnosis and active management. Lancet. 2: 1972; 1226–1227.
- MC White-Van Mourik, JM Connor. The psychosocial sequelae of a second trimester termination of pregnancy for fetal abnormality over a two year period. Birth Defects Original Article Series. 28: 1992; 61–74.
- MC White-Van Mourik, JM Connor, MA Ferguson-Smith. Patient care before and after termination of pregnancy for neural tube defects. Prenatal Diagnosis. 10: 1990; 497–505.
- TM Crombleholme, M D'Alton, M Cendron. Prenatal diagnosis and the pediatric surgeon: the impact of prenatal consultation on perinatal management. Journal of Pediatric Surgery. 31: 1996; 156–162.
- FI Luks, SR Carr, LR Feit. Experience with a multidisciplinary antenatal diagnosis and management model in fetal medicine. Journal of Maternal Fetal and Neonatal Medicine. 14: 2003; 333–337.
- L Aite, A Trucchi, A Nahom. Multidisciplinary management of fetal surgical abnormalities: the impact on maternal anxiety. European Journal of Pediatric Surgery. 12: 2002; 90–94.
- J Kemp, M Davenport, A Pernet. Antenatally diagnosed surgical abnormalities: the psychological effect of parental antenatal counseling. Journal of Pediatric Surgery. 33: 1998; 1376–1379.
- MS Scher, BM Kidder, D Shah. Pediatric neurology participation in a fetal diagnostic service. Pediatric Neurology. 30: 2004; 338–344.
- M Sandelowski, LC Jones. Healing fictions: stories of choosing in the aftermath of the detection of fetal abnormalities. Social Science and Medicine. 42: 1996; 353–361.
- JM Bosma, G van der Wal, SL Hosman-Benjaminse. Late zwangerschapsafbreking in Noord-Holland. II Zorgvuldigheid vooraf en toetsing achteraf [Late pregnancy interruption in Noord-Holland. II. Carefulness before and review afterwards]. Nederlands Tijdschrift voor Geneeskunde. 140: 1996; 605–609.
- Late zwangerschapsafbreking: zorgvuldigheid en toetsing. [Late termination of pregnancy: care and assessment]. 1998; Netherlands Ministry of Health/Ministry of Justice: Rijswijk.
- Nederlandse Vereniging voor Obstetrie en Gynaecologie. Model Reglement Medisch Handelen Late Zwangerschapsafbreking bij niet met het leven verenigbare afwijkingen vallend onder categorie 1; versie dd 221003. 2003.
- C Grevengood, LP Shulman, JS Dungan. Severity of abnormality influences decision to terminate pregnancies affected with fetal neural tube defects. Fetal Diagnosis and Therapy. 9: 1994; 273–277.
- PG Pryde, NB Isada, M Hallak. Determinants of parental decision to abort or continue after non-aneuploid ultrasound-detected fetal abnormalities. Obstetrics and Gynecology. 80: 1992; 52–56.
- E Sheiner, I Shoham-Vardi, D Weitzman. Decisions regarding pregnancy termination among Bedouin couples referred to third level ultrasound clinic. European Journal of Obstetrics & Gynecology and Reproductive Biology. 76: 1998; 141–146.
- KB Schechtman, DL Gray, JD Baty. Decision-making for termination of pregnancies with fetal abnormalities: analysis of 53,000 pregnancies. Obstetrics and Gynecology. 99: 2002; 216–222.